J Korean Med Sci.
2024 Jun;39(23):e188. 10.3346/jkms.2024.39.e188.
Clinical Outcomes of Clipping and Coil Embolization for Ruptured Intracranial Aneurysms Categorized by Region and Hospital Size: A Nationwide Cohort Study in Korea
- Affiliations
-
- 1Department of Neurosurgery, Hanyang University Guri Hospital, Hanyang University College of Medicine, Guri, Korea
- 2Department of Neurosurgery, Chungnam National University Sejong Hospital, Sejong, Korea
- 3Department of Neurosurgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- KMID: 2556682
- DOI: http://doi.org/10.3346/jkms.2024.39.e188
Abstract
- Background
To analyze the outcomes of clipping and coiling for ruptured intracranial aneurysms (RIAs) based on data from the National Health Insurance Service in South Korea, with a focus on variations according to region and hospital size.
Methods
This study analyzed the one-year mortality rates for patients with RIAs who underwent clipping or coiling in 2018. Coiling was further categorized into non-stent assisted coiling (NSAC) and stent assisted coiling (SAC). Hospitals were classified as tertiary referral general hospitals (TRGHs), general hospitals (GHs), or semi-general hospitals (sGHs) based on size. South Korea’s administrative districts were divided into 15 regions for analysis.
Results
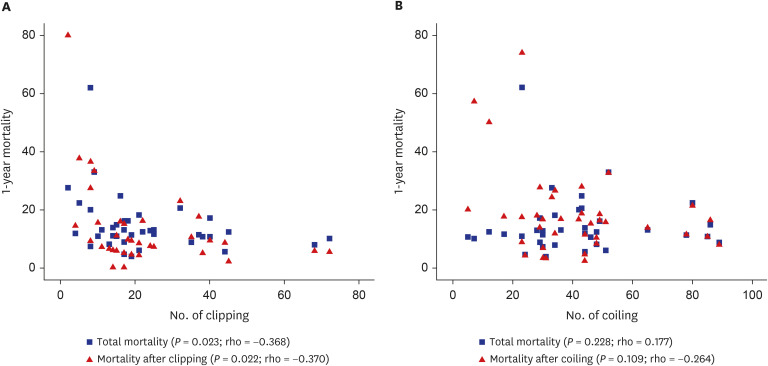
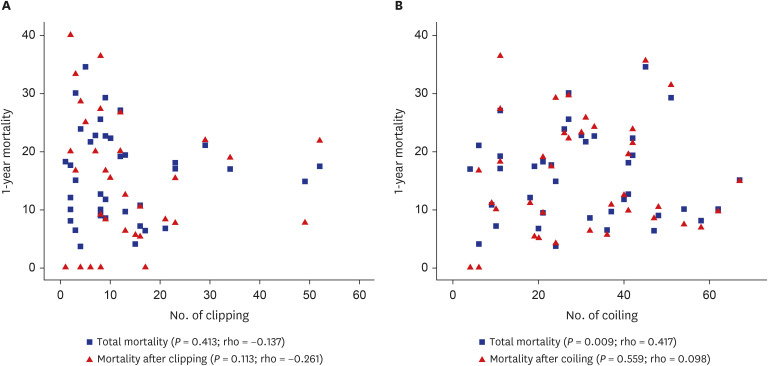
In 2018, there were 2,194 (33.1%) clipping procedures (TRGH, 985; GH, 827; sGH, 382) and 4,431 (66.9%) coiling procedures (TRGH, 1,642; GH, 2076; sGH, 713) performed for RIAs treatment. Among hospitals performing more than 20 treatments, the one-year mortality rates following clipping or coiling were 11.2% and 16.0%, respectively, with no significant difference observed. However, there was a significant difference in one-year mortality between NSAC and SAC (14.3% vs. 19.5%, P = 0.034), with clipping also showing significantly lower mortality compared to SAC (P = 0.019). No significant differences in other treatment modalities were observed according to hospital size, but clipping at TRGHs had significantly lower mortality than at GHs (P = 0.042). While no significant correlation was found between the number of treatments and outcomes at GHs, at TRGHs, a higher volume of clipping procedures was significantly associated with lower total mortality (P = 0.023) and mortality after clipping (P = 0.022).
