Ann Rehabil Med.
2024 Jun;48(3):211-219. 10.5535/arm.240010.
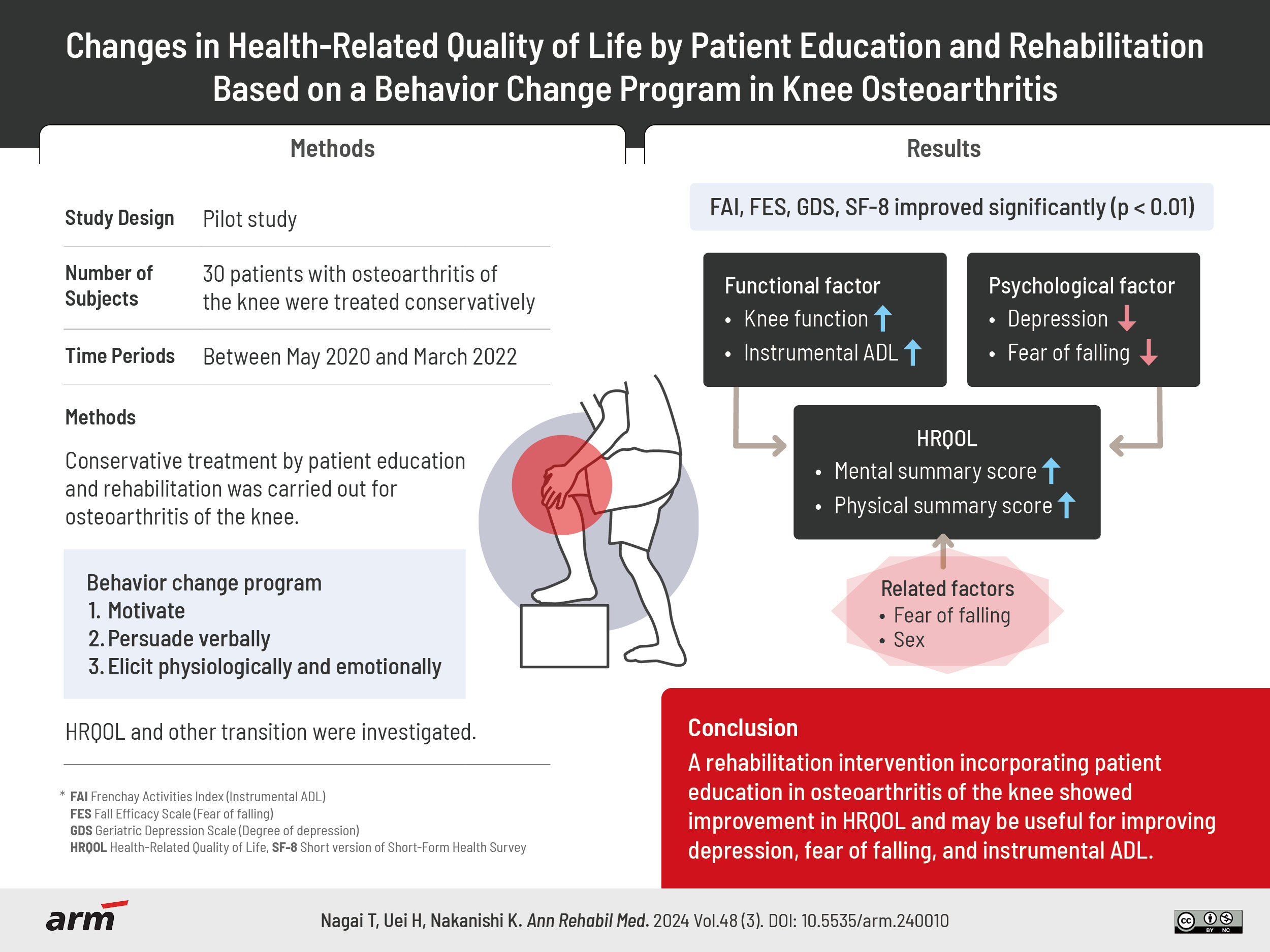
Changes in Health-Related Quality of Life by Patient Education and Rehabilitation Based on a Behavior Change Program in Knee Osteoarthritis
- Affiliations
-
- 1Department of Rehabilitation Medicine, Nihon University Hospital, Tokyo, Japan
- 2Department of Rehabilitation Medicine, Tokyo Women’s Medical University, Tokyo, Japan
- 3Department of Orthopedic Surgery, Nihon University School of Medicine, Tokyo, Japan
- KMID: 2557068
- DOI: http://doi.org/10.5535/arm.240010
Abstract
Objective
The purpose of this study was to examine how rehabilitation and patient education for knee osteoarthritis improves health-related quality of life (HRQOL) and to identify factors influencing HRQOL.
