Child Kidney Dis.
2024 Jun;28(2):66-73. 10.3339/ckd.24.010.
Hematuria in children: causes and evaluation
- Affiliations
-
- 1Department of Pediatrics, Korea University Guro Hospital, Seoul, Republic of Korea
- 2Department of Urology and Urological Science Institute, Yonsei University College of Medicine, Seoul, Republic of Korea
- 3Department of Pediatrics, Inha University Hospital, Inha University College of Medicine, Incheon, Republic of Korea
- 4Department of Urology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea
- 5Department of Pediatrics, Seoul National University Children’s Hospital, Seoul, Republic of Korea
- 6Department of Pediatrics, Seoul National University College of Medicine, Seoul, Republic of Korea
- 7Department of Pediatrics, Hallym University Sacred Heart Hospital, Anyang, Republic of Korea
- 8Department of Pediatrics, Chung-Ang University Hospital, Seoul, Republic of Korea
- 9Department of Pediatrics, Jeju National University College of Medicine, Jeju, Republic of Korea
- 10Department of Biostatistics, Korea University College of Medicine, Seoul, Republic of Korea
- 11Division for Healthcare Technology Assessment Research, National Evidence-Based Healthcare Collaborating Agency, Seoul, Republic of Korea
- 12Department of Pediatrics, Bucheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea
- 13Department of Pediatrics, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Republic of Korea
