J Korean Neurosurg Soc.
2024 Jul;67(4):411-417. 10.3340/jkns.2023.0184.
The Usefulness of Extradural Anterior Clinoidectomy for Lower-Lying Posterior Communicating Artery Aneurysms : A Cadaveric Study
- Affiliations
-
- 1Department of Neurosurgery, Chungnam National University Sejong Hospital, Sejong, Korea
- 2Department of Neurosurgery, College of Medicine, Hanyang University, Seoul, Korea
- 3Department of Neurosurgery, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea
- 4Department of Anatomy, College of Korean Medicine, Dongshin University, Naju, Korea
- KMID: 2556738
- DOI: http://doi.org/10.3340/jkns.2023.0184
Abstract
Objective
: To confirm the usefulness of the extradural anterior clinoidectomy during the clipping of a lower riding posterior communicating artery (PCoA) aneurysm through cadaver dissection.
Methods
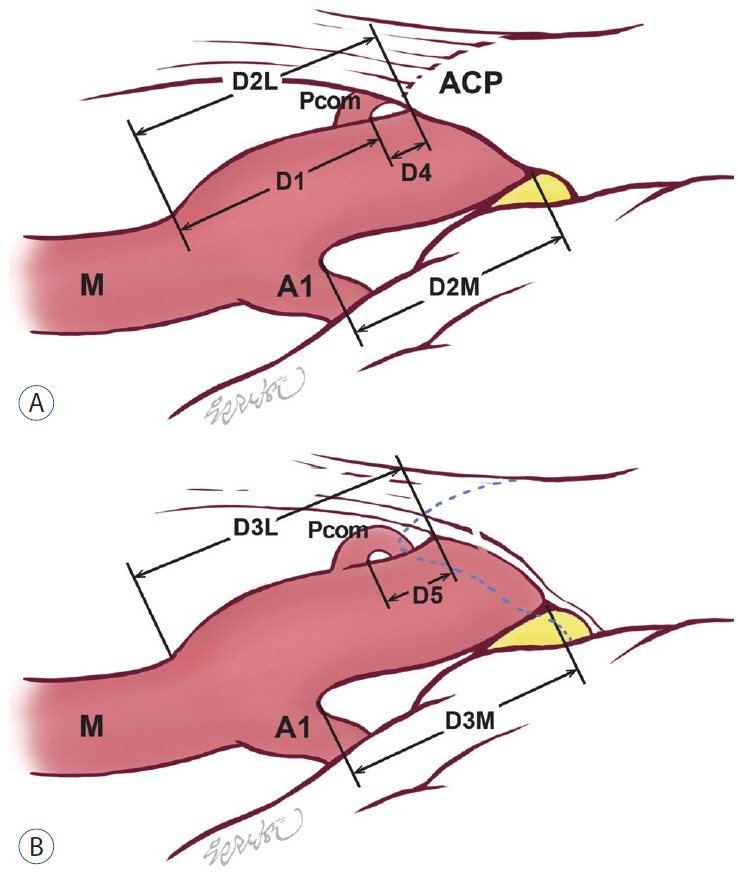
: Anatomic measurements of 12 adult cadaveric heads (24 sides total) were performed to compare the microsurgical exposure of the PCoA and internal carotid artery (ICA) before and after clinoidectomy. A standard pterional craniotomy and transsylvian approach were performed in all cadavers. The distance from the ICA bifurcation to the origin of PCoA (D1), pre-anterior clinoidectomy distance from the ICA bifurcation to tentorium (D2), post-anterior clinoidectomy distance from the ICA bifurcation to tentorium (D3), pre-anterior clinoidectomy distance from the tentorium to the origin of PCoA (D4) and post-anterior clinoidectomy distance from the tentorium to the origin of PCoA (D5) and the distance of the ICA obtained after anterior clinoidectomy (D6) were measured. We measured the precise thickness of the blade for the Yasargil clip with a digital precision ruler to confirm the usefulness of the extradural anterior clinoidectomy.
Results
: Twenty-four sites were dissected from 12 cadavers. The age of the cadavers was 79.83±6.25 years. The number of males was the same as the females. The space from the proximal origin of the PCoA to the preclinoid-tentorium (D4) was 1.45±1.08 mm (max, 4.01; min, 0.56). After the clinoidectomy, the space from the proximal origin of the PCoA to the postclinoid-tentorium (D5) was 3.612±1.15 mm (max, 6.14; min, 1.83). The length (D6) of the exposed proximal ICA after the extradural clinoididectomy was 2.17±1.04 mm on the lateral side and 2.16±0.89 mm on the medial side. The thickness of the Yasargil clip blade used during the clipping surgery was 1.35 mm measured with a digital precision ruler.
