J Korean Neurosurg Soc.
2024 Jul;67(4):385-396. 10.3340/jkns.2023.0199.
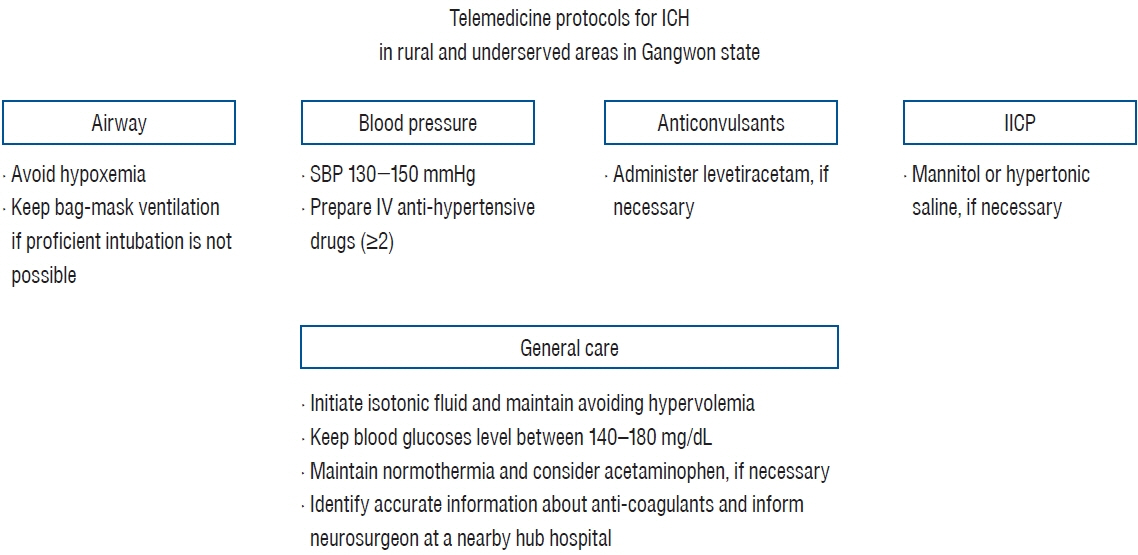
Telemedicine Protocols for the Management of Patients with Acute Spontaneous Intracerebral Hemorrhage in Rural and Medically Underserved Areas in Gangwon State : Recommendations for Doctors with Less Expertise at Local Emergency Rooms
- Affiliations
-
- 1Department of Neurosurgery, Kangwon National University Hospital, Chuncheon, Korea
- 2Department of Neurosurgery, Gangneung Asan Hospital, Gangneung, Korea
- 3Department of Neurosurgery, Yonsei University Wonju College of Medicine, Wonju, Korea
- 4Department of Neurosurgery, Hallym University College of Medicine, Chuncheon, Korea
- 5Department of Convergence Software, Hallym University, Chuncheon, Korea
- 6Department of Neurology, Konkuk University Medical Center, Seoul, Korea
- 7Department of Neurosurgery, Jeju National University College of Medicine, Jeju, Korea
- 8Department of Neurosurgery, Inje University Haeundae Paik Hospital, Busan, Korea
- 9Department of Neurosurgery, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea
- 10Department of Neurosurgery, CHA Bundang Medical Center, CHA University, Seongnam, Korea
- 11Department of Neurosurgery, SMG-SNU Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2556736
- DOI: http://doi.org/10.3340/jkns.2023.0199
Abstract
- Previously, we reported the concept of a cloud-based telemedicine platform for patients with intracerebral hemorrhage (ICH) at local emergency rooms in rural and medically underserved areas in Gangwon state by combining artificial intelligence and remote consultation with a neurosurgeon. Developing a telemedicine ICH treatment protocol exclusively for doctors with less ICH expertise working in emergency rooms should be part of establishing this system. Difficulties arise in providing appropriate early treatment for ICH in rural and underserved areas before the patient is transferred to a nearby hub hospital with stroke specialists. This has been an unmet medical need for decade. The available reporting ICH guidelines are realistically possible in university hospitals with a well-equipped infrastructure. However, it is very difficult for doctors inexperienced with ICH treatment to appropriately select and deliver ICH treatment based on the guidelines. To address these issues, we developed an ICH telemedicine protocol. Neurosurgeons from four university hospitals in Gangwon state first wrote the guidelines, and professors with extensive ICH expertise across the country revised them. Guidelines and recommendations for ICH management were described as simply as possible to allow more doctors to use them easily. We hope that our effort in developing the telemedicine protocols will ultimately improve the quality of ICH treatment in local emergency rooms in rural and underserved areas in Gangwon state.