- KMID: 2557072
- DOI: http://doi.org/10.3339/ckd.24.010
Abstract
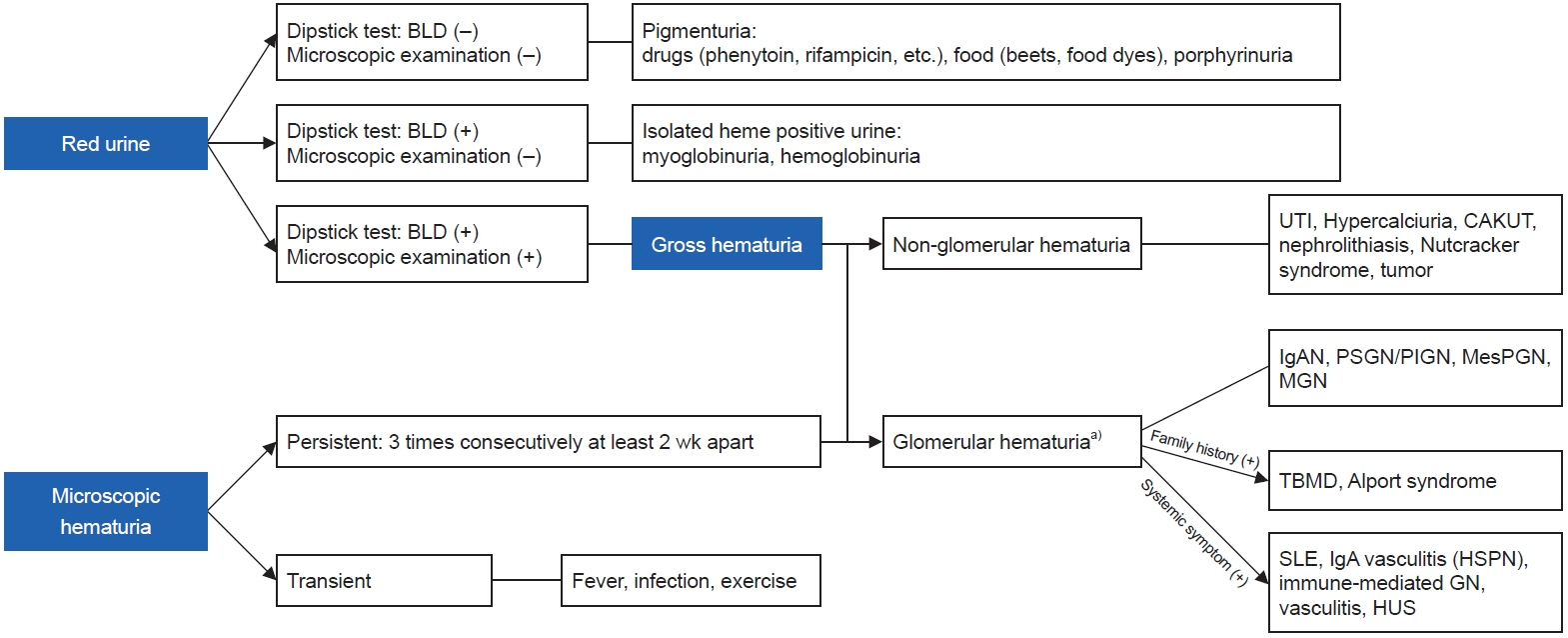
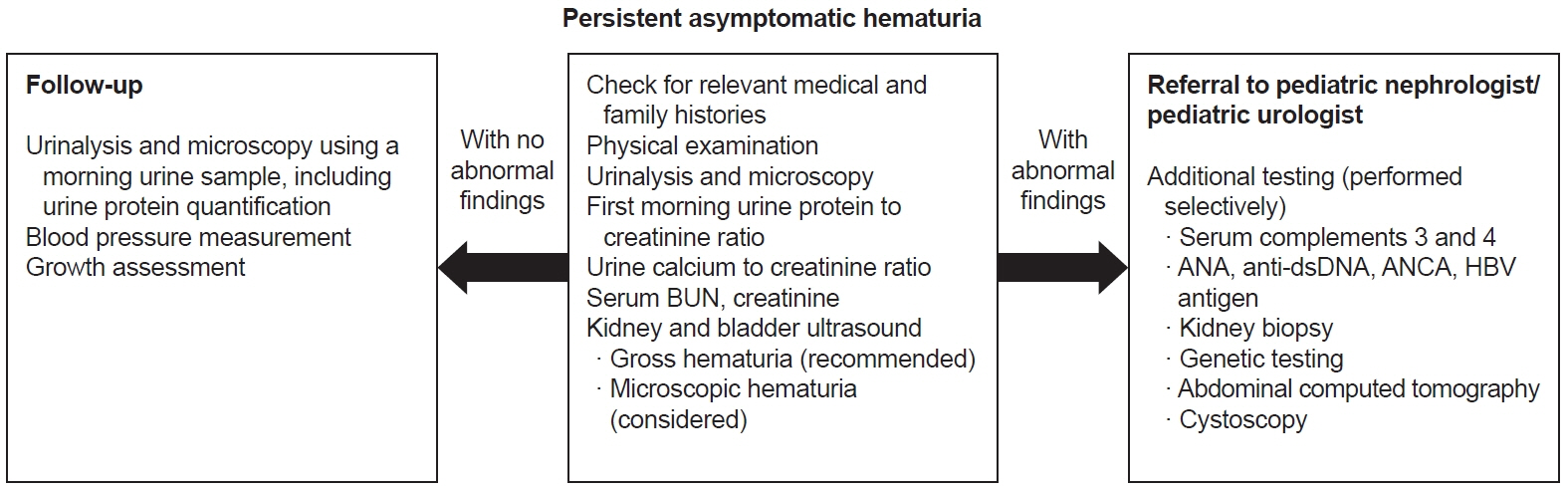
- Hematuria is the presence of blood in the urine and is classified as either gross hematuria or microscopic hematuria. There are many causes of hematuria, and the differential diagnosis depends on the presence or absence of comorbidities and whether it is glomerular or non-glomerular. When hematuria in children is symptomatic or persistent, an evaluation of the cause is essential. The causes of hematuria and basic approaches to its diagnosis are discussed in this review.
Keyword
Figure
Reference
-
References
1. Kliegman RM, Stanton B, St Geme JW, Schor NF, Behrman RE, Nelson WE. Nelson textbook of pediatrics. 21th ed. Elsevier;2019.2. Geary DF, Schaefer F. Pediatric kidney disease. 2nd ed. Elsevier;2016.3. Bignall ONR 2nd, Dixon BP. Management of hematuria in children. Curr Treat Options Pediatr. 2018; 4:333–49.
Article4. Vedula R, Iyengar AA. Approach to diagnosis and management of hematuria. Indian J Pediatr. 2020; 87:618–24.
Article5. Bergstein J, Leiser J, Andreoli S. The clinical significance of asymptomatic gross and microscopic hematuria in children. Arch Pediatr Adolesc Med. 2005; 159:353–5.
Article6. Youn T, Trachtman H, Gauthier B. Clinical spectrum of gross hematuria in pediatric patients. Clin Pediatr (Phila). 2006; 45:135–41.
