Clin Transplant Res.
2024 Jun;38(2):145-149. 10.4285/ctr.24.0002.
Successful kidney transplantation from a live donor with immune thrombocytopenia: a case report
- Affiliations
-
- 1Division of Pediatric Surgery, Department of Surgery, Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Hualien, Taiwan
- 2Division of General Surgery, Department of Surgery, Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Hualien, Taiwan
- 3Organ Transplantation Center, Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Hualien, Taiwan
- 4Department of Anesthesiology, Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Hualien, Taiwan
- 5Department of Hematology and Oncology, Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Hualien, Taiwan
- KMID: 2557608
- DOI: http://doi.org/10.4285/ctr.24.0002
Abstract
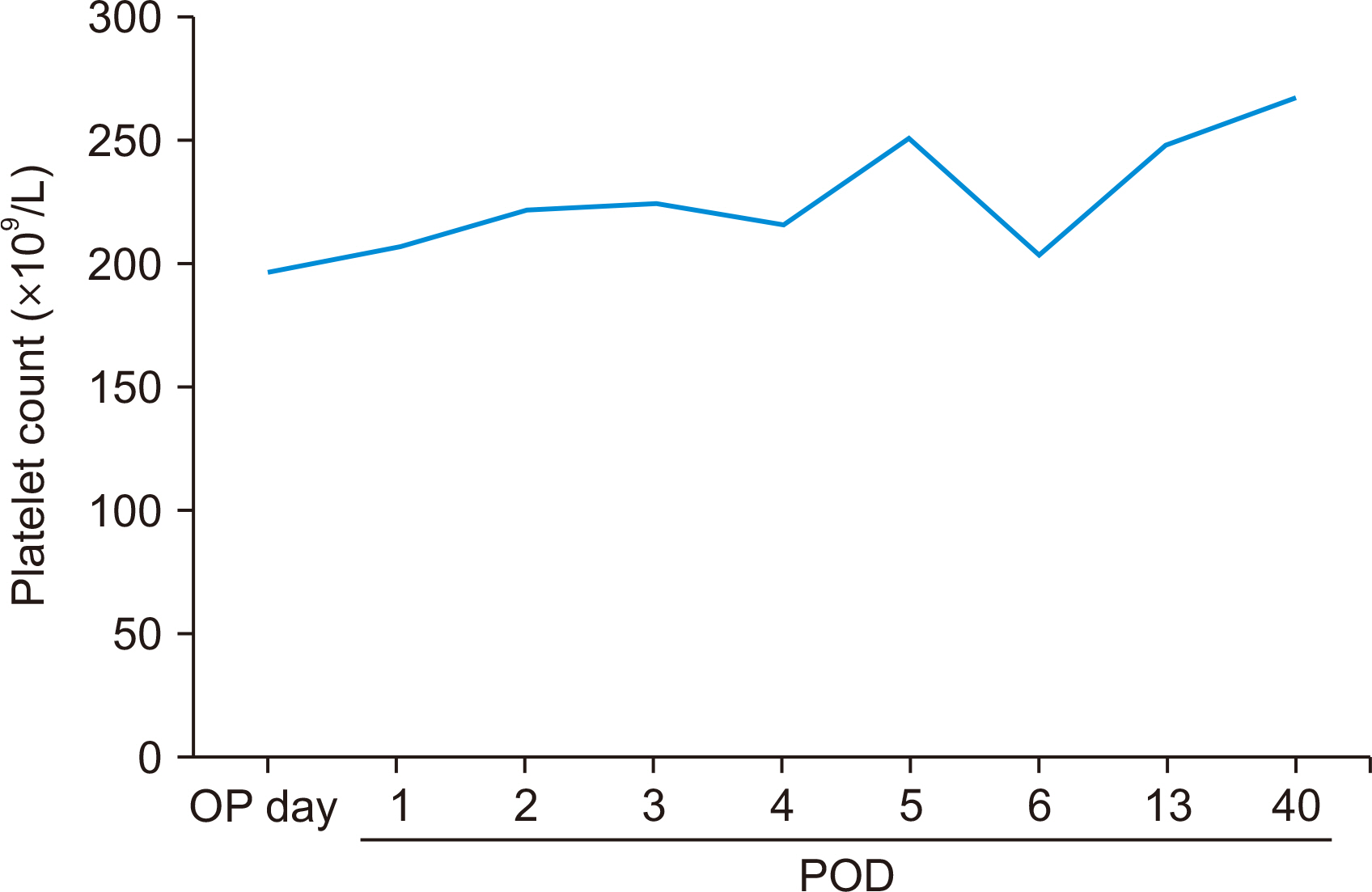
- Organ transplantation from donors with immune thrombocytopenia (ITP), a condition involving the autoantibody-mediated destruction of platelets, is a topic of debate due to the potential for transplantation-mediated autoimmune thrombocytopenia (TMAT), a rare but potentially fatal complication. Previous reports have described transplants from deceased liver donors with ITP who had very low platelet counts and disease largely refractory to treatment. Here, we present the first case of living kidney transplantation from a donor with ITP who underwent preoperative treatment, with concurrent splenectomy performed to reduce the long-term risk of spontaneous hemorrhage. To ensure the safety of the procedure, we monitored perioperative rotational thromboelastometry parameters and platelet counts, leading to the normalization of the donor’s platelet levels. The recipient experienced an uneventful recovery of renal function without perioperative bleeding or the development of TMAT. Our report suggests that kidney transplantation from a donor with well-managed ITP is safe, and such a condition should not be considered a contraindication for donation.
