J Korean Assoc Oral Maxillofac Surg.
2024 Jun;50(3):146-152. 10.5125/jkaoms.2024.50.3.146.
Clinical outcome of perioperative airway and ventilatory management in patients undergoing surgery for oral cavity cancer: a prospective observational study
- Affiliations
-
- 1Department of Anaesthesiology and Critical Care, All India Institute of Medical Sciences, Bhopal, India
- KMID: 2557631
- DOI: http://doi.org/10.5125/jkaoms.2024.50.3.146
Abstract
Objectives
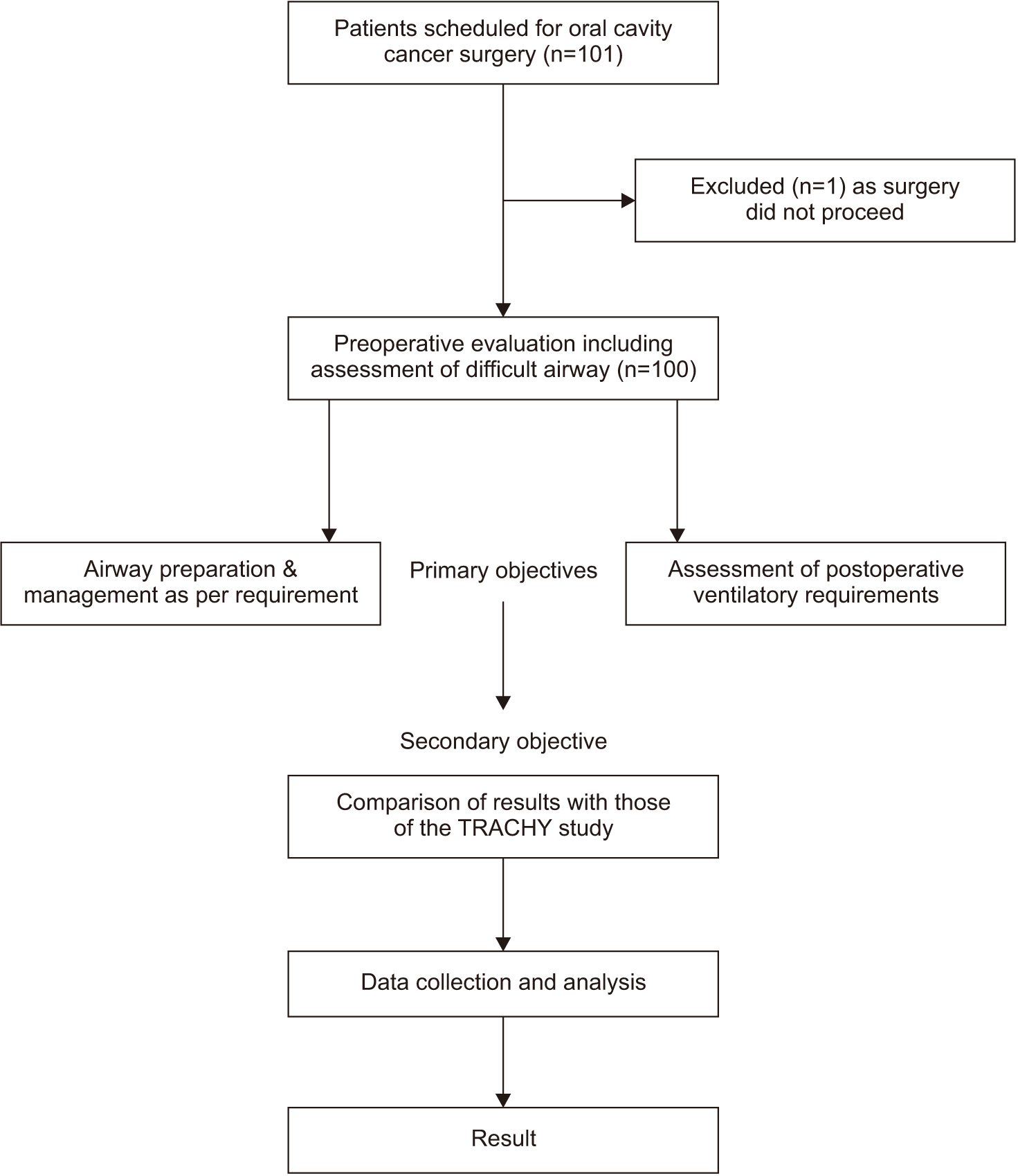
This prospective observational study aimed to assess the clinical outcomes of perioperative airway and ventilatory management in patients undergoing surgery for oral cavity cancer. The study described the frequencies and types of procedures for securing the airway and the duration and types of postoperative ventilatory support. We compared the findings with those of the TRACHY study.
