Ann Surg Treat Res.
2024 Jul;107(1):35-41. 10.4174/astr.2024.107.1.35.
The evaluation of feasibility of ambulatory laparoscopic cholecystectomy using intraoperative instillation of bupivacaine: a retrospective observational study
- Affiliations
-
- 1Department of Surgery, School of Medicine, Chosun University, Gwangju, Korea
- KMID: 2557578
- DOI: http://doi.org/10.4174/astr.2024.107.1.35
Abstract
- Purpose
This study aimed to compare outcomes of opioid patients-controlled anesthesia (PCA) and intraoperative local anesthesia in terms of postoperative pain, lab results, patient surveys, and discharge scores to evaluate the feasibility of ambulatory laparoscopic cholecystectomy (LC).
Methods
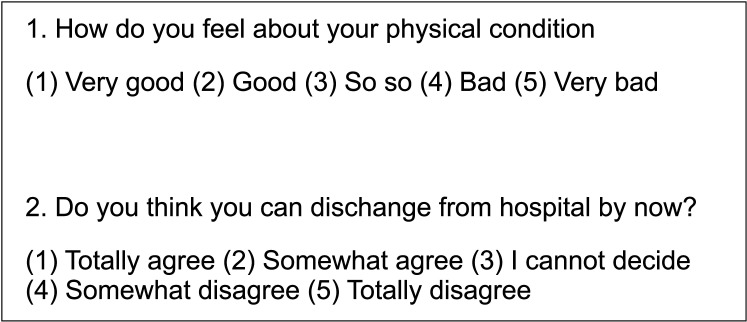
Patients who underwent LC for acute cholecystitis were assigned to the outpatient surgery (OPS) group or inpatient surgery (IPS) group according to the surgeon. In the OPS group, a mixture of bupivacaine and epinephrine was injected into trocar sites and sprayed on the surgical dissection field. Oral opioid and analgesics were given twice a day. In the IPS group, patients received opioid PCA. Numeric rating scale (NRS) for walking, erythrocyte sedimentation rate (ESR), CRP, self-assessed survey on general physical condition and discharge, and discharge score of ambulatory surgery were assessed postoperatively.
Results
NRS was significantly lower in the OPS group. There were no significant differences in ESR and CRP between the groups. Self-assessed survey on general conditions and the possibility of discharge were significantly better in the OPS group. The discharge scores at 3, 6, and 9 hours were significantly higher in the OPS group.
Conclusion
Intraoperative instillation of bupivacaine at port sites and dissection fields had a better effect on short-term postoperative pain, patient surveys, and discharge criteria of ambulatory surgery than opioid PCA.
Figure
Reference
-
1. Jiménez Fuertes M, Costa Navarro D. Outpatient laparoscopic cholecystectomy and pain control: a series of 100 cases. Cir Esp. 2015; 93:181–186. PMID: 24629917.2. Schuster KM, O’Connor R, Cripps M, Kuhlenschmidt K, Taveras L, Kaafarani HM, et al. Revision of the AAST grading scale for acute cholecyst it is with comparison to physiologic measures of severity. J Trauma Acute Care Surg. 2022; 92:664–674. PMID: 34936593.3. Schuster KM, O’Connor R, Cripps M, Kuhlenschmidt K, Taveras L, Kaafarani HM, et al. Multicenter validation of the American Association for the Surgery of Trauma grading scale for acute cholecystitis. J Trauma Acute Care Surg. 2021; 90:87–96. PMID: 33332782.4. Yokoe M, Hata J, Takada T, Strasberg SM, Asbun HJ, Wakabayashi G, et al. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2018; 25:41–54. PMID: 29032636.5. Kim TH, Kang H, Park JS, Chang IT, Park SG. Intraperitoneal ropivacaine instillation for postoperative pain relief after laparoscopic cholecystectomy. J Korean Surg Soc. 2010; 79:130–136.6. Sharmin I, Mahmud F, Chowdhury FA, Khatun M, Alam MT, Chowdhury AK. Comparison of pain control and analgesic consumption with or without infiltration of bupivacaine at port sites after laparoscopic cholecystectomy. Mymensingh Med J. 2023; 32:1133–1139. PMID: 37777912.7. Vijayaraghavalu S, Bharthi Sekar E. A comparative study on the postoperative analgesic effects of the intraperitoneal instillation of bupivacaine versus normal saline following laparoscopic cholecystectomy. Cureus. 