J Korean Med Sci.
2024 Jun;39(24):e189. 10.3346/jkms.2024.39.e189.
Antibiotics for Pediatric Patients With Laryngotracheobronchitis in Korea: A Nationwide Study Based on Administrative Data
- Affiliations
-
- 1Department of Pediatrics, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Pediatrics, Bucheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Pediatrics, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4The Vaccine Bio Research Institute, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 5Department of Pediatrics, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2556685
- DOI: http://doi.org/10.3346/jkms.2024.39.e189
Abstract
- Background
Antimicrobial resistance (AMR) is an important global public health concern in adults and children. Laryngotracheobronchitis (croup) is a common acute respiratory infection (ARI) among children, most often caused by a virus, and should not be treated with antibiotics. Reducing the usage of unnecessary antibiotics in ARI using an antimicrobial stewardship program (ASP) is an effective measure against AMR in children. This study investigates the antibiotic prescription pattern in pediatric patients with laryngotracheobronchitis in Korea. Our results will be useful to improve the ASP.
Methods
The data were obtained from the government agency Health Insurance Review and Assessment Service. We analyzed outpatient prescriptions issued to children ≤ 5 years of age with a first-listed diagnosis code for laryngotracheobronchitis, i.e., International Classification of Disease, 10th Revision, code J050 (croup), J040 (laryngitis), or J041 (tracheitis), during 2017–2020. For each prescription, demographic information and information about medical facilities visited (type of hospital, specialty of physician, location of hospital) were extracted. The overall antibiotic prescription rate was subsequently estimated, and multivariable analysis was conducted to determine the associated factors of antibiotic prescription. Prescribed antibiotics were described and classified into extendedspectrum penicillins, cephalosporin, and macrolides.
Results
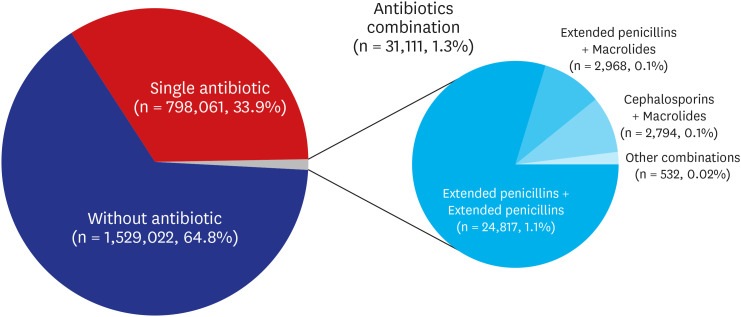
Of 2,358,194 prescriptions reviewed, 829,172 (35.2%) contained antibiotics. In the multivariable analysis, management in a hospital was the strongest factor associated with antibiotic prescription (adjusted odds ratio [aOR], 22.33; 95% confidence interval [CI], 20.87–23.89; P < 0.001), followed by management in a clinic (aOR, 12.66; 95% CI, 11.83–13.54; P < 0.001) and management in a general hospital (aOR, 8.96; 95% CI, 8.37–9.59; P < 0.001). Antibiotic prescription was also significantly associated with patients who were ≤ 2 years of age, managed by a pediatric specialist, and treated at a hospital located in a non-metropolitan region. Overall, extended-spectrum penicillins were the most frequently prescribed (18.6%) antibiotics, followed by cephalosporins (9.4%) and macrolides (8.5%).
Conclusion
The results of our study suggest that ASPs need to focus on physicians in hospitals, clinics, general hospitals, and pediatric specialties. Providing education programs to these groups to increase awareness of AMR and appropriate antibiotics use could be effective ASP policy and may help to reduce unnecessary prescriptions of antibiotics for laryngotracheobronchitis among pediatric patients and therefore potentially AMR in children in Korea.
Figure
Reference
-
1. Yoo JH. The forever war against evil germs. J Korean Med Sci. 2023; 38(10):e72. PMID: 36918026.
Article2. World Health Organization. Global Action Plan on Antimicrobial Resistance. Geneva, Switzerland: World Health Organization;2015.3. Kim K, Jung S, Kim M, Park S, Yang HJ, Lee E. Global trends in the proportion of macrolide-resistant Mycoplasma pneumonia infections: a systemic review and meta-analysis. JAMA Netw Open. 2022; 5(7):e2220949. PMID: 35816304.4. van Aerde KJ, de Haan L, van Leur M, Gerrits GP, Schers H, Moll HA, et al. Respiratory tract infection management and antibiotic prescription in children: a unique study comparing three levels of healthcare in the Netherlands. Pediatr Infect Dis J. 2021; 40(3):e100–e105. PMID: 33395212.
Article5. Mathibe LJ, Zwane NP. Unnecessary antimicrobial prescribing for upper respiratory tract infections in children in Pietermaritzburg, South Africa. Afr Health Sci. 2020; 20(3):1133–1142. PMID: 33402958.
Article6. Weragama K, Mudgil P, Whitehall J. Pediatric antimicrobial stewardship for respiratory infections in the emergency settings: a systematic review. Antibiotics (Basel). 2021; 10(11):1366. PMID: 34827304.
Article7. Romandini A, Pani A, Schenardi PA, Pattarino GA, De Giacomo C, Scaglione F. Antibiotic resistance in pediatric infections: global emerging threats, predicting the near future. Antibiotics (Basel). 2021; 10(4):393. PMID: 33917430.
Article9. Ryu S. The new Korean action plan for containment of antimicrobial resistance. J Glob Antimicrob Resist. 2017; 8:70–73. PMID: 28024981.
Article10. Cheong HS, Park KH, Kim HB, Kim SW, Kim B, Moon C, et al. Core elements for implementing antimicrobial stewardship programs in Korean general hospitals. Infect Chemother. 2022; 54(4):637–673. PMID: 36596679.