Conclusion
: The proximal length obtained by performing an external anterior clinoidectomy is about 2 mm, sufficient for proximal control during PCoA aneurysm surgery, considering the thickness of the aneurysm clips. In a subarachnoid hemorrhage, performing an extradural anterior clinoidectomy could prevent a devastating situation during PCoA aneurysm clipping.
Figure
Reference
-
References
1. Almekhlafi MA, Al Sultan AS, Kuczynski AM, Brinjikji W, Menon BK, Hill MD, et al. Antiplatelet therapy for prevention of thromboembolic complications in coiling-only procedures for unruptured brain aneurysms. J Neurointerv Surg. 12:298–302. 2020.
Article2. Chang HS, Joko M, Song JS, Ito K, Inoue T, Nakagawa H. Ultrasonic bone curettage for optic canal unroofing and anterior clinoidectomy. Technical note. J Neurosurg. 104:621–624. 2006.
Article3. Evans JJ, Hwang YS, Lee JH. Pre- versus post-anterior clinoidectomy measurements of the optic nerve, internal carotid artery, and opticocarotid triangle: a cadaveric morphometric study. Neurosurgery. 46:1018–1021. discussion 1021-1023. 2000.
Article4. Froelich SC, Aziz KM, Levine NB, Theodosopoulos PV, van Loveren HR, Keller JT. Refinement of the extradural anterior clinoidectomy: surgical anatomy of the orbitotemporal periosteal fold. Neurosurgery. 61:179–185. discussion 185-186. 2007.5. Golnari P, Nazari P, Garcia RM, Weiss H, Shaibani A, Hurley MC, et al. Volumes, outcomes, and complications after surgical versus endovascular treatment of aneurysms in the United States (1993-2015): continued evolution versus steady-state after more than 2 decades of practice. J Neurosurg. 134:848–861. 2020.
Article6. Gonçalves Pacheco Junior M, de Melo Junior JO, André Acioly M, Mansilla Cabrera Rodrigues R, Lima Pessôa B, Fernandes RA, et al. Tailored anterior clinoidectomy: beyond the intradural and extradural concepts. Cureus. 13:e14874. 2021.7. Hwang G, Huh W, Lee JS, Villavicencio JB, Villamor RB Jr, Ahn SY, et al. Standard vs modified antiplatelet preparation for preventing thromboembolic events in patients with high on-treatment platelet reactivity undergoing coil embolization for an unruptured intracranial aneurysm: a randomized clinical trial. JAMA Neurol. 72:764–772. 2015.
Article8. Hwang G, Jung C, Park SQ, Kang HS, Lee SH, Oh CW, et al. Thromboembolic complications of elective coil embolization of unruptured aneurysms: the effect of oral antiplatelet preparation on periprocedural thromboembolic complication. Neurosurgery. 67:743–748. discussion 748. 2010.
Article9. Hwang JS, Hyun MK, Lee HJ, Choi JE, Kim JH, Lee NR, et al. Endovascular coiling versus neurosurgical clipping in patients with unruptured intracranial aneurysm: a systematic review. BMC Neurol. 12:99. 2012.
Article10. Jiang Z, Chen Y, Zeng C, Feng J, Wan Y, Zhang X. Neurosurgical clipping versus endovascular coiling for patients with intracranial aneurysms: a systematic review and meta-analysis. World Neurosurg. 138:e191–e222. 2020.
Article11. Kamide T, Burkhardt JK, Tabani H, Safaee MM, Lawton MT. Preoperative prediction of the necessity for anterior clinoidectomy during microsurgical clipping of ruptured posterior communicating artery aneurysms. World Neurosurg. 109:e493–e501. 2018.
Article12. Kim CH, Hwang G, Kwon OK, Ban SP, Chinh ND, Tjahjadi M, et al. P2Y12 reaction units threshold for implementing modified antiplatelet preparation in coil embolization of unruptured aneurysms: a prospective validation study. Radiology. 282:542–551. 2017.
Article13. Kim DW, Kang SD. Association between internal carotid artery morphometry and posterior communicating artery aneurysm. Yonsei Med J. 48:634–638. 2007.
Article14. Kim JH, Kim JM, Cheong JH, Bak KH, Kim CH. Simple anterior petroclinoid fold resection in the treatment of low-lying internal carotidposterior communicating artery aneurysms. Surg Neurol. 72:142–145. 2009.
Article15. Lee SU, Kim T, Kwon OK, Bang JS, Ban SP, Byoun HS, et al. Trends in the incidence and treatment of cerebrovascular diseases in Korea : part I. Intracranial aneurysm, intracerebral hemorrhage, and arteriovenous malformation. J Korean Neurosurg Soc. 63:56–68. 2020.