Figure
Reference
-
References
1. An SJ, Kim TJ, Yoon BW. Epidemiology, risk factors, and clinical features of intracerebral hemorrhage: an update. J Stroke. 19:3–10. 2017.
Article2. Angileri FF, Cardali S, Conti A, Raffa G, Tomasello F. Telemedicine-assisted treatment of patients with intracerebral hemorrhage. Neurosurg Focus. 32:E6. 2012.
Article3. Arima H, Wang JG, Huang Y, Heeley E, Skulina C, Parsons MW, et al. Significance of perihematomal edema in acute intracerebral hemorrhage: the INTERACT trial. Neurology. 73:1963–1968. 2009.
Article4. Balami JS, Buchan AM. Complications of intracerebral haemorrhage. Lancet Neurol. 11:101–118. 2012.
Article5. Benghanem S, Mazeraud A, Azabou E, Chhor V, Shinotsuka CR, Claassen J, et al. Brainstem dysfunction in critically ill patients. Crit Care. 24:5. 2020.
Article6. Boehme AK, Hays AN, Kicielinski KP, Arora K, Kapoor N, Lyerly MJ, et al. Systemic inflammatory response syndrome and outcomes in intracerebral hemorrhage. Neurocrit Care. 25:133–140. 2016.
Article7. Brouwers HB, Greenberg SM. Hematoma expansion following acute intracerebral hemorrhage. Cerebrovasc Dis. 35:195–201. 2013.
Article8. Burneo JG, Fang J, Saposnik G; Investigators of the Registry of the Canadian Stroke Network. Impact of seizures on morbidity and mortality after stroke: a Canadian multi-centre cohort study. Eur J Neurol. 17:52–58. 2010.
Article9. Carney N, Totten AM, Cheney T, Jungbauer R, Neth MR, Weeks C, et al. Prehospital airway management: a systematic review. Prehosp Emerg Care. 26:716–727. 2022.
Article10. Charidimou A, Imaizumi T, Moulin S, Biffi A, Samarasekera N, Yakushiji Y, et al. Brain hemorrhage recurrence, small vessel disease type, and cerebral microbleeds: a meta-analysis. Neurology. 89:820–829. 2017.
Article11. Chen H, Song Z, Dennis JA. Hypertonic saline versus other intracranial pressure-lowering agents for people with acute traumatic brain injury. Cochrane Database Syst Rev. 12:CD010904. 2019.
Article12. Cho KC, Kim H, Suh SH. Trends in mortality from hemorrhagic stroke in Korea from 2012 to 2020. Neurointervention. 17:87–92. 2022.
Article13. Claassen J, Jetté N, Chum F, Green R, Schmidt M, Choi H, et al. Electrographic seizures and periodic discharges after intracerebral hemorrhage. Neurology. 69:1356–1365. 2007.
Article14. Dastur CK, Yu W. Current management of spontaneous intracerebral haemorrhage. Stroke Vasc Neurol. 2:21–29. 2017.
Article15. De Herdt V, Dumont F, Hénon H, Derambure P, Vonck K, Leys D, et al. Early seizures in intracerebral hemorrhage: incidence, associated factors, and outcome. Neurology. 77:1794–1800. 2011.16. Doria JW, Forgacs PB. Incidence, implications, and management of seizures following ischemic and hemorrhagic stroke. Curr Neurol Neurosci Rep. 19:37. 2019.
Article17. Fernando SM, Qureshi D, Talarico R, Tanuseputro P, Dowlatshahi D, Sood MM, et al. Intracerebral hemorrhage incidence, mortality, and association with oral anticoagulation use: a population study. Stroke. 52:1673–1681. 2021.
Article18. Gravesteijn BY, Sewalt CA, Nieboer D, Menon DK, Maas A, Lecky F, et al. Tracheal intubation in traumatic brain injury: a multicentre prospective observational study. Br J Anaesth. 125:505–517. 2020.19. Greenberg SM, Ziai WC, Cordonnier C, Dowlatshahi D, Francis B, Goldstein JN, et al. 2022 guideline for the management of patients with spontaneous intracerebral hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke. 53:e282–e361. 2022.
Article20. Haapaniemi E, Strbian D, Rossi C, Putaala J, Sipi T, Mustanoja S, et al. The CAVE score for predicting late seizures after intracerebral hemorrhage. Stroke. 45:1971–1976. 2014.
Article21. Health Insurance Review & Assessment Service : Analysis of Customized Healthcare Status by Local Governments. Wonju : Health Insurance Review & Assessment Service, 2023.22. Hoh BL, Ko NU, Amin-Hanjani S, Chou SH-Y, Cruz-Flores S, Dangayach NS, et al. 2023 guideline for the management of patients with aneurysmal subarachnoid hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke. 54:e314–e370. 2023.