Methods
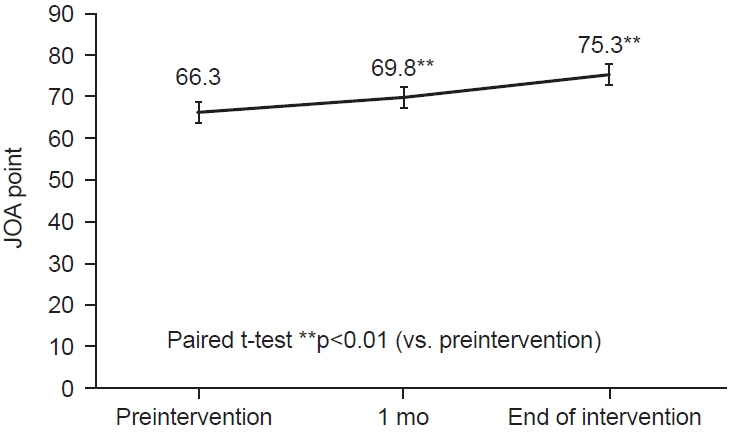
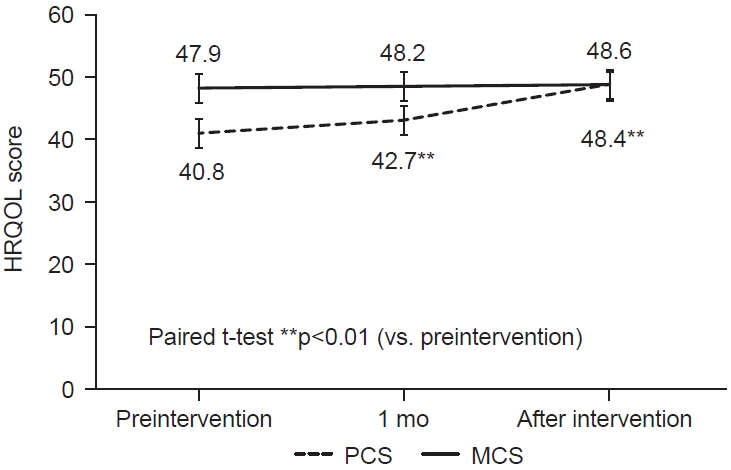
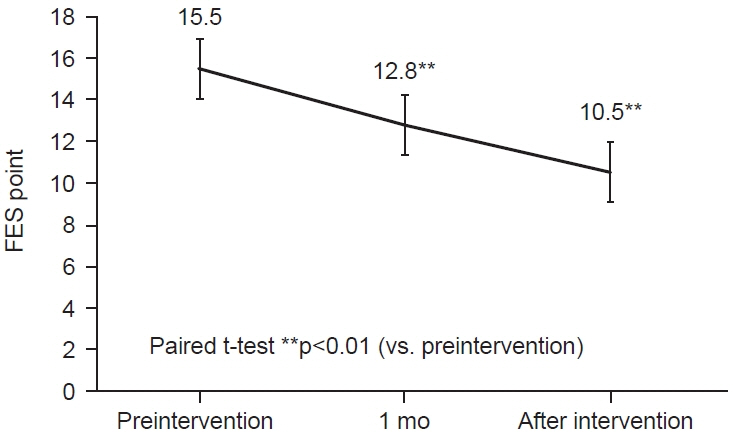
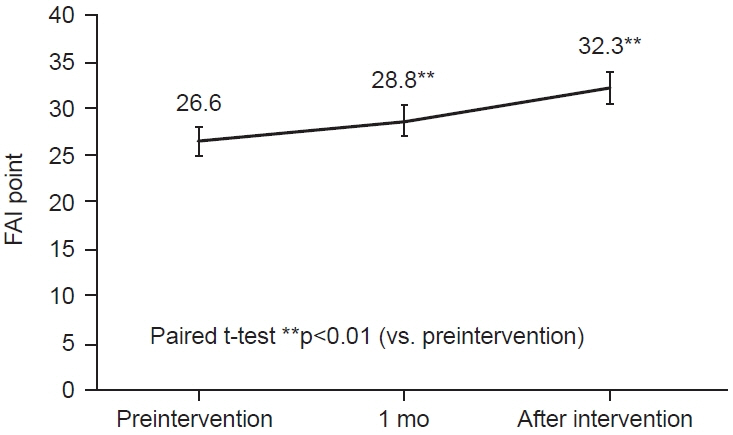
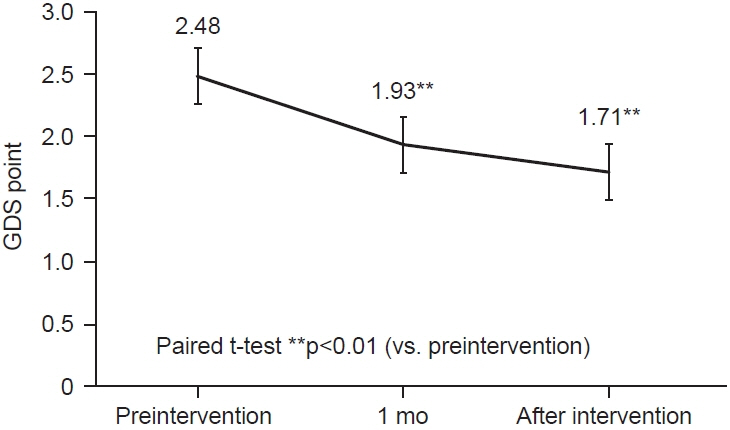
Between May 2020 and March 2022, 30 patients with osteoarthritis of the knee were treated conservatively and rehabilitated with a patient education program. The patient education program was based on the health belief model by Sedlak et al., and patient education using pamphlets was provided during the rehabilitation intervention. The survey items were patient basic information, instrumental activities of daily living (ADL) (FAI), fear of falling (FES), degree of depression (GDS), HRQOL (SF-8), knee function assessment (JOA score), and X-ray classification (K-L classification), and the survey method was a self-administered questionnaire at the start of rehabilitation, 1 month after the intervention, and at the end of the rehabilitation intervention. We examined factors affecting the physical component summary (PCS) and mental component summary (MCS) of HRQOL scores.
Results
JOA score, FES, FAI, GDS, and SF-8 improved significantly (p<0.01). MCS was also negatively correlated with FES and age (r=-0.486, -0.368). Sex was extracted as a factor for PCS as a factor affecting HRQOL (p<0.01). MCS was extracted with FES as a factor (p=0.046).
Conclusion
A rehabilitation intervention incorporating patient education in osteoarthritis of the knee showed improvement in HRQOL and may be useful for improving depression, fear of falling, and instrumental ADL.
