J Cerebrovasc Endovasc Neurosurg.
2024 Jun;26(2):216-222. 10.7461/jcen.2023.E2023.05.006.
Management of a ruptured posterior inferior cerebellar artery (PICA) aneurysm with end-to-end in situ bypass: Case report
- Affiliations
-
- 1Department of Neurosurgery, Hospital da Restauração, Recife, Brazil
- KMID: 2556985
- DOI: http://doi.org/10.7461/jcen.2023.E2023.05.006
Abstract
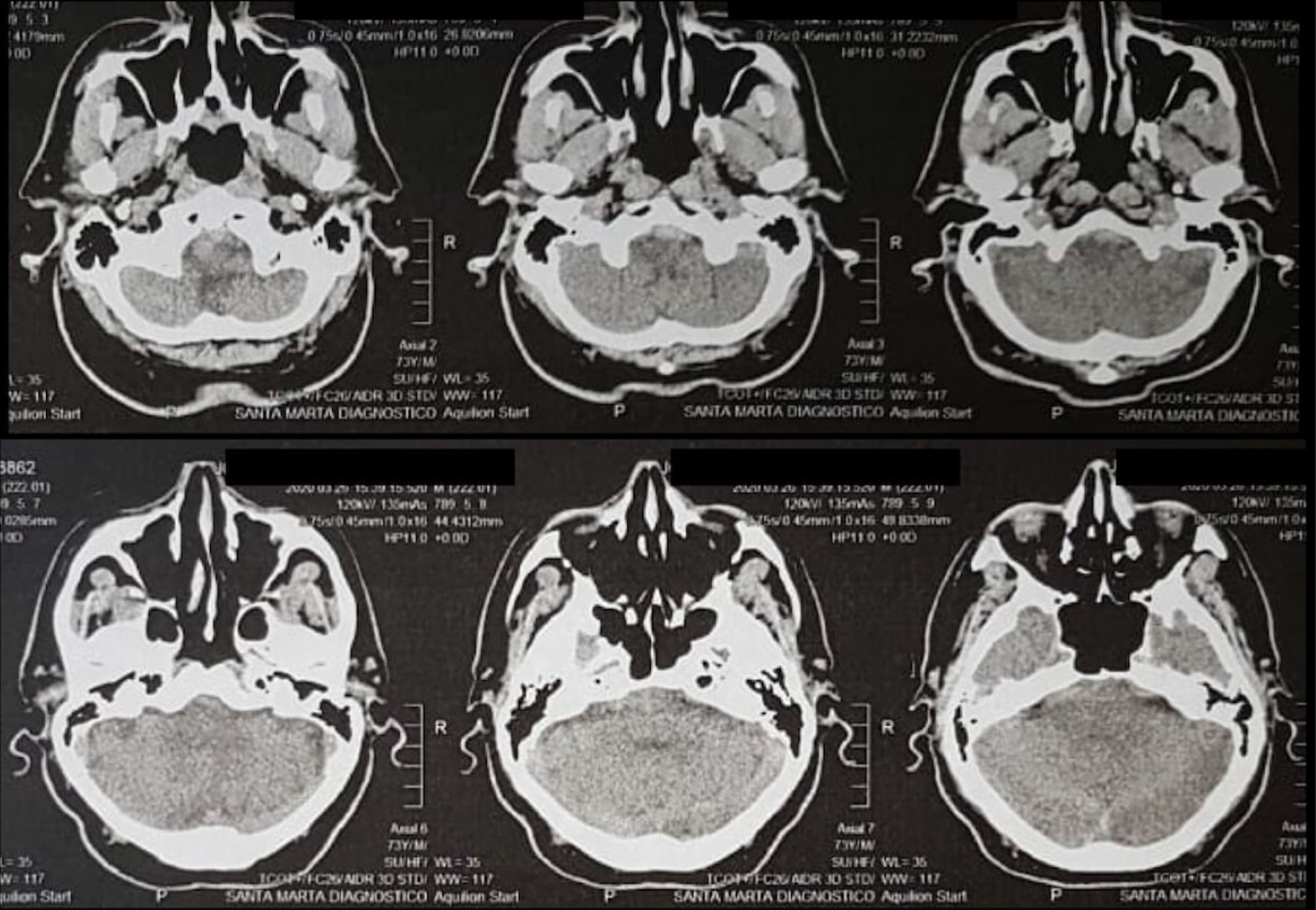
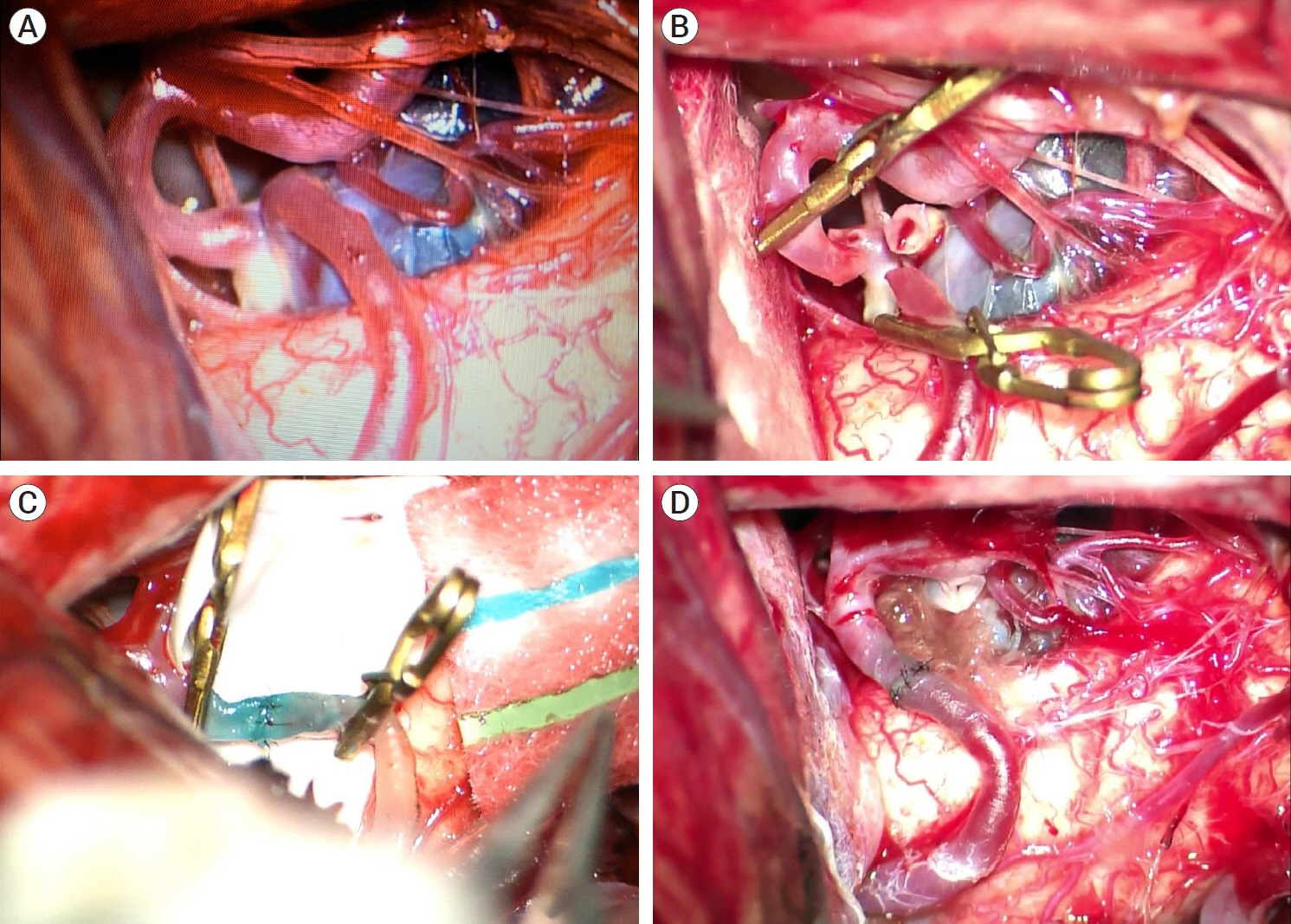
- Dissecting posterior inferior cerebellar artery (PICA) aneurysms are uncommon lesions. Their anatomy and the location of the dissection are variable, however, they usually occurs at the origin of the PICA. Dissecting PICA aneurysms generally have non-vascular morphology involving an entire segment of the artery and cannot be cut. Nevertheless, the detection of these vascular lesions has increased latterly, so it is necessary to recognize it and take the appropriate management modalities for these injuries. In this report, we describe a case of a 73-year-old male patient, who presented a history of severe headache, associated with neck stiffness, nausea, vomiting, dizziness, hypoactivity, mental confusion, and walking difficulty. Radiographic investigation with brain computed tomography (CT) showed mild bleeding in a pre-medullary and pre-pontine cistern, and cerebral angiogram showed a dissecting PICA aneurysm. Despite being a challenging treatment, microsurgery management was the chosen modality. It was performed an end-to-end anastomosis between the p2/p3 segments, showing to be effective with good clinical and radiographic outcomes. We discussed an unusual case, reviewing the current literature on clinical presentations, the angiographic characteristics of the dissecting aneurysms of PICA, and evaluating the clinical and angiographic results of patients undergoing microsurgical treatment.