Article7. Greenfield SP, Williot P, Kaplan D. Gross hematuria in children: a ten-year review. Urology. 2007; 69:166–9.
Article8. Mishra K, Kumar M, Patel A, Singh L, Zanak KD. Clinico-etiologic profile of macroscopic hematuria in children: a single center experience. Indian Pediatr. 2022; 59:25–7.
Article9. Kashtan CE, Gross O. Clinical practice recommendations for the diagnosis and management of Alport syndrome in children, adolescents, and young adults-an update for 2020. Pediatr Nephrol. 2021; 36:711–9.
Article10. Clark M, Aronoff S, Del Vecchio M. Etiologies of asymptomatic microscopic hematuria in children: systematic review of 1092 subjects. Diagnosis (Berl). 2015; 2:211–6.11. Vehaskari VM, Rapola J, Koskimies O, Savilahti E, Vilska J, Hallman N. Microscopic hematuria in school children: epidemiology and clinicopathologic evaluation. J Pediatr. 1979; 95(5 Pt 1):676–84.12. Trachtman H, Weiss RA, Bennett B, Greifer I. Isolated hematuria in children: indications for a renal biopsy. Kidney Int. 1984; 25:94–9.
Article13. Piqueras AI, White RH, Raafat F, Moghal N, Milford DV. Renal biopsy diagnosis in children presenting with haematuria. Pediatr Nephrol. 1998; 12:386–91.
Article14. Lin CY, Hsieh CC, Chen WP, Yang LY, Wang HH. The underlying diseases and follow-up in Taiwanese children screened by urinalysis. Pediatr Nephrol. 2001; 16:232–7.
Article15. Lee YM, Baek SY, Kim JH, Kim DS, Lee JS, Kim PK. Analysis of renal biopsies performed in children with abnormal findings in urinary mass screening. Acta Paediatr. 2006; 95:849–53.
Article16. Moghtaderi M, Noohi AH, Safaeyan B, Abbasi A, Sabsechian M, Meherkash M. Screening for microscopic hematuria in school-age children of Gorgan City. Iran J Kidney Dis. 2014; 8:70–2.17. Guven S, Gokce I, Deniz NC, Altuntas U, Yildiz N, Alpay H. Clinical and histopathological features of asymptomaticpersistent microscopic hematuria in children. Turk J Med Sci. 2016; 46:1707–11.
Article18. Hisano S, Ueda K. Asymptomatic haematuria and proteinuria: renal pathology and clinical outcome in 54 children. Pediatr Nephrol. 1989; 3:229–34.
Article19. Horie S, Ito S, Okada H, Kikuchi H, Narita I, Nishiyama T, et al. Japanese guidelines of the management of hematuria 2013. Clin Exp Nephrol. 2014; 18:679–89.
Article20. Brown DD, Reidy KJ. Approach to the child with hematuria. Pediatr Clin North Am. 2019; 66:15–30.
Article21. Hamadah AM, Gharaibeh K, Mara KC, Thompson KA, Lieske JC, Said S, et al. Urinalysis for the diagnosis of glomerulonephritis: role of dysmorphic red blood cells. Nephrol Dial Transplant. 2018; 33:1397–403.
Article22. Kidney Disease: Improving Global Outcomes (KDIGO) Glomerular Diseases Work Group. KDIGO 2021 clinical practice guideline for the management of glomerular diseases. Kidney Int. 2021; 100(4S):S1–276.23. Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, et al. New equations to estimate GFR in children with CKD. J Am Soc Nephrol. 2009; 20:629–37.
Article24. Kovacevic L. Diagnosis and management of nephrolithiasis in children. Pediatr Clin North Am. 2022; 69:1149–64.
Article25. Schwartz GJ, Schneider MF, Maier PS, Moxey-Mims M, Dharnidharka VR, Warady BA, et al. Improved equations estimating GFR in children with chronic kidney disease using an immunonephelometric determination of cystatin C. Kidney Int. 2012; 82:445–53.
Article26. Park E, Kim SW, Kim SJ, Baek M, Ahn YH, Yang EM, et al. Asymptomatic hematuria in children: Korean Society of Pediatric Nephrology recommendations for diagnosis and management. Kidney Res Clin Pract 2024 Mar 7 [Epub]. https://doi.org/10.23876/j.krcp.23.231.
Article