Kosin Med J.
2024 Jun;39(2):120-126. 10.7180/kmj.24.111.
Orbital complications of acute rhinosinusitis in adults: a 21-year experience
- Affiliations
-
- 1Department of Otorhinolaryngology, Gyeongsang National University Hospital, Jinju, Korea
- 2Institute of Health Sciences, Gyeongsang National University, Jinju, Korea
- 3Department of Otorhinolaryngology, Gyeongsang National University Changwon Hospital, Changwon, Korea
- KMID: 2556809
- DOI: http://doi.org/10.7180/kmj.24.111
Abstract
- Background
Orbital complications arising from acute rhinosinusitis (ARS) are a major concern for clinicians and serve as important warning indicators of ARS. Prompt recognition and appropriate management are crucial for preventing potential vision-threatening sequelae. Orbital complications of rhinosinusitis are markedly more common in children than in adults. The aim of this study was to investigate the clinical characteristics and treatment outcomes of orbital complications of ARS in adult patients.
Methods
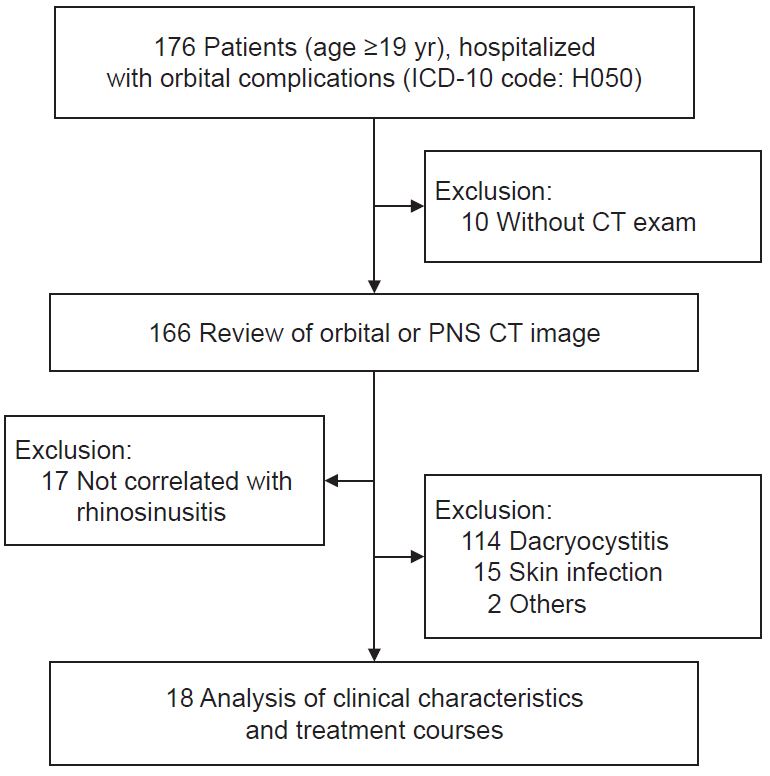
This retrospective observational cohort study analyzed the medical records of 176 patients admitted for orbital cellulitis/abscess (ICD code: H050) who underwent orbit or paranasal computed tomography from January 2001 to February 2022 at a tertiary hospital.
Results
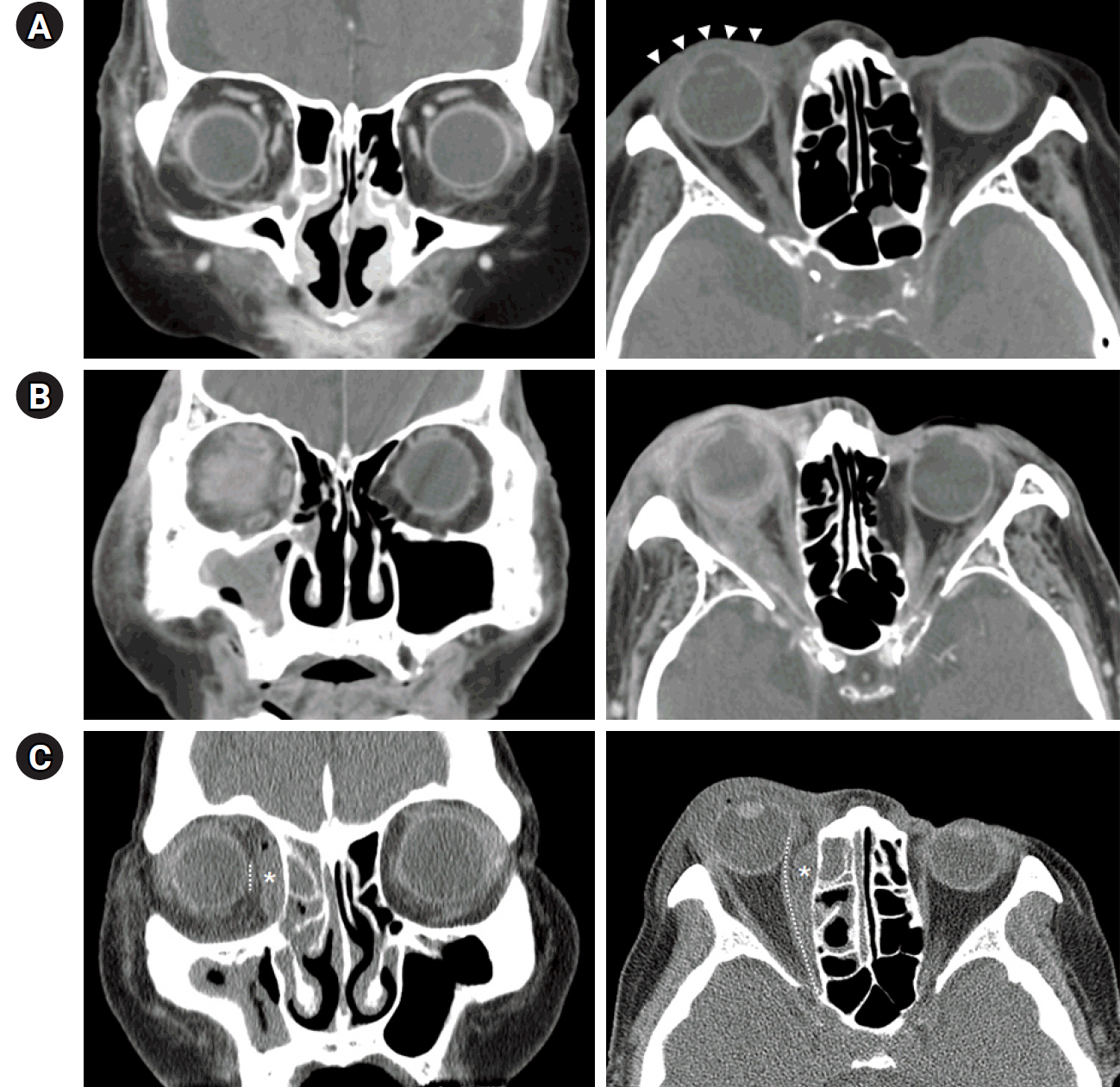
Eighteen adults with a mean age of 53.2±18.9 years were diagnosed with orbital complications due to ARS: five (27.8%) had preseptal cellulitis, eight (44.4%) had orbital cellulitis, and five (27.8%) had subperiosteal orbital abscess. None of the patients had an orbital abscess or cavernous sinus thrombosis. All patients had unilateral orbital complications (7 right and 11 left) and were managed with intravenous antibiotics for an average of 10.3±6.6 days. Five patients with subperiosteal orbital abscesses underwent intranasal endoscopic drainage at an average of 1.4±1.9 days after admission, while two patients required additional external drainage. Complete recovery was observed in all patients.
Conclusions
Conservative antimicrobial therapy can be effective for treating orbital complications from ARS, and not all adult patients require immediate surgical intervention for subperiosteal abscesses. Nonetheless, careful monitoring is essential, and an ophthalmologist must check patients’ visual acuity to prevent irreversible blindness.
Keyword
Figure
Reference
-
References