2021; 13:e14151. PMID: 33927953.8. Arabzadeh A, Seyedsadeghi M, Sadeghi N, Nejati K, Mohammadian Erdi A. Comparison of intraperitoneal bupivacaine and intravenous ketorolac for postoperative pain management following laparoscopic cholecystectomy. Anesth Pain Med. 2021; 11:e114623. PMID: 35291402.9. Manan A, Khan AA, Ahmad I, Usman M, Jamil T, Sajid MA. Intraperitoneal bupivacaine as post-laparoscopic cholecystectomy analgesia. J Coll Physicians Surg Pak. 2020; 30:9–12.10. Sandhya S, Puthenveettil N, Vinodan K. Intraperitoneal nebulization of ropivacaine for control of pain after laparoscopic cholecystectomy: a randomized control trial. J Anaesthesiol Clin Pharmacol. 2021; 37:443–448. PMID: 34759559.11. Ingelmo PM, Bucciero M, Somaini M, Sahillioglu E, Garbagnati A, Charton A, et al. Intraperitoneal nebulization of ropivacaine for pain control after laparoscopic cholecystectomy: a double-blind, randomized, placebo-controlled trial. Br J Anaesth. 2013; 110:800–806. PMID: 23293276.12. Szem JW, Hydo L, Barie PS. A double-blinded evaluation of intraperitoneal bupivacaine vs saline for the reduction of postoperative pain and nausea after laparoscopic cholecystectomy. Surg Endosc. 1996; 10:44–48. PMID: 8711605.13. Mounika V, Sahu L, Mishra K, Mohapatra PS. A comparative evaluation of post-operative pain management using erector spinae plane block and oblique transverse abdominis plane block in patients undergoing laparoscopic cholecystectomy. Cureus. 2023; 15:e35750. PMID: 37020482.14. Güngör H, Ciftci B, Alver S, Gölboyu BE, Ozdenkaya Y, Tulgar S. Modified thoracoabdominal nerve block through perichondrial approach (M-TAPA) vs local infiltration for pain management after laparoscopic cholecystectomy surgery: a randomized study. J Anesth. 2023; 37:254–260. PMID: 36575362.15. Gin E, Lowen D, Tacey M, Hodgson R. Reduced laparoscopic intra-abdominal pressure during laparoscopic cholecystectomy and its effect on post-operative pain: a double-blinded randomised control trial. J Gastrointest Surg. 2021; 25:2806–2813. PMID: 33565010.16. Kwon OH, Kim SK, Mun DB, Yun YK. Outpatient laparoscopic cholecystectomy at ambulatory surgical center. Korean J Hepatobiliary Pancreat Surg. 2001; 5:109–115.17. Kang WJ, Kim SH, Lee SM. Effects of intraperitoneal lidocaine on abdominal and shoulder pain after a laparoscopic cholecystectomy. Korean J Anesthesiol. 2002; 42:198–204.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of 0.5% Bupivacaine Instillation for the Postoperative Pain after Laparoscopic Cholecystectomy
- The Effects of Intraperitoneal Local Anesthetics on the Postoperative Pain Relief in Laparoscopic Cholecystectomy
- The Topical Intraperitoneal Anesthesia of 0.5% Bupivacaine Before Laparoscopic Cholecystectomy is Effective on the Postoperative Pain Control
- Laparoscopic Cholecystectomy in the Second Trimester of Pregnancy
- Korea University Experience in Laparoscopic Cholecystectomy