Figure
Reference
-
1. Abla AA, McDougall CM, Breshears JD, Lawton MT. Intracranial-to-intracranial bypass for posterior inferiorcerebellar artery aneurysms: Options, technical challenges, and results in 35 patients. J Neurosurg. 2016; May. 124(5):1275–86.2. Benet A, Montemurro N, Lawton MT. Management of a ruptured posterior Inferior cerebelar artery (PICA) aneurysm with PICA-PICA in situ bypass and trapping: 3-dimensional operative video. Oper Neurosurg (Hagerstown). 2017; Jun. 13(3):400.
Article3. Bertalanffy H, Sure U, Petermeyer M, Becker R, Gilsbach JM. Management of aneurysms of the vertebral artery-posterior inferior cerebellar artery complex. Neurol Med Chir (Tokyo). 1998; 38 Suppl:93–103.
Article4. Ioannidis I, Nasis N, Andreou A. Endovascular treatment of ruptured dissecting posterior inferior cerebellar artery aneurysms. Interv Neuroradiol. 2012; Dec. 18(4):442–8.
Article5. Lanzino G. Intracranial Aneurysms (1st ed.). Torino, Italy: Edizioni Minerva Medica;2016.6. Lee SY, Sekhar LN. Treatment of aneurysms by excision or trapping with arterial reimplantation or interpositional grafting. Report of three cases. J Neurosurg. 1996; Jul. 85(1):178–85.7. Lewis SB, Chang DJ, Peace DA, Lafrentz PJ, Day AL. Distal posterior inferior cerebellar artery aneurysms: Clinical features and management. J Neurosurg. 2002; Oct. 97(4):756–66.
Article8. Liew D, Ng PY, Ng I. Surgical management of ruptured and unruptured symptomatic posterior inferior cerebellar artery aneurysms. Br J Neurosurg. 2004; Dec. 18(6):608–12.
Article9. Rodríguez-Hernández A, Zador Z, Rodríguez-Mena R, Lawton MT. Distal aneurysms of intracranial arteries: application of numerical nomenclature, predilection for cerebellar arteries, and results of surgical management. World Neurosurg. 2013; Jul-Aug. 80(1-2):103–12.
Article10. Sanai N, Zador Z, Lawton MT. Bypass surgery for complex brain aneurysms: an assessment of intracranial-intracranial bypass. Neurosurgery. 2009; Oct. 65(4):670–83. discussion 683.11. Winn RH. Youmans Neurological Surgery (6th ed.). Philadelphia: Elsevier Saunders;2011.12. Yamakawa H, Kaku Y, Yoshimura S, Ohkuma A, Sakai N. Two cases of dissecting aneurysm of the distal posterior inferior cerebellar artery: Possible involvement of segmentalmediolytic arteriopathy in the pathogenesis. Clin Neurol Neurosurg. 2005; Feb. 107(2):117–22.13. Yamaki VN, Paschoal EHA, Teixeira MJ, Figueiredo EG. Surgical treatment of posterior circulation aneurysms – Anatomical study and surgical technique. Arq Bras Neurocir. 2018; 37:27–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- In Situ Intersegmental Anastomosis within a Single Artery for Treatment of an Aneurysm at the Posterior Inferior Cerebellar Artery: Closing Omega Bypass
- Medial Trunk Aneurysm of the Distal Posterior Inferior Cerebellar Artery in the Fourth Ventricle: Case Report
- Technical Consideration for Coiling of Ruptured Proximal Posterior Inferior Cerebellar Artery Aneurysm
- Posterior Inferior Cerebellar Artery Aneurysm, Mimicking Lateral Medullary Infarction: A Case Report
- The Dissecting Aneurysm of the Posterior Inferior Cerebellar Artery with Unusual Clinical Course