Ann Surg Treat Res.
2024 Jul;107(1):27-34. 10.4174/astr.2024.107.1.27.
Analysis of the learning curve for laparoscopic pancreaticoduodenectomy based on a single surgeon’s experience: a retrospective observational study
- Affiliations
-
- 1Division of Hepato-Pancreato-Biliary Surgery, Department of Surgery, Chonnam National University Medical School, Gwangju, Korea
- KMID: 2557577
- DOI: http://doi.org/10.4174/astr.2024.107.1.27
Abstract
- Purpose
Laparoscopic pancreaticoduodenectomy (LPD) is a highly challenging procedure, which prevents its widespread adoption despite its advantages of being a minimally invasive procedure. This study analyzed the learning curve for LPD based on a single surgeon’s experience.
Methods
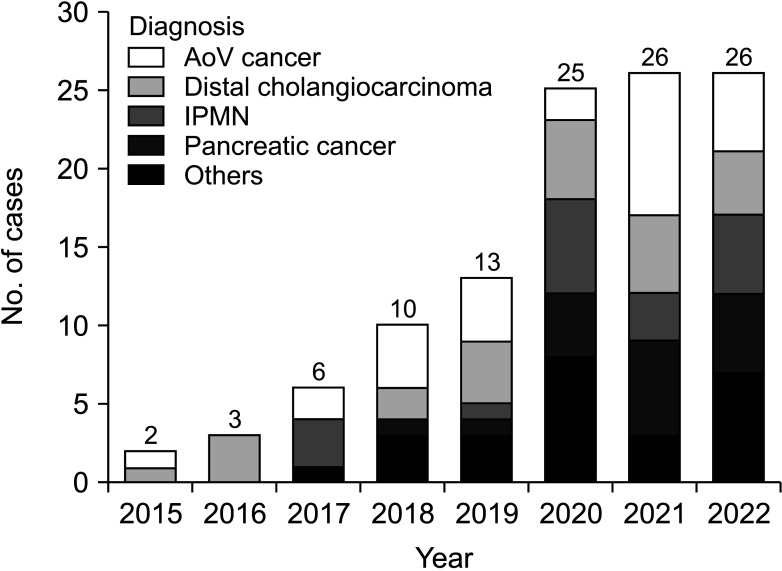
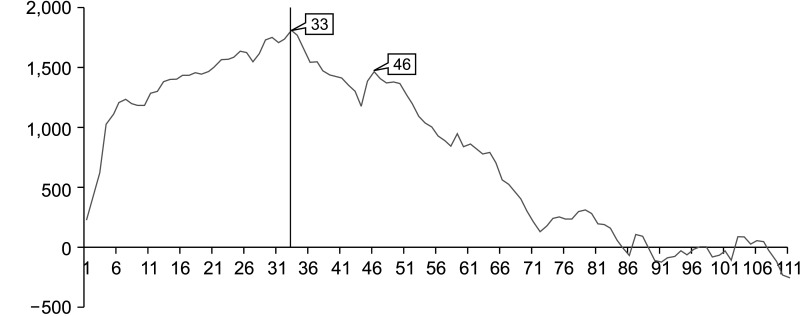
We retrospectively analyzed the medical records of 111 consecutive patients who underwent LPD by a single surgeon between March 2014 and October 2022. The learning curve was assessed using cumulative summation (CUSUM) and risk-adjusted CUSUM (RA-CUSUM) methods. Surgical failure was defined as conversion to an open procedure or the occurrence of severe complications (Clavien-Dindo grade ≥III). Based on the learning curve analysis, we divided the learning curve into the early and late phases and compared the operative outcomes in each phase.
Results
Based on the CUSUM analysis, the operation time decreased after the first 33 cases. Based on the RA-CUSUM analysis, the LPD technique stabilized after the 44th case. In the late phase, operation time, length of stay, and incidence of delayed gastric emptying, severe complications, and surgical failure were significantly lower than in the early phase.
Conclusion
Our results indicate that 44 cases are required for stabilization of the LPD technique and improvement of operative outcomes.