Conclusion
Using Korea NHIS data, mortality rates for RIAs showed no significant variation by hospital size due to coiling’s prevalence. However, differences in clipping outcomes by hospital size and volume in TRGH highlight the need for national efforts to improve clipping skills and standardization. Additionally, the higher mortality rate with SAC emphasizes the importance of precise indications for its application.
Figure
Reference
-
1. Lee SU, Kim T, Kwon OK, Bang JS, Ban SP, Byoun HS, et al. Trends in the incidence and treatment of cerebrovascular diseases in Korea : Part I. Intracranial aneurysm, intracerebral hemorrhage, and arteriovenous malformation. J Korean Neurosurg Soc. 2020; 63(1):56–68. PMID: 31064041.2. Lee SH, Lee SU, Kwon OK, Bang JS, Ban SP, Kim T, et al. Clinical outcomes of clipping and coiling in elderly patients with unruptured cerebral aneurysms: a national cohort study in Korea. J Korean Med Sci. 2021; 36(26):e178. PMID: 34227262.3. Ryu BG, Lee SU, Shim HS, Park JM, Lee YJ, Kim YD, et al. Clinical outcomes of coil embolization for unruptured intracranial aneurysms categorized by region and hospital size : a nationwide cohort study in Korea. J Korean Neurosurg Soc. 2023; 66(6):690–702. PMID: 37661089.4. Lindgren A, Burt S, Bragan Turner E, Meretoja A, Lee JM, Hemmen TM, et al. Hospital case-volume is associated with case-fatality after aneurysmal subarachnoid hemorrhage. Int J Stroke. 2019; 14(3):282–289. PMID: 30019632.5. Leifer D, Fonarow GC, Hellkamp A, Baker D, Hoh BL, Prabhakaran S, et al. Association between hospital volumes and clinical outcomes for patients with nontraumatic subarachnoid hemorrhage. J Am Heart Assoc. 2021; 10(15):e018373. PMID: 34325522.6. Li H, Pan R, Wang H, Rong X, Yin Z, Milgrom DP, et al. Clipping versus coiling for ruptured intracranial aneurysms: a systematic review and meta-analysis. Stroke. 2013; 44(1):29–37. PMID: 23238862.7. Shao B, Wang J, Chen Y, He X, Chen H, Peng Y, et al. Clipping versus coiling for ruptured intracranial aneurysms: a meta-analysis of randomized controlled trials. World Neurosurg. 2019; 127:e353–e365. PMID: 30928577.8. Lanzino G, Murad MH, d’Urso PI, Rabinstein AA. Coil embolization versus clipping for ruptured intracranial aneurysms: a meta-analysis of prospective controlled published studies. AJNR Am J Neuroradiol. 2013; 34(9):1764–1768. PMID: 23578672.9. Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. 2005; 366(9488):809–817. PMID: 16139655.10. Molyneux AJ, Kerr RS, Birks J, Ramzi N, Yarnold J, Sneade M, et al. Risk of recurrent subarachnoid haemorrhage, death, or dependence and standardised mortality ratios after clipping or coiling of an intracranial aneurysm in the International Subarachnoid Aneurysm Trial (ISAT): long-term follow-up. Lancet Neurol. 2009; 8(5):427–433. PMID: 19329361.11. Kim CH, Kim YH, Sung SK, Son DW, Song GS, Lee SW. Clinical safety and effectiveness of stent-assisted coil embolization with neuroform atlas stent in intracranial aneurysm. J Korean Neurosurg Soc. 2020; 63(1):80–88. PMID: 31805757.12. Bechan RS, Sprengers ME, Majoie CB, Peluso JP, Sluzewski M, van Rooij WJ. Stent-assisted coil embolization of intracranial aneurysms: complications in acutely ruptured versus unruptured aneurysms. AJNR Am J Neuroradiol. 