Keyword
Figure
Reference
-
1. Richardson R, Connelly M, Dipchand C, Garg AX, Ghanekar A, Houde I, et al. Kidney paired donation protocol for participating donors 2014. Transplantation. 2015; Oct. 99(10 Suppl 1):S1–88. DOI: 10.1097/TP.0000000000000918. PMID: 26425842.
Article2. Diaz GC, Prowda J, Lo IJ, Arepally GM, Evans N, Wheeless Y, et al. 2008; Transplantation-mediated alloimmune thrombocytopenia: guidelines for utilization of thrombocytopenic donors. Liver Transpl. 14:1803–9. DOI: 10.1002/lt.21539. PMID: 19025920.3. Hill QA, Harrison LC, Padmakumar AD, Owen RG, Prasad KR, Lucas GF, et al. 2017; A fatal case of transplantation-mediated alloimmune thrombocytopenia following liver transplantation. Hematology. 22:162–7. DOI: 10.1080/10245332.2016.1240392. PMID: 27764999.
Article4. Takatsuki M, Uemoto S, Kurokawa T, Koshiba T, Inomata Y, Tanaka K. 1999; Idiopathic thrombocytopenic purpura after a living-related liver transplantation. Transplantation. 67:479–81. DOI: 10.1097/00007890-199902150-00023. PMID: 10030298.
Article5. Trotter PB, Robb M, Summers D, Watson CJ, Clatworthy M, Bradley JA, et al. 2017; Donors with immune thrombocytopenia: do they pose a risk to transplant recipients? Am J Transplant. 17:796–802. DOI: 10.1111/ajt.14105. PMID: 27935215.
Article6. Lee JY, Lee JH, Lee H, Kang B, Kim JW, Kim SH, et al. 2017; Epidemiology and management of primary immune thrombocytopenia: a nationwide population-based study in Korea. Thromb Res. 155:86–91. DOI: 10.1016/j.thromres.2017.05.010. PMID: 28525829.
Article7. Cines DB, Bussel JB, Liebman HA, Luning Prak ET. 2009; The ITP syndrome: pathogenic and clinical diversity. Blood. 113:6511–21. DOI: 10.1182/blood-2009-01-129155. PMID: 19395674. PMCID: PMC2710913.8. Zychowicz A, Radkowiak D, Lasek A, Małczak P, Witowski J, Major P, et al. 2018; Laparoscopic splenectomy for immune thrombocytopenia in patients with a very low platelet count. Wideochir Inne Tech Maloinwazyjne. 13:157–63. DOI: 10.5114/wiitm.2018.75847. PMID: 30002747. PMCID: PMC6041578.
Article9. Nielsen VG, Geary BT, Baird MS. 2000; Evaluation of the contribution of platelets to clot strength by thromboelastography in rabbits: the role of tissue factor and cytochalasin D. Anesth Analg. 91:35–9. DOI: 10.1213/00000539-200007000-00007. PMID: 10866883.
Article10. Johnson RJ, Bradbury LL, Martin K, Neuberger J. UK Transplant Registry. 2014; Organ donation and transplantation in the UK-the last decade: a report from the UK national transplant registry. Transplantation. 97 Suppl 1:S1–27. DOI: 10.1097/01.TP.0000438215.16737.68. PMID: 24356460.11. Friend PJ, McCarthy LJ, Filo RS, Leapman SB, Pescovitz MD, Lumeng L, et al. 1990; Transmission of idiopathic (autoimmune) thrombocytopenic purpura by liver transplantation. N Engl J Med. 323:807–11. DOI: 10.1056/NEJM199009203231207. PMID: 2392133.12. de la Torre AN, Fisher A, Wilson DJ, Harrison J, Koneru B. 2004; A case report of donor to recipient transmission of severe thrombocytopenia purpura. Transplantation. 77:1473–4. DOI: 10.1097/01.TP.0000122417.61345.2D. PMID: 15167613.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transplantation of En Bloc Pediatric Cadaver Kidneys into Adult Recipient
- Successful Living Donor Kidney Transplantation in a Patient with MTHFR Deficiency and Heparin-Induced Thrombocytopenia: A Case Report
- Evaluation of the Recipient and Donor in Living Kidney Transplantation
- Kidney Transplantation after ex vivo Repair of an Aneurysm of the Donor Renal Artery
- Simultaneous Pancreas-kidney Transplantation from Pediatric Donor: A Case Report