Ann Pediatr Endocrinol Metab.
2024 Jun;29(3):174-181. 10.6065/apem.2346094.047.
The impacts of COVID-19 on childhood obesity: prevalence, contributing factors, and implications for management
- Affiliations
-
- 1Division of Pediatric Endocrinology, Department of Pediatrics, School of Medicine, Pusan National University, Yangsan, Korea
- 2Department of Pediatrics, Pusan National University Children’s Hospital, Yangsan, Korea
- KMID: 2556674
- DOI: http://doi.org/10.6065/apem.2346094.047
Abstract
- Purpose
This study aimed to identify changes in the prevalence of obesity and related diseases among children and adolescents during the coronavirus disease 2019 (COVID-19) pandemic.
Methods
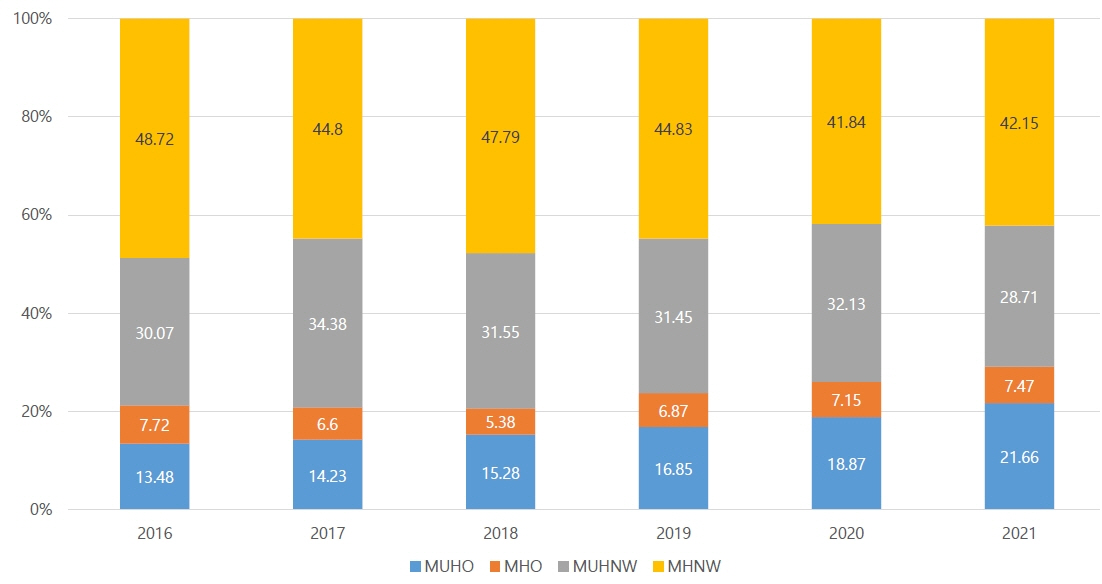
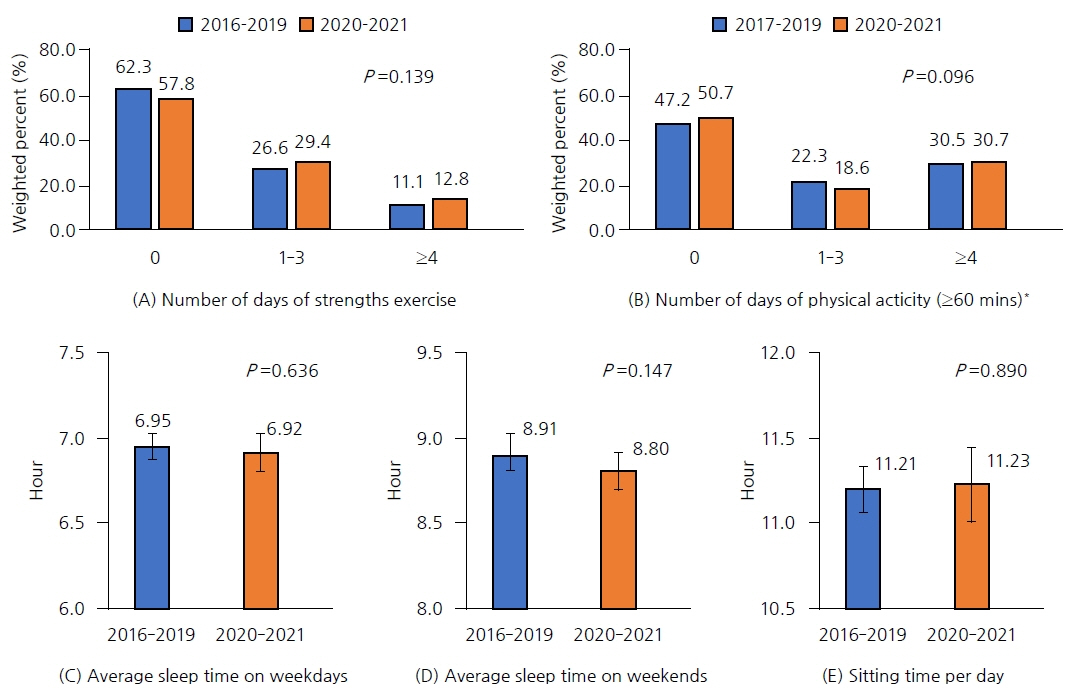
This study was conducted using data from the 2016–2021 Korean National Health and Nutrition Examination Survey and included 3,861 children and adolescents aged 10–18 years. The prevalence of obesity and related diseases was adjusted for age, sex, and income. We also analyzed the socioeconomic, nutritional, and physical activity items in the survey.
