Acute Crit Care.
2024 May;39(2):257-265. 10.4266/acc.2023.01620.
Implementation of Society for Cardiovascular Angiography and Interventions classification in patients with cardiogenic shock secondary to acute myocardial infarction in a spanish university hospital
- Affiliations
-
- 1Cardiac Intensive Care Unit, Division of Cardiology, Complejo Hospitalario Universitario, Badajoz, Spain
- 2Division of Cardiology, Complejo Hospitalario Universitario, Badajoz, Spain
- 3Interventional Cardiology Unit, Division of Cardiology, Complejo Hospitalario Universitario, Badajoz, Spain
- KMID: 2557242
- DOI: http://doi.org/10.4266/acc.2023.01620
Abstract
- Background
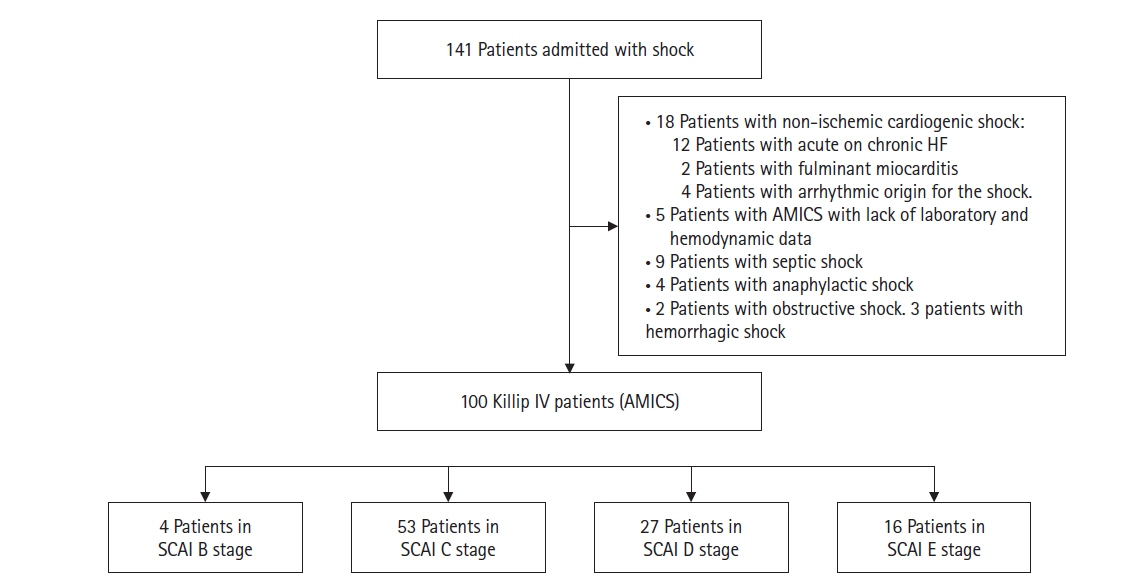
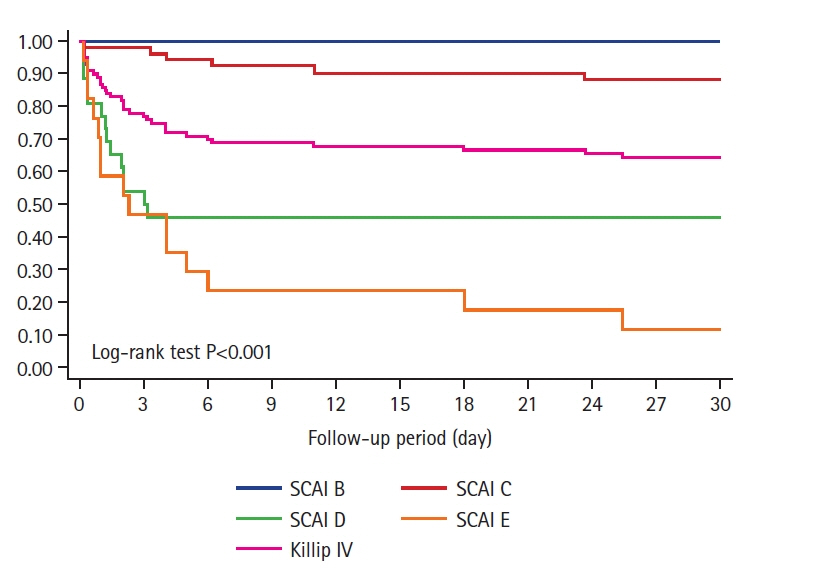
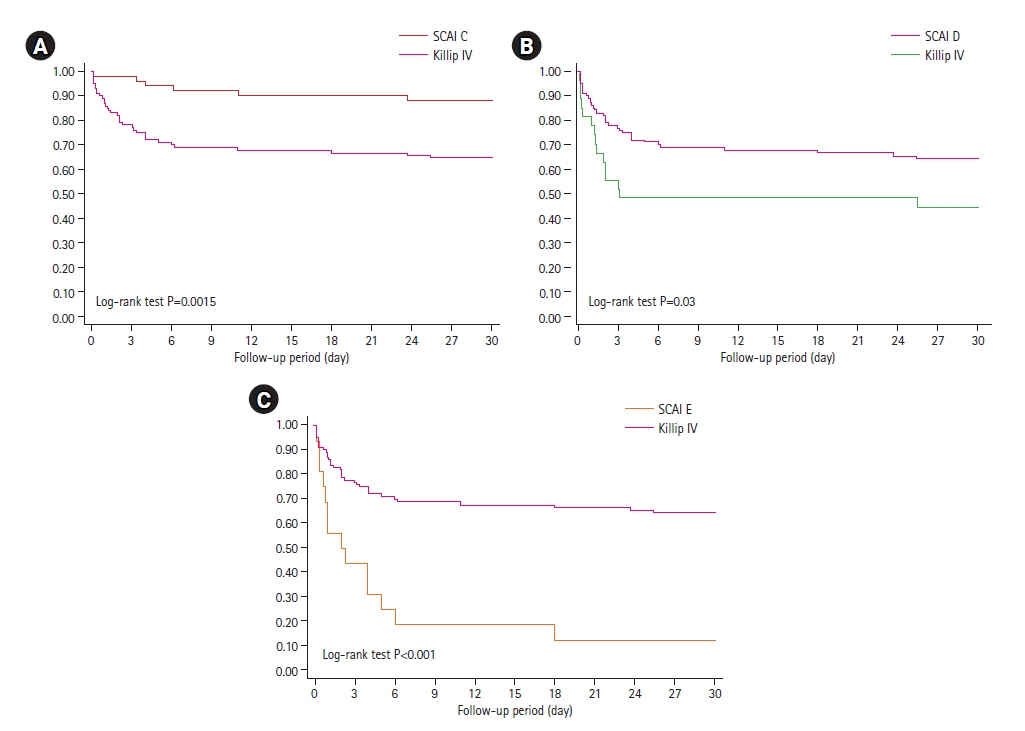
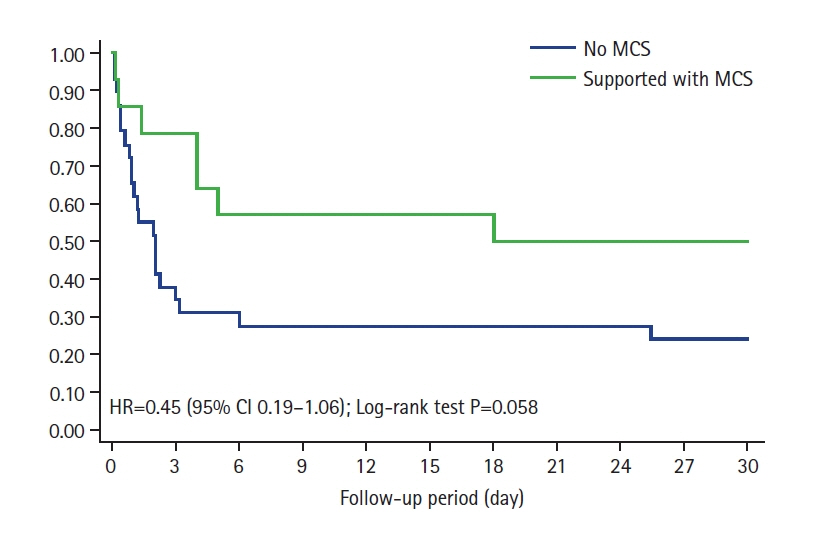
Killip-Kimball classification has been used for estimating death risk in patients suffering acute myocardial infarction (AMI). Killip-Kimball stage IV corresponds to cardiogenic shock. However, the Society for Cardiovascular Angiography and Interventions (SCAI) classification provides a more precise tool to classify patients according to shock severity. The aim of this study was to apply this classification to a cohort of Killip IV patients and to analyze the differences in death risk estimation between the two classifications. Methods: A single-center retrospective cohort study of 100 consecutive patients hospitalized for “Killip IV AMI” between 2016 and 2023 was performed to reclassify patients according to SCAI stage. Results: Distribution of patients according to SCAI stages was B=4%, C=53%, D=27%, E=16%. Thirty-day mortality increased progressively according to these stages (B=0%, C=11.88%, D=55.56%, E=87.50%; P<0.001). The exclusive use of Killip IV stage overestimated death risk compared to SCAI C (35% vs. 11.88%, P=0.002) and underestimated it compared to SCAI D and E stages (35% vs. 55.56% and 87.50%, P=0.03 and P<0.001, respectively). Age >69 years, creatinine >1.15 mg/dl and advanced SCAI stages (SCAI D and E) were independent predictors of 30-day mortality. Mechanical circulatory support use showed an almost significant benefit in advanced SCAI stages (D and E hazard ratio, 0.45; 95% confidence interval, 0.19–1.06; P=0.058). Conclusions: SCAI classification showed superior death risk estimation compared to Killip IV. Age, creatinine levels and advanced SCAI stages were independent predictors of 30-day mortality. Mechanical circulatory support could play a beneficial role in advanced SCAI stages.
