Child Kidney Dis.
2024 Jun;28(2):74-79. 10.3339/ckd.24.009.
Effect of renal Doppler ultrasound on the detection of nutcracker syndrome in children presenting orthostatic proteinuria
- Affiliations
-
- 1Department of Pediatrics, Yonsei University College of Medicine, Seoul, Republic of Korea
- 2Department of Radiology, Severance Hospital and Research Institute of Radiological Science, Yonsei University College of Medicine, Seoul, Republic of Korea
- 3Division of Pediatric Nephrology, Severance Children’s Hospital, Seoul, Republic of Korea
- 4Institute of Kidney Disease Research, Yonsei University College of Medicine, Seoul, Republic of Korea
- 5Severance Underwood Meta-Research Center, Institute of Convergence Science, Yonsei University, Seoul, Republic of Korea
- KMID: 2557073
- DOI: http://doi.org/10.3339/ckd.24.009
Abstract
- Purpose
To compare the Doppler sonographic findings of the left renal vein (LRV) of children diagnosed with nutcracker syndrome with and without orthostatic proteinuria.
Methods
Fifty and 53 consecutive children with and without orthostatic proteinuria, respectively, underwent renal Doppler ultrasonography examinations. The peak velocity (PV) was measured at the hilar portion of the LRV and between the aorta and superior mesenteric artery. Renal Doppler ultrasonography findings and clinical data including urine protein-to-creatinine ratio (UPCR) were compared according to the presence or absence of orthostatic proteinuria.
Results
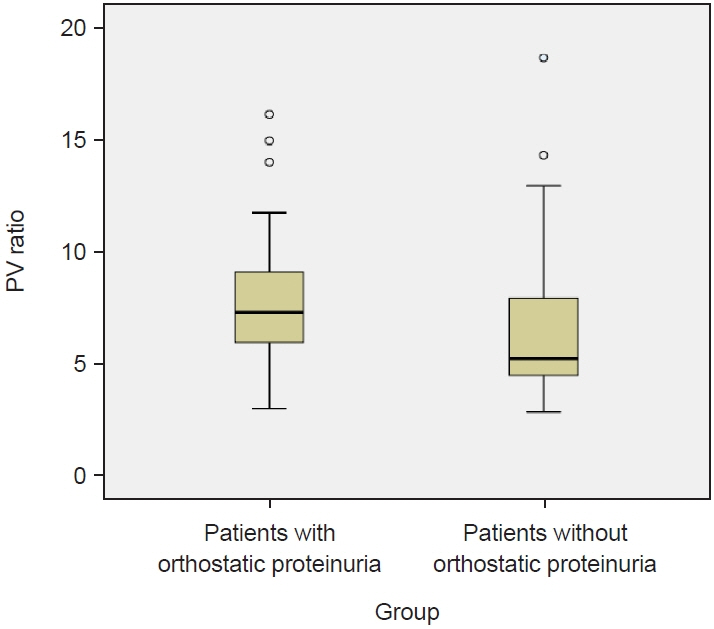
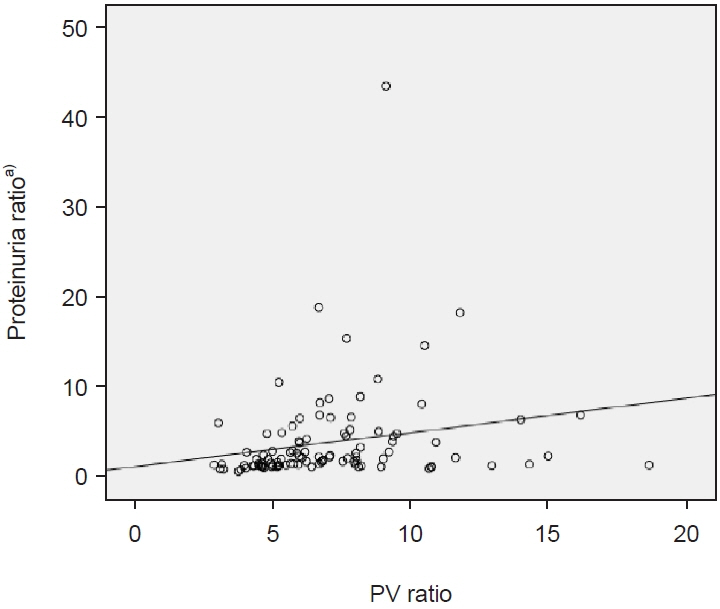
Between the two groups, no significant differences were observed in terms of age or sex. The PV ratio between the aortomesenteric and hilar portions was 7.79±2.65 and 6.32±3.01 in children with and without orthostatic proteinuria, respectively (P=0.009). No significant differences were observed between the two groups in terms of the UPCR in the first morning urine sample. However, the UPCR in the afternoon urine sample was significantly higher in children with orthostatic proteinuria than in those without orthostatic proteinuria (0.49±0.46 vs. 0.11±0.04 mg/mg, P<0.001). Furthermore, the PV ratio between the aortomesenteric and hilar portions revealed a positive correlation with the ratio of UPCR of the afternoon and that of first morning urine samples (R=0.21, P=0.034).