Article16. Li W, Zhu W, Wang A, Zhang G, Zhang Y, Wang K, et al. Effect of adjusted antiplatelet therapy on preventing ischemic events after stenting for intracranial aneurysms. Stroke. 52:3815–3825. 2021.
Article17. Matano F, Murai Y, Mizunari T, Yamaguchi M, Yamada T, Baba E, et al. Incision of the anterior petroclinoidal fold during clipping for securing the proximal space of an internal carotid artery-posterior communicating artery aneurysm: a technical note. Neurosurg Rev. 42:777–781. 2019.
Article18. Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, et al. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet. 360:1267–1274. 2002.
Article19. Molyneux AJ, Birks J, Clarke A, Sneade M, Kerr RS. The durability of endovascular coiling versus neurosurgical clipping of ruptured cerebral aneurysms: 18 year follow-up of the UK cohort of the International Subarachnoid Aneurysm Trial (ISAT). Lancet. 385:691–697. 2015.
Article20. Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. 366:809–817. 2005.
Article21. Nagasawa S, Kikuchi H, Kim NG, Yonekawa Y. Analysis of internal carotid-posterior communicating artery aneurysms with difficulty in clipping: with special reference to radiometry. No Shinkei Geka. 16:959–964. 1988.22. Niibo T, Takizawa K, Sakurai J, Takebayashi S, Koizumi H, Kobayashi T, et al. Prediction of the difficulty of proximal vascular control using 3DCTA for the surgical clipping of internal carotid artery-posterior communicating artery aneurysms. J Neurosurg. 134:1165–1172. 2020.
Article23. Nossek E, Setton A, Dehdashti AR, Chalif DJ. Anterior petroclinoid fold fenestration: an adjunct to clipping of postero-laterally projecting posterior communicating aneurysms. Neurosurg Rev. 37:637–641. 2014.
Article24. Ochiai C, Wakai S, Inou S, Nagai M. Preoperative angiographical prediction of the necessity to removal of the anterior clinoid process in internal carotid-posterior communicating artery aneurysm surgery. Acta Neurochir (Wien). 99:117–121. 1989.
Article25. Park SK, Shin YS, Lim YC, Chung J. Preoperative predictive value of the necessity for anterior clinoidectomy in posterior communicating artery aneurysm clipping. Neurosurgery. 65:281–285. discussion 285-286. 2009.
Article26. Romani R, Elsharkawy A, Laakso A, Kangasniemi M, Hernesniemi J. Tailored anterior clinoidectomy through the lateral supraorbital approach: experience with 82 consecutive patients. World Neurosurg. 77:512–517. 2012.
Article27. Salgado López L, Muñoz Hernández F, Asencio Cortés C, Tresserras Ribó P, Álvarez Holzapfel MJ, Molet Teixidó J. Extradural anterior clinoidectomy in the management of parasellar meningiomas: analysis of 13 years of experience and literature review. Neurocirugia (Astur : Engl Ed). 29:225–232. 2018.
Article28. Son HE, Park MS, Kim SM, Jung SS, Park KS, Chung SY. The avoidance of microsurgical complications in the extradural anterior clinoidectomy to paraclinoid aneurysms. J Korean Neurosurg Soc. 48:199–206. 2010.
Article29. Tayebi Meybodi A, Lawton MT, Yousef S, Guo X, González Sánchez JJ, Tabani H, et al. Anterior clinoidectomy using an extradural and intradural 2-step hybrid technique. J Neurosurg. 130:238–247. 2018.
Article30. Thiarawat P, Jahromi BR, Kozyrev DA, Intarakhao P, Teo MK, ChoqueVelasquez J, et al. Microneurosurgical management of posterior communicating artery aneurysm: a contemporary series from Helsinki. World Neurosurg. 101:379–388. 2017.
Article31. Yonekawa Y, Ogata N, Imhof HG, Olivecrona M, Strommer K, Kwak TE, et al. Selective extradural anterior clinoidectomy for supra- and parasellar processes. Technical note. J Neurosurg. 87:636–642. 1997.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Pterional Approach and Extradural Anterior Clinoidectomy to Clip Paraclinoid Aneurysms
- The Avoidance of Microsurgical Complications in the Extradural Anterior Clinoidectomy to Paraclinoid Aneurysms
- Microsurgical anatomy of the Anterior Cerebral-anterior Communicating Artery
- Clinical Analysis of the Pattern of Anterior-Posterior Circulation in Patients with Posterior Communicating Artery Aneurysm
- Transposition of Anterior Choroidal Artery and Posterior Communicating Artery Origin