Patients and Methods
One hundred patients undergoing oral cavity oncological surgeries were included. Airway assessment included inter-incisor gap, Mallampati class, neck movements, and radiological features. Surgical parameters, postoperative ventilatory support, and complications were documented.
Results
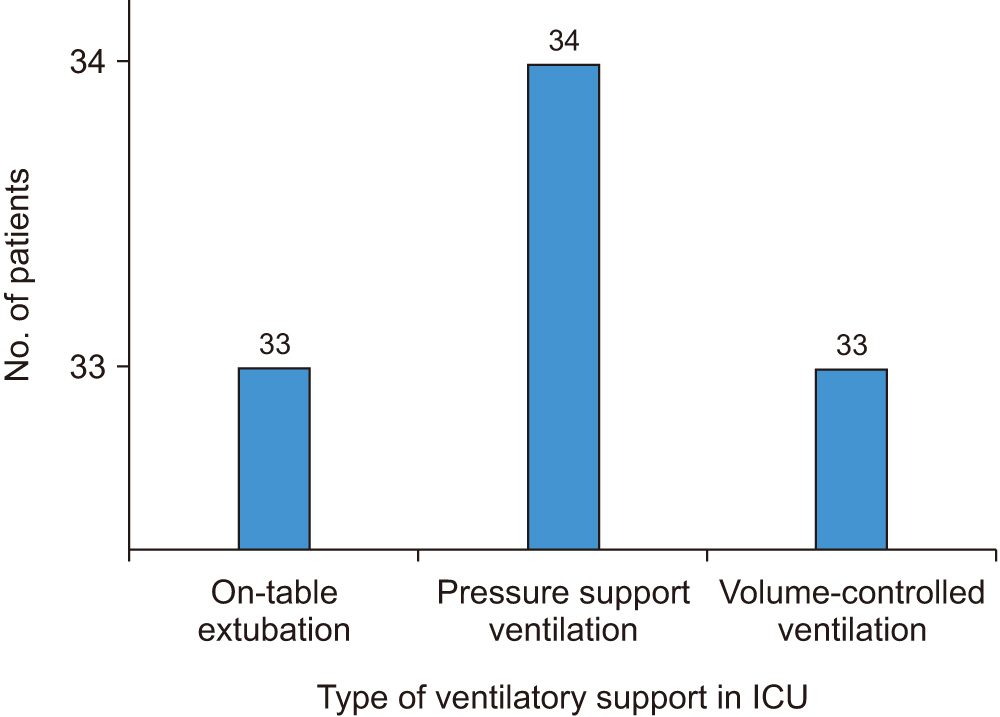
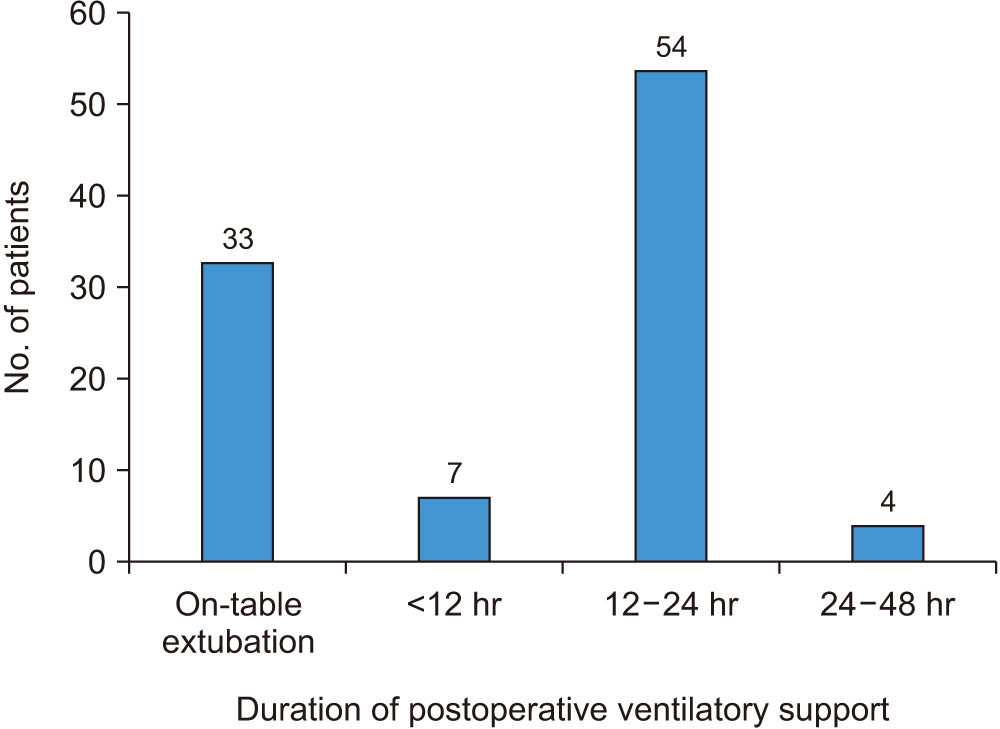
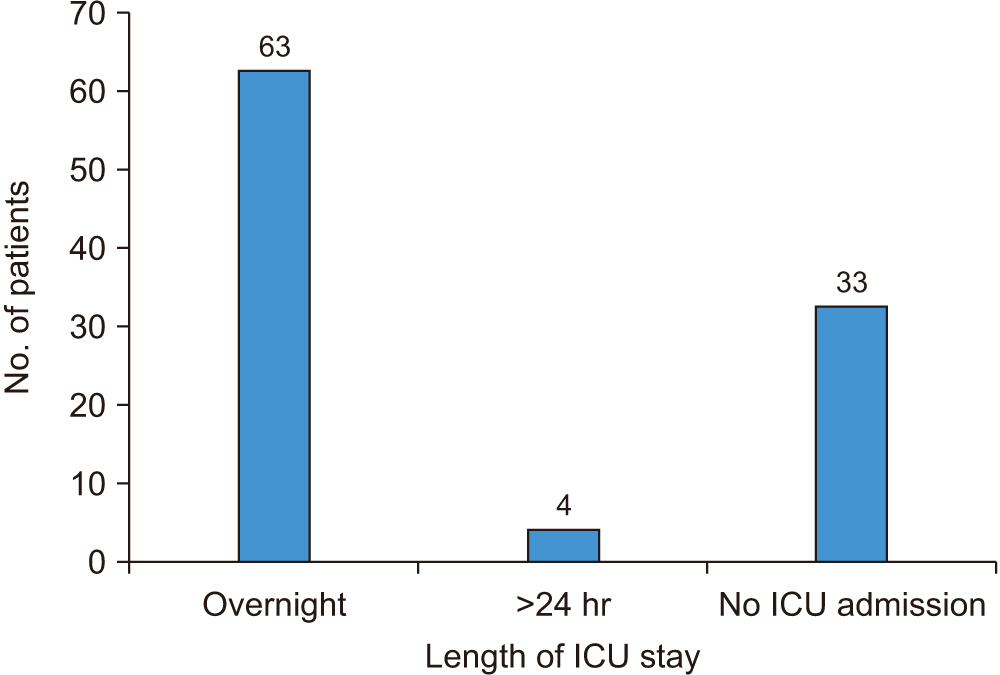
The buccal mucosa was the most common cancer site (48.0%), and direct laryngoscopy was deemed difficult in 58.0% of patients. Awake fibreoptic intubation or elective tracheostomy was required in 43.0% of cases. Thirty-three patients were extubated on the table, and 34 patients were successfully managed with a delayed extubation strategy. In comparison with the TRACHY study, variations were observed in demographic parameters, tumour characteristics, and surgical interventions. Our mean TRACHY score was 1.38, and only five patients had a score ≥4. Prophylactic tra-cheostomy was performed in 2.0% of cases, in contrast to the TRACHY study in which 42.0% of patients underwent the procedure.
Conclusion
The study emphasizes the challenges in airway management for oral cavity cancer surgery. While prophylactic tracheostomy may be necessary in specific cases, individualized approaches, including delayed extubation, are preferrable to maximize safety. Our findings contribute to better understanding and managing perioperative challenges in oral cancer patients and highlight the need for personalized strategies. Scoring systems like TRACHY should not be accepted as universally applicable.
Figure
Reference
-
References
1. Bedi RS, Pande G, Patel JS, Khan Z, Chauhan N. 2015; Oral cancer: a review. Eras J Med Res. 2:22–41.2. Dougherty TB, Nguyen DT. 1994; Anesthetic management of the patient scheduled for head and neck cancer surgery. J Clin Anesth. 6:74–82. https://doi.org/10.1016/0952-8180(94)90125-2. DOI: 10.1016/0952-8180(94)90125-2. PMID: 8142105.
Article3. Kruse-Lösler B, Langer E, Reich A, Joos U, Kleinheinz J. 2005; Score system for elective tracheotomy in major head and neck tumour surgery. Acta Anaesthesiol Scand. 49:654–9. https://doi.org/10.1111/j.1399-6576.2005.00655.x. DOI: 10.1111/j.1399-6576.2005.00655.x. PMID: 15836679.