Figure
Reference
-
1. Curry ZA, Beling A, Borg-Stein J. Knee osteoarthritis in midlife women: unique considerations and comprehensive management. Menopause. 2022; 29:748–55.
Article2. Yoshimura N, Muraki S, Oka H, Mabuchi A, En-Yo Y, Yoshida M, et al. Prevalence of knee osteoarthritis, lumbar spondylosis, and osteoporosis in Japanese men and women: the research on osteoarthritis/osteoporosis against disability study. J Bone Miner Metab. 2009; 27:620–8.
Article3. Yoshimura N, Muraki S, Nakamura K, Tanaka S. Epidemiology of the locomotive syndrome: the research on osteoarthritis/osteoporosis against disability study 2005-2015. Mod Rheumatol. 2017; 27:1–7.
Article4. Park HM, Kim HS, Lee YJ. Knee osteoarthritis and its association with mental health and health-related quality of life: a nationwide cross-sectional study. Geriatr Gerontol Int. 2020; 20:379–83.
Article5. Nagai T, Tsurusaki M, Horaguchi T, Uei H, Nagaoka M. Verification of phycological factors related to health-related quality of life in elderly knee osteoarthritis: a prospective cohort study. J Orthop Sci. 2020; 25:868–73.
Article6. Meeus M, Nijs J, Hamers V, Ickmans K, Oosterwijck JV. The efficacy of patient education in whiplash associated disorders: a systematic review. Pain Physician. 2012; 15:351–61.7. Snyder H, Engström J. The antecedents, forms and consequences of patient involvement: a narrative review of the literature. Int J Nurs Stud. 2016; 53:351–78.
