Kosin Med J.
2024 Mar;39(1):75-79. 10.7180/kmj.23.132.
Surgical management of giant adrenal myelolipoma using a modified Makuuchi incision: a case report
- Affiliations
-
- 1Department of Urology, Pusan National University Hospital, Busan, Korea
- KMID: 2556802
- DOI: http://doi.org/10.7180/kmj.23.132
Abstract
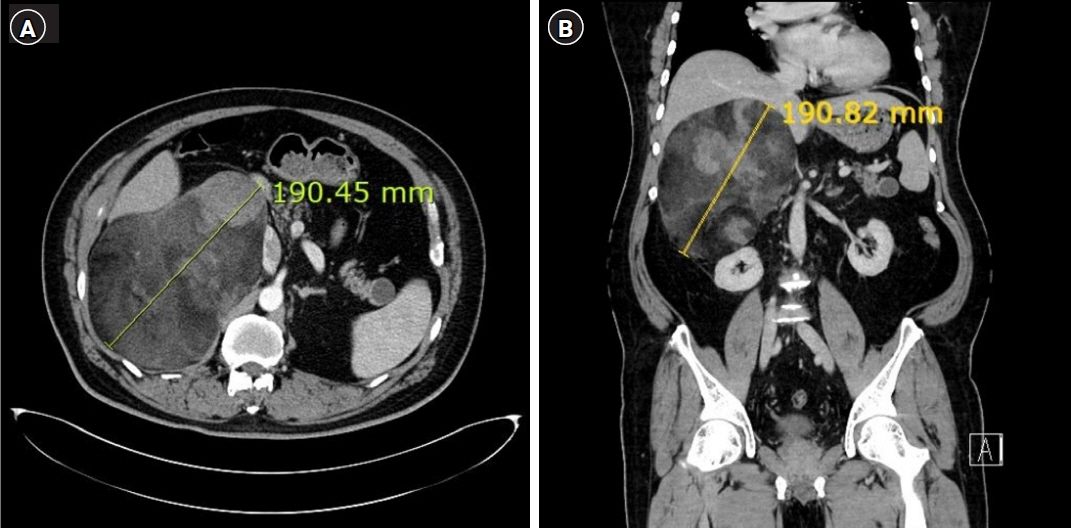
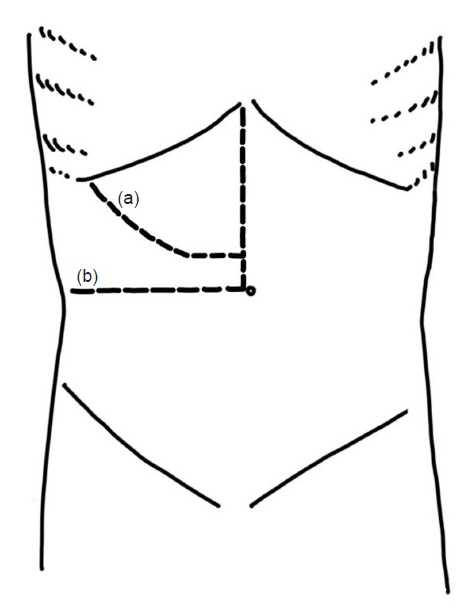
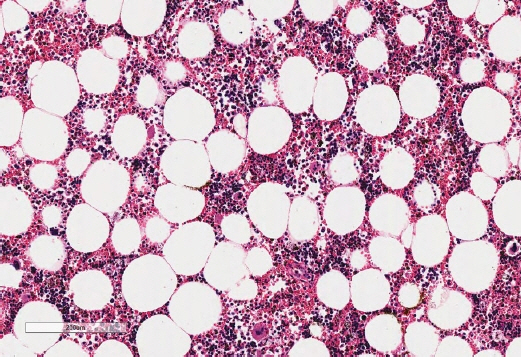
- Giant adrenal myelolipomas are rare, benign, and hormonally inactive tumors. We present the case of a 53-year-old man with a 19-cm retroperitoneal mass, initially suspected to be a retroperitoneal liposarcoma, angiomyolipoma, or adrenal myelolipoma. After conducting endocrine assessments, which were within normal ranges, we decided to perform surgical excision using a modified Makuuchi incision. The tumor was successfully removed, and the final pathological examination confirmed the diagnosis of adrenal myelolipoma. The patient was discharged with no complications and remained without disease recurrence or distant metastasis as of 1 year postoperatively. In conclusion, giant myelolipomas are rare and cause symptoms owing to their large size. Surgical removal is recommended for large or symptomatic myelolipomas. The modified Makuuchi incision allows efficient and safe tumor removal in open surgery for giant myelolipomas.