2016; 37(3):502–507. PMID: 26405089.13. Chalouhi N, Jabbour P, Singhal S, Drueding R, Starke RM, Dalyai RT, et al. Stent-assisted coiling of intracranial aneurysms: predictors of complications, recanalization, and outcome in 508 cases. Stroke. 2013; 44(5):1348–1353. PMID: 23512976.14. Bodily KD, Cloft HJ, Lanzino G, Fiorella DJ, White PM, Kallmes DF. Stent-assisted coiling in acutely ruptured intracranial aneurysms: a qualitative, systematic review of the literature. AJNR Am J Neuroradiol. 2011; 32(7):1232–1236. PMID: 21546464.15. Zhang G, Wu Y, Wei Y, Xue G, Chen R, Lv N, et al. Stent-assisted coiling vs. coiling alone of ruptured tiny intracranial aneurysms: a contemporary cohort study in a high-volume center. Front Neurol. 2022; 13:1076026. PMID: 36561296.16. Jiang W, Zuo Q, Xue G, Zhang X, Tang H, Duan G, et al. Low profile visualized intraluminal support stent-assisted Hydrocoil embolization for acutely ruptured wide-necked intracranial aneurysms: a propensity score-matched cohort study. Clin Neurol Neurosurg. 2022; 218:107302. PMID: 35636381.17. Russo R, Bradac GB, Castellan L, Gallesio I, Garbossa D, Iannucci G, et al. Neuroform Atlas stent-assisted coiling of ruptured intracranial aneurysms: a multicenter study. J Neuroradiol. 2021; 48(6):479–485. PMID: 32205256.18. Liu C, Guo K, Wu X, Wu L, Cai Y, Hu X, et al. Utility of low-profile visualized intraluminal support (LVIS™) stent for treatment of acutely ruptured bifurcation aneurysms: a single-center study. Front Neurol. 2023; 14:1050369. PMID: 37034062.19. Jin Y, Guo X, Quan T, Chen Z, Liu C, Guan S. Safety and efficacy of endovascular treatment for tiny ruptured intracranial aneurysms with low-profile visualized intraluminal support stents. Interv Neuroradiol. 2023; 29(2):141–147. PMID: 35147055.20. Phillips TJ, Dowling RJ, Yan B, Laidlaw JD, Mitchell PJ. Does treatment of ruptured intracranial aneurysms within 24 hours improve clinical outcome? Stroke. 2011; 42(7):1936–1945. PMID: 21680909.21. Siddiq F, Chaudhry SA, Tummala RP, Suri MF, Qureshi AI. Factors and outcomes associated with early and delayed aneurysm treatment in subarachnoid hemorrhage patients in the United States. Neurosurgery. 2012; 71(3):670–677. PMID: 22653398.22. de Gans K, Nieuwkamp DJ, Rinkel GJ, Algra A. Timing of aneurysm surgery in subarachnoid hemorrhage: a systematic review of the literature. Neurosurgery. 2002; 50(2):336–340. PMID: 11844269.23. Germans MR, Coert BA, Vandertop WP, Verbaan D. Time intervals from subarachnoid hemorrhage to rebleed. J Neurol. 2014; 261(7):1425–1431. PMID: 24807086.24. Nieuwkamp DJ, de Gans K, Algra A, Albrecht KW, Boomstra S, Brouwers PJ, et al. Timing of aneurysm surgery in subarachnoid haemorrhage--an observational study in The Netherlands. Acta Neurochir (Wien). 2005; 147(8):815–821. PMID: 15944811.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular Coil Embolization After Clipping: Endovascular Treatment of Incompletely Clipped or Recurred Cerebral Aneurysms
- Recent Trends in the Treatment of Cerebral Aneurysms: Comparison between Endovascular Coil Embolization and Surgical Clipping
- Ruptured Very Small Cerebral Aneurysms and the Usefulness of Coil Embolization
- Combined Endovascular and Microsurgical Procedures as Complementary Approaches in the Treatment of a Single Intracranial Aneurysm
- Comprehension of Two Modalities: Endovascular Coiling and Microsurgical Clipping in Treatment of Intracranial Aneurysms