Article4. Marsh M, Elliott S, Anand R, Brennan PA. 2009; Early postoperative care for free flap head & neck reconstructive surgery--a national survey of practice. Br J Oral Maxillofac Surg. 47:182–5. https://doi.org/10.1016/j.bjoms.2008.06.004. DOI: 10.1016/j.bjoms.2008.06.004. PMID: 18640751.
Article5. Madgar O, Livneh N, Dobriyan A, Dagan E, Alon EE. 2022; Airway management following head and neck microvascular reconstruction: is tracheostomy mandatory? Braz J Otorhinolaryngol. 88 Suppl 4:S44–9. https://doi.org/10.1016/j.bjorl.2021.07.007. DOI: 10.1016/j.bjorl.2021.07.007. PMID: 34756557. PMCID: PMC9756065.
Article6. Cameron M, Corner A, Diba A, Hankins M. 2009; Development of a tracheostomy scoring system to guide airway management after major head and neck surgery. Int J Oral Maxillofac Surg. 38:846–9. https://doi.org/10.1016/j.ijom.2009.03.713. DOI: 10.1016/j.ijom.2009.03.713. PMID: 19423295.
Article7. Crosher R, Baldie C, Mitchell R. 1997; Selective use of tracheostomy in surgery for head and neck cancer: an audit. Br J Oral Maxillofac Surg. 35:43–5. https://doi.org/10.1016/s0266-4356(97)90008-5. DOI: 10.1016/S0266-4356(97)90008-5. PMID: 9043003.
Article8. Cai TY, Zhang WB, Yu Y, Wang Y, Mao C, Guo CB, et al. 2020; Scoring system for selective tracheostomy in head and neck surgery with free flap reconstruction. Head Neck. 42:476–84. https://doi.org/10.1002/hed.26028. DOI: 10.1002/hed.26028. PMID: 31799777.
Article9. Myatra SN, Gupta S, D'Cruz AK, Rajanala V, Dhar H, Sharma S, et al. 2021; Identification of patients for a delayed extubation strategy versus elective tracheostomy for postoperative airway management in major oral cancer surgery: a prospective observational study in seven hundred and twenty patients. Oral Oncol. 121:105502. https://doi.org/10.1016/j.oraloncology.2021.105502. DOI: 10.1016/j.oraloncology.2021.105502. PMID: 34450455.
Article10. Coyle MJ, Shrimpton A, Perkins C, Fasanmade A, Godden D. 2012; First do no harm: should routine tracheostomy after oral and maxillofacial oncological operations be abandoned? Br J Oral Maxillofac Surg. 50:732–5. https://doi.org/10.1016/j.bjoms.2012.01.003. DOI: 10.1016/j.bjoms.2012.01.003. PMID: 22325994.
Article11. Mohamedbhai H, Ali S, Dimasi I, Kalavrezos N. 2018; TRACHY score: a simple and effective guide to management of the airway in head and neck cancer. Br J Oral Maxillofac Surg. 56:709–14. https://doi.org/10.1016/j.bjoms.2018.07.015. DOI: 10.1016/j.bjoms.2018.07.015. PMID: 30126752.
Article12. Kim YH, Kim MY, Kim CH. 2014; Elective tracheostomy scoring system for severe oral disease patients. J Korean Assoc Oral Maxillofac Surg. 40:211–9. https://doi.org/10.5125/jkaoms.2014.40.5.211. DOI: 10.5125/jkaoms.2014.40.5.211. PMID: 25368833. PMCID: PMC4217265.
Article13. Bhatnagar S, Mishra S, Jha RR, Singhal AK. 2005; Predicting difficult laryngoscopy in oral cancer patients. Indian J Anaesth. 49:413–6.14. Dawson R, Phung D, Every J, Gunawardena D, Low TH, Ch'ng S, et al. 2021; Tracheostomy in free-flap reconstruction of the oral cavity: can it be avoided? A cohort study of 187 patients. ANZ J Surg. 91:1246–50. https://doi.org/10.1111/ans.16762. DOI: 10.1111/ans.16762. PMID: 33825282.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Preoperative risk evaluation and perioperative management of patients with obstructive sleep apnea: a narrative review
- Surgical Excision and Reconstruction in Oral Cavity Cancer
- Perioperative and anesthetic management of patients with rheumatoid arthritis
- The role of the Computed Tomography in Head and Neck Cancer: Comparison of CT Staging with Clinical Staging in Oral Cavity, Oropharynx and Larynx Cancer
- An Experience of Anesthesia of Congenital Anomaly with Airway Involvement : 46 case report