Keyword
Figure
Reference
-
1. Kolte D, Khera S, Aronow WS, Mujib M, Palaniswamy C, Sule S, et al. Trends in incidence, management, and outcomes of cardiogenic shock complicating ST-elevation myocardial infarction in the United States. J Am Heart Assoc. 2014; 3:e000590.
Article2. Berg DD, Bohula EA, van Diepen S, Katz JN, Alviar CL, Baird-Zars VM, et al. Epidemiology of shock in contemporary cardiac intensive care units. Circ Cardiovasc Qual Outcomes. 2019; 12:e005618.3. Thiele H, Akin I, Sandri M, Fuernau G, de Waha S, Meyer-Saraei R, et al. PCI strategies in patients with acute myocardial infarction and cardiogenic shock. N Engl J Med. 2017; 377:2419–32.
Article4. Hunziker L, Radovanovic D, Jeger R, Pedrazzini G, Cuculi F, Urban P, et al. Twenty-year trends in the incidence and outcome of cardiogenic shock in AMIS plus registry. Circ Cardiovasc Interv. 2019; 12:e007293.5. Killip T 3rd, Kimball JT. Treatment of myocardial infarction in a coronary care unit: a two year experience with 250 patients. Am J Cardiol. 1967; 20:457–64.6. Baran DA, Grines CL, Bailey S, Burkhoff D, Hall SA, Henry TD, et al. SCAI clinical expert consensus statement on the classification of cardiogenic shock: this document was endorsed by the American College of Cardiology (ACC), the American Heart Association (AHA), the Society of Critical Care Medicine (SCCM), and the Society of Thoracic Surgeons (STS) in April 2019. Catheter Cardiovasc Interv. 2019; 94:29–37.
Article7. Naidu SS, Baran DA, Jentzer JC, Hollenberg SM, van Diepen S, Basir MB, et al. SCAI SHOCK stage classification expert consensus update: a review and incorporation of validation studies. J Soc Cardiovasc Angiogr Interv. 2022; 1:100008.
Article8. Baran DA, Long A, Badiye AP, Stelling K. Prospective validation of the SCAI shock classification: single center analysis. Catheter Cardiovasc Interv. 2020; 96:1339–47.9. Schrage B, Dabboura S, Yan I, Hilal R, Neumann JT, Sörensen NA, et al. Application of the SCAI classification in a cohort of patients with cardiogenic shock. Catheter Cardiovasc Interv. 2020; 96:E213–9.
Article10. Hanson ID, Tagami T, Mando R, Kara Balla A, Dixon SR, Timmis S, et al. SCAI shock classification in acute myocardial infarction: insights from the National Cardiogenic Shock Initiative. Catheter Cardiovasc Interv. 2020; 96:1137–42.11. Wayangankar SA, Bangalore S, McCoy LA, Jneid H, Latif F, Karrowni W, et al. Temporal trends and outcomes of patients undergoing percutaneous coronary interventions for cardiogenic shock in the setting of acute myocardial infarction: a report from the CathPCI registry. JACC Cardiovasc Interv. 2016; 9:341–51.12. Belletti A, Lerose CC, Zangrillo A, Landoni G. Vasoactive-inotropic score: evolution, clinical utility, and pitfalls. J Cardiothorac Vasc Anesth. 2021; 35:3067–77.