1. Fokkens WJ, Lund VJ, Hopkins C, Hellings PW, Kern R, Reitsma S, et al. European position paper on rhinosinusitis and nasal polyps 2020. Rhinology. 2020; 58(Suppl S29):1–464.2. DeBoer DL, Kwon E. Acute sinusitis [Internet]. StatPearls Publishing;2023. [cited 2024 May 11]. https://pubmed.ncbi.nlm.nih.gov/31613481/.3. Aring AM, Chan MM. Current concepts in adult acute rhinosinusitis. Am Fam Physician. 2016; 94:97–105.4. Hoffmans R, Wagemakers A, van Drunen C, Hellings P, Fokkens W. Acute and chronic rhinosinusitis and allergic rhinitis in relation to comorbidity, ethnicity and environment. PLoS One. 2018; 13:e0192330.5. Chandler JR, Langenbrunner DJ, Stevens ER. The pathogenesis of orbital complications in acute sinusitis. Laryngoscope. 1970; 80:1414–28.6. Kim YJ, Min YG. Orbital complications of rhinosinusitis: characteristics in pediatric patients. J Rhinol. 2000; 7:109–12.7. Kim JW, Ahn SK, Jeon SY, Kim JP, Kim BG. Clinical analysis of orbital subperiosteal abscesses as a complication of acute sinusitis. Korean J Otolaryngol-Head Neck Surg. 2003; 46:575–9.8. Chung SW, Cho JG, Lee SH, Lee SH, Hwang SJ, Lee HM. Clinical analysis of orbital subperiosteal abscess. J Rhinol. 2005; 12:50–4.9. Oh JH, Cho MJ, Mo JY, Song JW, Kahng H, Kim HJ. Clinical analysis of orbital complications of acute sinusitis according to age. J Rhinol. 2006; 13:22–5.10. Lim GH, Kim JS, Kim YD, Ye MK, Shin SH. Orbital complications of sinusitis: a retrospective clinical analysis. J Rhinol. 2009; 16:35–8.11. Dankbaar JW, van Bemmel AJ, Pameijer FA. Imaging findings of the orbital and intracranial complications of acute bacterial rhinosinusitis. Insights Imaging. 2015; 6:509–18.12. Snidvongs K, Chitsuthipakorn W, Akarapas C, Aeumjaturapat S, Chusakul S, Kanjanaumporn J, et al. Risk factors of orbital complications in outpatients presenting with severe rhinosinusitis: a case-control study. Clin Otolaryngol. 2021; 46:587–93.13. Zhao EE, Koochakzadeh S, Nguyen SA, Yoo F, Pecha P, Schlosser RJ. Orbital complications of acute bacterial rhinosinusitis in the pediatric population: a systematic review and meta-analysis. Int J Pediatr Otorhinolaryngol. 2020; 135:110078.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Orbital Complications of Rhinosinusitis: Characteristics in Pediatric Patients
- Clinical Characteristics and Treatment of Fungal Rhinosinusitis
- Clinical Analysis of Orbital Complications of Acute Sinusitis according to Age
- A Case of Periorbital Necrotizing Fasciitis Occurred in Patient with Acute Rhinosinusitis
- Clinical Review of Orbital Complications Caused by Paranasal Sinusitis: 10-Years Experience