Article23. Hong KS, Bang OY, Kang DW, Yu KH, Bae HJ, Lee JS, et al. Stroke statistics in Korea: part I. Epidemiology and risk factors: a report from the Korean Stroke Society and clinical research center for stroke. J Stroke. 15:2–20. 2013.
Article24. Hong KS, Bang OY, Kim JS, Heo JH, Yu KH, Bae HJ, et al. Stroke statistics in Korea: part II stroke awareness and acute stroke care, a report from the Korean Stroke Society and clinical research center for stroke. J Stroke. 15:67–77. 2013.
Article25. Im SI. What regional disparity trends of cardiovascular mortality have changed in 2019 compared to the 1980s? Korean Circ J. 52:844–846. 2022.
Article26. Jin Z, Chen Y. Telemedicine in the Cloud Era: prospects and challenges. Ieee Pervasive Comput. 14:54–61. 2015.
Article27. Jun HS, Yang K, Kim J, Jeon JP, Ahn JH, Lee SJ, et al. Development of cloud-based telemedicine platform for acute intracerebral hemorrhage in Gangwon-do : concept and protocol. J Korean Neurosurg Soc. 66:488–493. 2023.
Article28. Karhunen H, Jolkkonen J, Sivenius J, Pitkänen A. Epileptogenesis after experimental focal cerebral ischemia. Neurochem Res. 30:1529–1542. 2005.
Article29. Kim E, Baek J, Kim M, Lee H, Bae JW, Kim HC. Trends in regional disparity in cardiovascular mortality in Korea, 1983-2019. Korean Circ J. 52:829–843. 2022.
Article30. Kim JE, Ko SB, Kang HS, Seo DH, Park SQ, Sheen SH, et al. Clinical practice guidelines for the medical and surgical management of primary intracerebral hemorrhage in Korea. J Korean Neurosurg Soc. 56:175–187. 2014.
Article31. Koenig MA, Bryan M, Lewin JL 3rd, Mirski MA, Geocadin RG, Stevens RD. Reversal of transtentorial herniation with hypertonic saline. Neurology. 70:1023–1029. 2008.
Article32. Kongwad LI, Hegde A, Menon G, Nair R. Influence of admission blood glucose in predicting outcome in patients with spontaneous intracerebral hematoma. Front Neurol. 9:725. 2018.
Article33. Kuohn LR, Witsch J, Steiner T, Sheth KN, Kamel H, Navi BB, et al. Early deterioration, hematoma expansion, and outcomes in deep versus lobar intracerebral hemorrhage: the FAST trial. Stroke. 53:2441–2448. 2022.
Article34. Lee SU, Kim T, Kwon OK, Bang JS, Ban SP, Byoun HS, et al. Trends in the incidence and treatment of cerebrovascular diseases in Korea : part I. Intracranial aneurysm, intracerebral hemorrhage, and arteriovenous malformation. J Korean Neurosurg Soc. 63:56–68. 2020.
Article35. Li Z, You M, Long C, Bi R, Xu H, He Q, et al. Hematoma expansion in intracerebral hemorrhage: an update on prediction and treatment. Front Neurol. 11:702. 2020.
Article36. Liu J, Xu H, Chen Q, Zhang T, Sheng W, Huang Q, et al. Prediction of hematoma expansion in spontaneous intracerebral hemorrhage using support vector machine. EBioMedicine. 43:454–459. 2019.
Article37. May N, Anderson K. Towards evidence based emergency medicine: best BETs from the Manchester Royal Infirmary. BET 3: suxamethonium (succinylcholine) for RSI and intubation in head injury. Emerg Med J. 29:511–514. 2012.
Article38. McGurgan IJ, Ziai WC, Werring DJ, Al-Shahi Salman R, Parry-Jones AR. Acute intracerebral haemorrhage: diagnosis and management. Pract Neurol. 21:128–136. 2020.
Article39. Mehta A, Zusman BE, Choxi R, Shutter LA, Yassin A, Antony A, et al. Seizures after intracerebral hemorrhage: incidence, risk factors, and impact on mortality and morbidity. World Neurosurg. 112:e385–e392. 2018.
Article40. Morgenstern LB, Hemphill JC 3rd, Anderson C, Becker K, Broderick JP, Connolly ES Jr, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 41:2108–2129. 2010.
Article41. Mullen MT, Kasner SE, Messé SR. Seizures do not increase in-hospital mortality after intracerebral hemorrhage in the nationwide inpatient sample. Neurocrit Care. 19:19–24. 2013.