Article13. González-Pacheco H, Gopar-Nieto R, Araiza-Garaygordobil D, Briseño-Cruz JL, Eid-Lidt G, Ortega-Hernandez JA, et al. Application of the SCAI classification to admission of patients with cardiogenic shock: analysis of a tertiary care center in a middle-income country. PLoS One. 2022; 17:e0273086.
Article14. Jentzer JC, van Diepen S, Barsness GW, Henry TD, Menon V, Rihal CS, et al. Cardiogenic shock classification to predict mortality in the cardiac intensive care unit. J Am Coll Cardiol. 2019; 74:2117–28.15. Jentzer JC, Schrage B, Holmes DR, Dabboura S, Anavekar NS, Kirchhof P, et al. Influence of age and shock severity on short-term survival in patients with cardiogenic shock. Eur Heart J Acute Cardiovasc Care. 2021; 10:604–12.
Article16. Schrage B, Becher PM, Goßling A, Savarese G, Dabboura S, Yan I, et al. Temporal trends in incidence, causes, use of mechanical circulatory support and mortality in cardiogenic shock. ESC Heart Fail. 2021; 8:1295–303.
Article17. Kim Y, Park J, Essa M, Lansky AJ, Sugeng L. Frequency of management of cardiogenic shock with mechanical circulatory support devices according to race. Am J Cardiol. 2020; 125:1782–7.
Article18. Berg DD, Kaur G, Bohula EA, Baird-Zars VM, Alviar CL, Barnett CF, et al. Prognostic significance of haemodynamic parameters in patients with cardiogenic shock. Eur Heart J Acute Cardiovasc Care. 2023; 12:651–60.
Article19. Harjola VP, Lassus J, Sionis A, Køber L, Tarvasmäki T, Spinar J, et al. Clinical picture and risk prediction of short-term mortality in cardiogenic shock. Eur J Heart Fail. 2015; 17:501–9.
Article20. Pöss J, Köster J, Fuernau G, Eitel I, de Waha S, Ouarrak T, et al. Risk stratification for patients in cardiogenic shock after acute myocardial infarction. J Am Coll Cardiol. 2017; 69:1913–20.21. Damluji AA, Forman DE, van Diepen S, Alexander KP, Page RL 2nd, Hummel SL, et al. Older adults in the cardiac intensive care unit: factoring geriatric syndromes in the management, prognosis, and process of care: a scientific statement from the American Heart Association. Circulation. 2020; 141:e6–32.
Article22. Koreny M, Karth GD, Geppert A, Neunteufl T, Priglinger U, Heinz G, et al. Prognosis of patients who develop acute renal failure during the first 24 hours of cardiogenic shock after myocardial infarction. Am J Med. 2002; 112:115–9.
Article23. Ho HH, Ong HA, Arasaratnam P, Ooi YW, Tan J, Loh KK, et al. Predictors of in-hospital mortality in patients with acute myocardial infarction complicated by cardiogenic shock in the contemporary era of primary percutaneous coronary intervention. Int J Cardiol Heart Vessel. 2014; 3:88–9.
Article24. Fuernau G, Poenisch C, Eitel I, Denks D, de Waha S, Pöss J, et al. Prognostic impact of established and novel renal function biomarkers in myocardial infarction with cardiogenic shock: a biomarker substudy of the IABP-SHOCK II-trial. Int J Cardiol. 2015; 191:159–66.
Article25. Zweck E, Kanwar M, Li S, Sinha SS, Garan AR, Hernandez-Montfort J, et al. Clinical course of patients in cardiogenic shock stratified by phenotype. JACC Heart Fail. 2023; 11:1304–15.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraaortic Balloon Counterpulsation Support in Cardiogenic Shock due to Ventricular Septal Perforation and Huge Inferior Myocardial Infarction
- Mechanical Circulatory Support in the Cardiac Catheterization Laboratory for Cardiogenic Shock
- Operative Treatment of Mitral Valve Regurgitation due to Papillary Muscle Rupture from Acute Myocardial Infarction Under ECMO: A case report
- Coronary Intervention of Cardiogenic Shock in Acute Myocardial Infarction
- A case of acute anterior and lateral myocardial infarction altering with time from a large intracoronary thrombus on left main trunk