Article11. Hwang S, Kwon KT. Core elements for successful implementation of antimicrobial stewardship programs. Infect Chemother. 2021; 53(3):421–435. PMID: 34623776.
Article12. Health Insurance Review and Assessment Service. 4 out of 10 infants with colds still use antibiotics! Updated 2022. Accessed January 24, 2024. https://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA020041000100&brdScnBltNo=4&brdBltNo=10786&pageIndex=1&pageIndex2=1 .13. Ministry of Health and Welfare. 2017 Handbook of establishing and managing medical facilities. Updated 2017. Accessed April 19, 2024. https://www.mohw.go.kr/board.es?mid=a10107010000&bid=0042&act=view&list_no=357060&tag=&cg_code=&list_depth=1 .14. Perez A, Lively JY, Curns A, Weinberg GA, Halasa NB, Staat MA, et al. Respiratory virus surveillance among children with acute respiratory illnesses – new vaccine surveillance network, United States, 2016–2021. MMWR Morb Mortal Wkly Rep. 2022; 71(40):1253–1259. PMID: 36201373.
Article15. Jeon IS, Cho WJ, Lee J, Kim HM. Epidemiology and clinical severity of hospitalized children with viral croup. Pediatr Infect Vaccine. 2018; 25(1):8–16.
Article16. Song YK, Han N, Kim MG, Chang HJ, Sohn HS, Ji E, et al. A national pharmacoepidemiological study of antibiotic use in Korean paediatric outpatients. Arch Dis Child. 2017; 102(7):660–666. PMID: 28119402.
Article17. Sun G, Manzanares K, Foley KA, Zhou Y, MacGeorge EL. Antibiotic stewardship with upper respiratory tract infection patients at student health centers: Providers’ communication experiences and strategies. Am J Infect Control. 2023; 51(2):154–158. PMID: 35605753.
Article18. Korea Disease Control and Prevention Agency. Report of Infection Control and Prevention in Medical Facilities in 2021. Cheongju, Korea: Korea Disease Control and Prevention Agency;2016.19. Breuner CC, Moreno MA. Approaches to the difficult patient/parent encounter. Pediatrics. 2011; 127(1):163–169. PMID: 21173004.
Article20. Lee S. Spatial and socioeconomic inequalities in accessibility to healthcare services in South Korea. Healthcare (Basel). 2022; 10(10):2049. PMID: 36292496.
Article21. Cho BH. Regional Inequalities in Healthcare Workers and Medical Facilities.: Korean Social Trends 2018. Daejeon, Korea: Korea Statistics Research Institute;2018. p. 100–110.22. Centers for Disease Control and Prevention. Pediatric outpatient treatment recommendations. Updated 2017. Accessed January 24, 2024. https://www.cdc.gov/antibiotic-use/clinicians/pediatric-treatment-rec.html .23. Korea Disease Control and Prevention Agency. Guidelines for the Antibiotics Use in Children With Acute Upper Respiratory Tract Infection. Cheongju, Korea: Korea Disease Control and Prevention Agency;2016.24. Shin SM, Shin JY, Kim MH, Lee SH, Choi S, Park BJ. Prevalence of antibiotic use for pediatric acute upper respiratory tract infections in Korea. J Korean Med Sci. 2015; 30(5):617–624. PMID: 25931794.
Article25. Watson JR, Wang L, Klima J, Moore-Clingenpeel M, Gleeson S, Kelleher K, et al. Healthcare claims data: an underutilized tool for pediatric outpatient antimicrobial stewardship. Clin Infect Dis. 2017; 64(11):1479–1485. PMID: 28329388.
Article26. Korppi M, Heikkilä P, Palmu S, Huhtala H, Csonka P. Antibiotic prescribing for children with upper respiratory tract infection: a Finnish nationwide 7-year observational study. Eur J Pediatr. 2022; 181(8):2981–2990. PMID: 35606593.
Article27. Rybak MJ, McGrath BJ. Combination antimicrobial therapy for bacterial infections. Guidelines for the clinician. Drugs. 1996; 52(3):390–405. PMID: 8875129.
Article28. Hong KB, Choi EH, Lee HJ, Lee SY, Cho EY, Choi JH, et al. Macrolide resistance of Mycoplasma pneumoniae, South Korea, 2000–2011. Emerg Infect Dis. 2013; 19(8):1281–1284. PMID: 23876792.29. Kim JH, Kim JY, Yoo CH, Seo WH, Yoo Y, Song DJ, et al. Macrolide resistance and its impact on M. Pneumonia pneumonia in children: comparison of two recent epidemics in Korea. Allergy Asthma Immunol Res. 2017; 9(4):340–346. PMID: 28497921.
Article30. Park JY, Kang HM, Kwak EM, Rhim JW, Ahn YH, Lee H, et al. Impact of antibiotic prescribing patterns on susceptibilities of uropathogen in children below 24 months old. Antibiotics (Basel). 2020; 9(12):915. PMID: 33339282.
Article31. Korea Children’s Hospital Association. Find for specialized hospital with pediatrics. Updated 2024. Accessed April 21, 2024. https://www.kcha.kr/html/sub06/01.asp .
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Aspergillus Laryngotracheobronchitis in a Child with Primary Immunodeficiency
- Nationwide Survey on the Prevalence of Allergic Diseases according to Region and Age
- Prevalence of Inflammatory Bowel Disease Unclassified, as Estimated Using the Revised Porto Criteria, among Korean Pediatric Patients with Inflammatory Bowel Disease
- The Meaning and Impact of Appropriate Use of Antibiotics
- Methods for Estimation of Nationwide Cancer Incidence from Population-based Cancer Registries