Conclusions
This study suggests that there can be a significant correlation of the PV ratio between the aortomesenteric and hilar portion of the LRV with orthostatic proteinuria in pediatric patients with nutcracker syndrome.
Figure
Cited by 1 articles
-
Nutcracker syndrome in pediatrics: a rare entity?
Hyung Eun Yim
Child Kidney Dis. 2024;28(3):90-92. doi: 10.3339/ckd.24.014.
Reference
-
References
1. Ananthan K, Onida S, Davies AH. Nutcracker syndrome: an update on current diagnostic criteria and management guidelines. Eur J Vasc Endovasc Surg. 2017; 53:886–94.
Article2. Kalantar DS, Park SJ, Shin JI. Nutcracker syndrome in children: review of symptom, diagnosis, and treatment. Child Kidney Dis. 2023; 27:89–96.
Article3. Kim SH. Doppler US and CT diagnosis of nutcracker syndrome. Korean J Radiol. 2019; 20:1627–37.
Article4. Park SJ, Lim JW, Cho BS, Yoon TY, Oh JH. Nutcracker syndrome in children with orthostatic proteinuria: diagnosis on the basis of Doppler sonography. J Ultrasound Med. 2002; 21:39–45.5. Cho BS, Choi YM, Kang HH, Park SJ, Lim JW, Yoon TY. Diagnosis of nut-cracker phenomenon using renal Doppler ultrasound in orthostatic proteinuria. Nephrol Dial Transplant. 2001; 16:1620–5.
Article6. Gulleroglu NB, Gulleroglu K, Uslu N, Baskin E. Left renal vein entrapment in postural proteinuria: the diagnostic utility of the aortomesenteric angle. Eur J Pediatr. 2022; 181:3339–43.
Article7. Mazzoni MB, Kottanatu L, Simonetti GD, Ragazzi M, Bianchetti MG, Fossali EF, et al. Renal vein obstruction and orthostatic proteinuria: a review. Nephrol Dial Transplant. 2011; 26:562–5.
Article8. Shin JI, Park SJ, Cho MH, Kim JH. Left renal venographic findings in children with orthostatic proteinuria. Nephrol Dial Transplant. 2011; 26:2715.
Article9. Ekim M, Bakkaloglu SA, Tumer N, Sanlidilek U, Salih M. Orthostatic proteinuria as a result of venous compression (nutcracker phenomenon): a hypothesis testable with modern imaging techniques. Nephrol Dial Transplant. 1999; 14:826–7.10. Lee SJ, You ES, Lee JE, Chung EC. Left renal vein entrapment syndrome in two girls with orthostatic proteinuria. Pediatr Nephrol. 1997; 11:218–20.
Article11. Shintaku N, Takahashi Y, Akaishi K, Sano A, Kuroda Y. Entrapment of left renal vein in children with orthostatic proteinuria. Pediatr Nephrol. 1990; 4:324–7.
Article12. Leung AK, Wong AH, Barg SS. Proteinuria in children: evaluation and differential diagnosis. Am Fam Physician. 2017; 95:248–54.13. Kim SH, Cho SW, Kim HD, Chung JW, Park JH, Han MC. Nutcracker syndrome: diagnosis with Doppler US. Radiology. 1996; 198:93–7.
Article14. Park SJ, Shin JI. Low body mass index in nutcracker phenomenon: an underrecognized condition. Kidney Int. 2013; 84:1287.
Article15. El-Sadr AR, Mina E. Anatomical and surgical aspects in the operative management of varicocele. Urol Cutaneous Rev. 1950; 54:257–62.16. Hersey N, Masood J, Papatsoris AG, Staios D, Buchholz N, Albanis S. ‘The Nutcracker Phenomenon’: case report and review of literature. Curr Urol. 2007; 1:110–2.17. de Schepper A. "Nutcracker" phenomenon of the renal vein and venous pathology of the left kidney. J Belge Radiol. 1972; 55:507–11.18. Berthelot JM, Douane F, Maugars Y, Frampas E. Nutcracker syndrome: a rare cause of left flank pain that can also manifest as unexplained pelvic pain. Joint Bone Spine. 2017; 84:557–62.
Article19. Mohammadi A, Ghasemi-Rad M, Mladkova N, Masudi S. Varicocele and nutcracker syndrome: sonographic findings. J Ultrasound Med. 2010; 29:1153–60.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Nutcracker Syndrome Presenting with Orthostatic Proteinuria
- Orthostatic Proteinuria with Nutcracker Phenomenon: Case Report
- A Case of Nutcracker Syndrome Associated with Orthostatic Proteinuria and Idiopathic Chronic Fatigue in a Child
- Mesangial Hypercellularity in a Patient with Nutcracker Syndrome and Orthostatic Proteinuria
- Significant Proteinuria Caused by Posterior Nutcracker Phenomenon