Results
During the COVID-19 pandemic, there was a significant increase in the prevalence of obesity (p=0.02), central obesity (p=0.001), mean body mass index (BMI, p=0.03), and hemoglobin A1c (p=0.005) among children and adolescents aged 10–18 years. The intake of food and calories was significantly reduced in the normal-weight group (p=0.001 and <0.001) but not in the obese group. Incidences of skipping breakfast increased and eating out decreased, regardless of obesity status. However, the changes in health behaviors were not significant. The prevalence of central obesity and increased BMI showed a significant linear association between children and their parents, especially in the 10–12-year-old age group. A clear increase in the proportion of metabolically unhealthy children and adolescents was observed in the obese group, and the frequency of central obesity in parents also increased.
Conclusion
The number of metabolically unhealthy, obese children and adolescents increased during the COVID-19 pandemic. Age-specific strategies that consider growth, development, and genetic and social factors are required. Health strategies targeting the entire family are required to develop healthier habits.
Keyword
Figure
Reference
-
References
1. Di Cesare M, Sorić M, Bovet P, Miranda JJ, Bhutta Z, Stevens GA, et al. The epidemiological burden of obesity in childhood: a worldwide epidemic requiring urgent action. BMC Med. 2019; 17:212.
Article2. World Health Organization. Fact sheet. Obesity and overweight [Internet]. Geneva (Switzerland): World Health Organization; 2024 [cited 2023 Feb 25]. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.3. Deckelbaum RJ, Williams CL. Childhood obesity: the health issue. Obes Res. 2001; 9 Suppl 4:239S–243S.
Article4. Parsons TJ, Power C, Logan S, Summerbelt C. Childhood predictors of adult obesity: a systematic review. Int J Obes Relat Metab Disord. 1999; 23 Suppl 8:S1–107.5. Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public-health crisis, common sense cure. Lancet. 2002; 360:473–82.
Article6. Lee Y, Lee KS. Relationship between unhealthy weight control behaviors and substance use patterns among Korean adolescents: results from the 2017 national youth risk behavior survey. Public Health. 2019; 174:56–64.
Article7. Zimmet P, Alberti G, Kaufman F, Tajima N, Silink M, Arslanian S, et al. The metabolic syndrome in children and adolescents. Lancet. 2007; 369:2059–61.
Article8. Ministry of Health and Welfare. Dietary reference intakes for Koreans 2020. Sejong (Korea): Ministry of Health and Welfare;2020.9. Kim HY, Kim JH. Temporal trends in the prevalence of metabolically healthy overweight and obesity in Korean youth: data from the Korea National Health and Nutrition Examination Survey 2011-2019. Ann Pediatr Endocrinol Metab. 2022; 27:134–41.
Article10. Kang S, Seo MY, Kim SH, Park MJ. Changes in lifestyle and obesity during the COVID-19 pandemic in Korean adolescents: based on the Korea Youth Risk Behavior Survey 2019 and 2020. Ann Pediatr Endocrinol Metab. 2022; 27:281–8.
Article11. Videira-Silva A, Freira S, Fonseca H. Metabolically healthy overweight adolescents: definition and components. Ann Pediatr Endocrinol Metab. 2020; 25:256–64.
Article12. Lawrence JM, Divers J, Isom S, Saydah S, Imperatore G, Pihoker C, et al. Trends in prevalence of type 1 and type 2 diabetes in children and adolescents in the US, 2001-2017. JAMA. 2021; 326:717–27.
Article13. Patarrão RS, Lautt WW, Afonso RA, Ribeiro RT, Fernandes AB, Boavida JM, et al. Postprandial but not fasting insulin resistance is an early identifier of dysmetabolism in overweight subjects. Can J Physiol Pharmacol. 2012; 90:923–31.
Article14. Espinola-Klein C, Gori T, Blankenberg S, Munzel T. Inflammatory markers and cardiovascular risk in the metabolic syndrome. Front Biosci (Landmark Ed). 2011; 16:1663–74.
Article15. Moon S, Park JS, Ahn Y. The cut-off values of triglycerides and glucose index for metabolic syndrome in American and Korean adolescents. J Korean Med Sci. 2017; 32:427–33.
Article16. Kosti RI, Panagiotakos DB, Tountas Y, Mihas CC, Alevizos A, Mariolis T, et al. Parental body mass index in association with the prevalence of overweight/obesity among adolescents in Greece; dietary and lifestyle habits in the context of the family environment: the Vyronas study. Appetite. 2008; 51:218–22.