Article8. The Japanese Orthopaedic Association. Exercise therapy for knee osteoarthritis [Internet]. The Japanese Orthopaedic Association; 2003 [cited 2020 May]. Available from: https://www.joa.or.jp/public/publication/pdf/knee_osteoarthritis.pdf.9. Hashimoto M, Yasumura S, Nakano K, Kimura M, Nakamura K, Fujino K, et al. [Feasibility study of locomotion training in a home-visit preventive care program]. Nihon Ronen Igakkai Zasshi. 2012; 49:476–82. Japanese.
Article10. Sedlak CA, Doheny MO, Jones SL. Osteoporosis education programs: changing knowledge and behaviors. Public Health Nurs. 2000; 17:398–402.
Article11. Kan HS, Chan PK, Chiu KY, Yan CH, Yeung SS, Ng YL, et al. Non-surgical treatment of knee osteoarthritis. Hong Kong Med J. 2019; 25:127–33.
Article12. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957; 16:494–502.
Article13. Koshino T. [Japanese Orthopaedic Association knee scoring system]. J Jpn Orthop Assoc. 1988; 62:900–2. Japanese.14. Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol. 1990; 45:239–43.
Article15. Holbrook M, Skilbeck CE. An activities index for use with stroke patients. Age Ageing. 1983; 12:166–70.
Article16. Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982-1983; 17:37–49.
Article17. Asokan GV, Awadhalla M, Albalushi A, Al-Tamji S, Juma Z, Alasfoor M, et al. The magnitude and correlates of geriatric depression using Geriatric Depression Scale (GDS-15) - a Bahrain perspective for the WHO 2017 campaign ‘Depression - let’s talk’. Perspect Public Health. 2019; 139:79–87.
Article18. Dias FLDC, Teixeira AL, Guimarães HC, Barbosa MT, Resende EPF, Beato RG, et al. Accuracy of the 15-item Geriatric Depression Scale (GDS-15) in a community-dwelling oldest-old sample: the Pietà Study. Trends Psychiatry Psychother. 2017; 39:276–9.
Article19. Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992; 30:473–83.20. Muraki S, Akune T, Nagata K, Ishimoto Y, Yoshida M, Tokimura F, et al. Does osteophytosis at the knee predict health-related quality of life decline? A 3-year follow-up of the ROAD study. Clin Rheumatol. 2015; 34:1589–97.
Article21. Stanghelle B, Bentzen H, Giangregorio L, Pripp AH, Skelton DA, Bergland A. Effects of a resistance and balance exercise programme on physical fitness, health-related quality of life and fear of falling in older women with osteoporosis and vertebral fracture: a randomized controlled trial. Osteoporos Int 2020;31:1069-78. Erratum in: Osteoporos Int. 2020; 31:1187.
Article22. Taglietti M, Dela Bela LF, Dias JM, Pelegrinelli ARM, Nogueira JF, Batista Júnior JP, et al. Postural sway, balance confidence, and fear of falling in women with knee osteoarthritis in comparison to matched controls. PM R. 2017; 9:774–80.
Article23. Simsek H, Erkoyun E, Akoz A, Ergor A, Ucku R. Falls, fear of falling and related factors in community-dwelling individuals aged 80 and over in Turkey. Australas J Ageing. 2020; 39:e16–23.
Article24. Sayre EC, Guermazi A, Nicolaou S, Esdaile JM, Kopec JA, Singer J, et al. A whole-joint, unidimensional, irreversible, and fine-grained MRI knee osteoarthritis severity score, based on cartilage, osteophytes and meniscus (OA-COM). PLoS One. 2021; 16:e0258451.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence of Knee Osteoarthritis and Health-Related Quality of Life in Stroke Patients over 60 Years Old: A Cross-Sectional Study Using Korean National Health and Nutrition Examination Survey V
- Association of Weight Change and Physical Activity with Knee Pain and Health-Related Quality of Life in East Asian Women Aged 50 Years and Older with Knee Osteoarthritis: A Population-Based Study
- The Effects of a Self-Management Program on Physical Function and Quality of Life of Patients with Knee Osteoarthritis
- Health-related indicators according to restricted activity and health-related quality of life in osteoarthritis patients - based on Korean national health and nutrition survey
- Development and Evaluation of a Joint Health Self-management Program for the Elderly with Knee Osteoarthritis in Communities: Applying the IMB Model