Keyword
Figure
Reference
-
1. Gagner M, Pomp A. Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc. 1994; 8:408–410. PMID: 7915434.2. Cuschieri A, Jakimowicz JJ, van Spreeuwel J. Laparoscopic distal 70% pancreatectomy and splenectomy for chronic pancreatitis. Ann Surg. 1996; 223:280–285. PMID: 8604908.3. Kim H, Choi HZ, Kang BM, Lee JW. Learning curve in laparoscopic pancreaticoduodenectomy: using risk-adjusted cumulative summation methods. J Laparoendosc Adv Surg Tech A. 2022; 32:401–407. PMID: 34388041.4. Kim S, Yoon YS, Han HS, Cho JY, Choi Y, Lee B. Evaluation of a single surgeon’s learning curve of laparoscopic pancreaticoduodenectomy: risk-adjusted cumulative summation analysis. Surg Endosc. 2021; 35:2870–2878. PMID: 32548654.5. Choi M, Hwang HK, Lee WJ, Kang CM. Total laparoscopic pancreaticoduodenectomy in patients with periampullary tumors: a learning curve analysis. Surg Endosc. 2021; 35:2636–2644. PMID: 32495184.6. Nagakawa Y, Nakamura Y, Honda G, Gotoh Y, Ohtsuka T, Ban D, et al. Learning curve and surgical factors influencing the surgical outcomes during the initial experience with laparoscopic pancreaticoduodenectomy. J Hepatobiliary Pancreat Sci. 2018; 25:498–507. PMID: 30291768.7. Wang M, Meng L, Cai Y, Li Y, Wang X, Zhang Z, et al. Learning curve for laparoscopic pancreaticoduodenectomy: a CUSUM analysis. J Gastrointest Surg. 2016; 20:924–935. PMID: 26902090.8. Song KB, Kim SC, Lee W, Hwang DW, Lee JH, Kwon J, et al. Laparoscopic pancreaticoduodenectomy for periampullary tumors: lessons learned from 500 consecutive patients in a single center. Surg Endosc. 2020; 34:1343–1352. PMID: 31214805.9. Subramaniam S, Aalberg JJ, Soriano RP, Divino CM. New 5-factor modified frailty index using American College of Surgeons NSQIP data. J Am Coll Surg. 2018; 226:173–181. PMID: 29155268.10. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213. PMID: 15273542.11. Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 2017; 161:584–591. PMID: 28040257.12. Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007; 142:761–768. PMID: 17981197.13. Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, et al. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007; 142:20–25. PMID: 17629996.14. Steiner SH, Cook RJ, Farewell VT, Treasure T. Monitoring surgical performance using risk-adjusted cumulative sum charts. Biostatistics. 2000; 1:441–452. PMID: 12933566.15. Li J, Jiang J, Jiang X, Liu L. Risk-adjusted monitoring of surgical performance. PLoS One. 2018; 13:e0200915. PMID: 30089109.16. Callery MP, Pratt WB, Kent TS, Chaikof EL, Vollmer CM Jr. A prospectively validated clinical risk score accurately predicts pancreatic fistula after pancreatoduodenectomy. J Am Coll Surg. 2013; 216:1–14. PMID: 23122535.17. Conrad C, Basso V, Passot G, Zorzi D, Li L, Chen HC, et al. Comparable long-term oncologic outcomes of laparoscopic versus open pancreaticoduodenectomy for adenocarcinoma: a propensity score weighting analysis. Surg Endosc. 2017; 31:3970–3978. PMID: 28205031.18. Croome KP, Farnell MB, Que FG, Reid-Lombardo KM, Truty MJ, Nagorney DM, et al. Total laparoscopic pancreaticoduodenectomy for pancreatic ductal adenocarcinoma: oncologic advantages over open approaches? Ann Surg. 2014; 260:633–640. PMID: 25203880.19. Zhang H, Lan X, Peng B, Li B. Is total laparoscopic pancreaticoduodenectomy superior to open procedure?: a meta-analysis. World J Gastroenterol. 2019; 25:5711–5731. PMID: 31602170.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Learning Curve and Clinicopathologic Analysis in Transperitoneal Laparoscopic Adrenalectomy; Performed by a Single Young Surgeon with No Experience of Open Adrenalectomy
- The Learning Curve for Single-Port Laparoscopic Cholecystectomy by Experienced Laparoscopic Surgeon
- The Learning Curve of the Beginner Surgeon with Supervisor for Laparoscopic Totally Extraperitoneal Repair
- Laparoscopic Appendectomy: Is There a Learning Curve after Completion of Colorectal Fellowships Training?
- Transition from Conventional to Reduced-Port Laparoscopic Gastrectomy to Treat Gastric Carcinoma: a Single Surgeon's Experience from a Small-Volume Center