Article42. Murthy SB, Moradiya Y, Dawson J, Lees KR, Hanley DF, Ziai WC, et al. Perihematomal edema and functional outcomes in intracerebral hemorrhage: influence of hematoma volume and location. Stroke. 46:3088–3092. 2015.
Article43. Naidech AM, Garg RK, Liebling S, Levasseur K, Macken MP, Schuele SU, et al. Anticonvulsant use and outcomes after intracerebral hemorrhage. Stroke. 40:3810–3815. 2009.
Article44. National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 333:1581–1587. 1995.45. Passero S, Rocchi R, Rossi S, Ulivelli M, Vatti G. Seizures after spontaneous supratentorial intracerebral hemorrhage. Epilepsia. 43:1175–1180. 2002.
Article46. Rangel-Castilla L, Gopinath S, Robertson CS. Management of intracranial hypertension. Neurol Clin. 26:521–541, x. 2008.
Article47. Robinson N, Clancy M. In patients with head injury undergoing rapid sequence intubation, does pretreatment with intravenous lignocaine/lidocaine lead to an improved neurological outcome? A review of the literature. Emerg Med J. 18:453–457. 2001.
Article48. Seder DB, Riker RR, Jagoda A, Smith WS, Weingart SD. Emergency neurological life support: airway, ventilation, and sedation. Neurocrit Care. 17 Suppl 1:S4–S20. 2012.
Article49. Steiner T, Al-Shahi Salman R, Beer R, Christensen H, Cordonnier C, Csiba L, et al. European Stroke Organisation (ESO) guidelines for the management of spontaneous intracerebral hemorrhage. Int J Stroke. 9:840–855. 2014.
Article50. Stiell IG, Nesbitt LP, Pickett W, Munkley D, Spaite DW, Banek J, et al. The OPALS major trauma study: impact of advanced life-support on survival and morbidity. CMAJ. 178:1141–1152. 2008.
Article51. Susanto M, Riantri I. Optimal dose and concentration of hypertonic saline in traumatic brain injury: a systematic review. Medeni Med J. 37:203–211. 2022.
Article52. Tan G, Zhou J, Yuan D, Sun S. Formula for use of mannitol in patients with intracerebral haemorrhage and high intracranial pressure. Clin Drug Investig. 28:81–87. 2008.
Article53. Tarwade P, Smischney NJ. Endotracheal intubation sedation in the intensive care unit. World J Crit Care Med. 11:33–39. 2022.
Article54. Tran QK, Bzhilyanskaya V, Lurie T, Fairchild M, Rehan MA, Rashid A, et al. Phenytoin prophylaxis and functional outcomes following spontaneous intracerebral hemorrhage: a systematic review and meta-analysis. J Neurol Sci. 429:117624. 2021.
Article55. van der Jagt M. Fluid management of the neurological patient: a concise review. Crit Care. 20:126. 2016.
Article56. Wagner I, Hauer EM, Staykov D, Volbers B, Dörfler A, Schwab S, et al. Effects of continuous hypertonic saline infusion on perihemorrhagic edema evolution. Stroke. 42:1540–1545. 2011.
Article57. Wilkinson DA, Pandey AS, Thompson BG, Keep RF, Hua Y, Xi G. Injury mechanisms in acute intracerebral hemorrhage. Neuropharmacology. 134(Pt B):240–248. 2018.
Article58. Wilson BR, Bruno J, Duckwitz M, Akers N, Jeanmonod D, Jeanmonod R. Prehospital end-tidal CO2 as an early marker for transfusion requirement in trauma patients. Am J Emerg Med. 45:254–257. 2021.
Article59. Yang J, Arima H, Wu G, Heeley E, Delcourt C, Zhou J, et al. Prognostic significance of perihematomal edema in acute intracerebral hemorrhage: pooled analysis from the intensive blood pressure reduction in acute cerebral hemorrhage trial studies. Stroke. 46:1009–1013. 2015.
Article60. Zheng J, Yu Z, Ma L, Guo R, Lin S, You C, et al. Association between blood glucose and functional outcome in intracerebral hemorrhage: a systematic review and meta-analysis. World Neurosurg. 114:e756–e765. 2018.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development of Cloud-Based Telemedicine Platform for Acute Intracerebral Hemorrhage in Gangwon-do : Concept and Protocol
- Improvement of supportive systems for medically-underserved areas
- Current State of u-Health and Its Developmental Strategies in Korea
- Strategies to enhance public health doctor system in South Korea
- Influence of cognitive function and social support on health-related quality of life of elderly men in partial medically underserved rural areas: A cross-sectional study