Article17. Sijtsma A, Sauer PJ, Corpeleijn E. Parental correlations of physical activity and body mass index in young childrenthe GECKO Drenthe cohort. Int J Behav Nutr Phys Act. 2015; 12:132.18. Maffeis C, Talamini G, Tato L. Influence of diet, physical activity and parents’ obesity on children’s adiposity: a fouryear longitudinal study. Int J Obes Relat Metab Disord. 1998; 22:758–64.
Article19. Alinia S, Hels O, Tetens I. The potential association between fruit intake and body weight – a review. Obes Rev. 2009; 10:639–47.
Article20. Ventura AK, Birch LL. Does parenting affect children's eating and weight status? Int J Behav Nutr Phys Act. 2008; 5:15.
Article21. Silventoinen K, Rokholm B, Kaprio J, Sørensen TI. The genetic and environmental influences on childhood obesity: a systematic review of twin and adoption studies. Int J Obes (Lond). 2010; 34:29–40.
Article22. Fernandes MM, Sturm R. The role of school physical activity programs in child body mass trajectory. J Phys Act Health. 2011; 8:174–81.
Article23. Halliday TJ, Kwak S. Weight gain in adolescents and their peers. Econ Hum Biol. 2009; 7:181–90.
Article24. Kim SY, Yoo DM, Min C, Choi HG. Changes in dietary habits and exercise pattern of Korean adolescents from prior to during the COVID-19 pandemic. Nutrients. 2021; 13:3314.
Article25. Daviddi G, Ricci MA, De Vuono S, Gentili A, Boni M, Lupattelli G. Folate and vitamin B12 in morbid obesity: the influence of folate on anti-atherogenic lipid profile. Int J Vitam Nutr Res. 2020; 90:295–301.
Article26. Nguyen HD, Oh H, Kim MS. An increased intake of thiamine diminishes the risk of metabolic syndrome in the Korean population with various comorbidities. Diabetes Metab Syndr. 2022; 16:102443.
Article27. Dehkordi E, Sedehi M, Shahraki Z, Najafi R. Effect of folic acid on homocysteine and insulin resistance of overweight and obese children and adolescents. Adv Biomed Res. 2016; 5:88.
Article28. Engler MM, Engler MB, Malloy MJ, Chiu EY, Schloetter MC, Paul SM, et al. Antioxidant vitamins C and E improve endothelial function in children with hyperlipidemia: Endothelial Assessment of Risk from Lipids in Youth (EARLY) Trial. Circulation. 2003; 108:1059–63.
Article29. Zhou SS, Zhou Y. Excess vitamin intake: an unrecognized risk factor for obesity. World J Diabetes. 2014; 5:1–13.
Article30. Chen H, Karne RJ, Hall G, Campia U, Panza JA, Cannon RO 3rd, et al. High-dose oral vitamin C partially replenishes vitamin C levels in patients with type 2 diabetes and low vitamin C levels but does not improve endothelial dysfunction or insulin resistance. Am J Physiol Heart Circ Physiol. 2006; 290:H137–45.
Article31. Ma X, Chen Q, Pu Y, Guo M, Jiang Z, Huang W, et al. Skipping breakfast is associated with overweight and obesity: a systematic review and meta-analysis. Obes Res Clin Pract. 2020; 14:1–8.
Article32. Cayres SU, Urban JB, Fernandes RA. Physical activity and skipping breakfast have independent effects on body fatness among adolescents. J Pediatr Gastroenterol Nutr. 2018; 67:666–70.
Article33. Önnerfält J, Erlanson-Albertsson C, Montelius C, Thorngren-Jerneck K. Obese children aged 4–6 displayed decreased fasting and postprandial ghrelin levels in response to a test meal. Acta Paediatr. 2018; 107:523–8.
Article34. Betts JA, Richardson JD, Chowdhury EA, Holman GD, Tsintzas K, Thompson D. The causal role of breakfast in energy balance and health: a randomized controlled trial in lean adults. Am J Clin Nutr. 2014; 100:539–47.
Article35. Sears B, Perry M. The role of fatty acids in insulin resistance. Lipids Health Dis. 2015; 14:121.
Article36. Lee JS, Mishra G, Hayashi K, Watanabe E, Mori K, Kawakubo K. Combined eating behaviors and overweight: Eating quickly, late evening meals, and skipping breakfast. Eat Behav. 2016; 21:84–8.
Article37. Yamamoto R, Tomi R, Shinzawa M, Yoshimura R, Ozaki S, Nakanishi K, et al. Associations of skipping breakfast, lunch, and dinner with weight gain and overweight/obesity in university students: a retrospective cohort study. Nutrients. 2021; 13:271.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The COVID-19 pandemic: an unprecedented tragedy in the battle against childhood obesity
- Diabetes, Obesity, and COVID-19
- Changes in Expenditures of the National Health Insurance of Korea during the COVID-19 Pandemic and the Financial Implications Thereof
- The prevalence of childhood obesity and risk factors associated with obesity in Asan city
- Changes in lifestyle and obesity during the COVID-19 pandemic in Korean adolescents: based on the Korea Youth Risk Behavior Survey 2019 and 2020