Keyword
Figure
Reference
-
References
1. Calissendorff J, Juhlin CC, Sundin A, Bancos I, Falhammar H. Adrenal myelolipomas. Lancet Diabetes Endocrinol. 2021; 9:767–75.2. Alvarez JF, Goldstein L, Samreen N, Beegle R, Carter C, Shaw A, et al. Giant adrenal myelolipoma. J Gastrointest Surg. 2014; 18:1716–8.3. Cochetti G, Paladini A, Boni A, Silvi E, Tiezzi A, De Vermandois JAR, et al. Robotic treatment of giant adrenal myelolipoma: a case report and review of the literature. Mol Clin Oncol. 2019; 10:492–6.4. Im SI. How to write case reports in medicine. Kosin Med J. 2022; 37:102–6.5. Lee HS. Ethical issues in clinical research and publication. Kosin Med J. 2022; 37:278–82.6. Pokrovskaya A, Tarzimanova A, Vetluzhskaya M, Podzolkov V. Rare case of symptomatic adrenal myelolipoma. BMJ Case Rep. 2021; 14:e245181.7. Mhammedi WA, Ouslim H, Ouraghi A, Irzi M, Elhoumaidi A, Elhoumaidi A, et al. Adrenal myelolipoma: from tumorigenesis to management. Pan Afr Med J. 2019; 34:180.8. Nakayama Y, Matayoshi N, Akiyama M, Sawatsubashi Y, Nagata J, Hisaoka M, et al. Giant adrenal myelolipoma in a patient without endocrine disorder: a case report and a review of the literature. Case Rep Surg. 2018; 2018:4854368.9. Vigutto G, Lauro A, Vaccari S, Pirini MG, Diegoli M, D'Andrea V, et al. Giant retroperitoneal myelolipoma: an unusual diagnostic GI challenge-case report and review of the literature. Dig Dis Sci. 2019; 64:3431–5.10. Decmann A, Perge P, Toth M, Igaz P. Adrenal myelolipoma: a comprehensive review. Endocrine. 2018; 59:7–15.11. Alemanno G, Bergamini C, Prosperi P, Valeri A. Adrenalectomy: indications and options for treatment. Updates Surg. 2017; 69:119–25.12. Fernandes GC, Gupta RK, Kandalkar BM. Giant adrenal myelolipoma. Indian J Pathol Microbiol. 2010; 53:325–6.13. Uludag M, Aygun N, Işgor A. Surgical indications and techniques for adrenalectomy. Sisli Etfal Hastan Tip Bul. 2020; 54:8–22.14. Makuuchi M, Kawasaki S. Surgical management of malignant liver disease. In: Lygidakis N, Makuuchi M, edtiors. Pitfalls and complications in the diagnosis and management of hepatobiliary and pancreatic diseases. Georg Thieme Verlag; 1993. p. 86-88.15. Chang SB, Palavecino M, Wray CJ, Kishi Y, Pisters PW, Vauthey JN, et al. Modified Makuuchi incision for foregut procedures. Arch Surg. 2010; 145:281–4.16. Bokka SH, Sreenivasan Kodakkattil S, Manikandan R, Lalgudi Narayanan D, M H, Kalra S, et al. Usage of modified makuuchi incision for surgical management of complex renal and adrenal lesions. Cureus. 2020; 12:e11012.17. Sonmez K, Turkyilmaz Z, Karabulut R, Kaya C, Polat F, Atan A. Use of modified Makuuchi incision for surgical treatment of abdominal tumor in children. Arch Esp Urol. 2022; 75:282–6.