Ann Pediatr Endocrinol Metab.
2024 Jun;29(3):142-151. 10.6065/apem.2346184.092.
Gamma-aminobutyric acid for delaying type 1 diabetes mellitus: an update
- Affiliations
-
- 1Faculty of Medicine, Udayana University, Denpasar, Bali, Indonesia
- 2Faculty of Medicine, Udayana University, Denpasar, Bali, Indonesia
- 3Division of Endocrinology and Metabolism, Department of Internal Medicine, Faculty of Medicine, Udayana University/Prof. IGNG Ngoerah General Hospital, Bali, Indonesia
- KMID: 2556669
- DOI: http://doi.org/10.6065/apem.2346184.092
Abstract
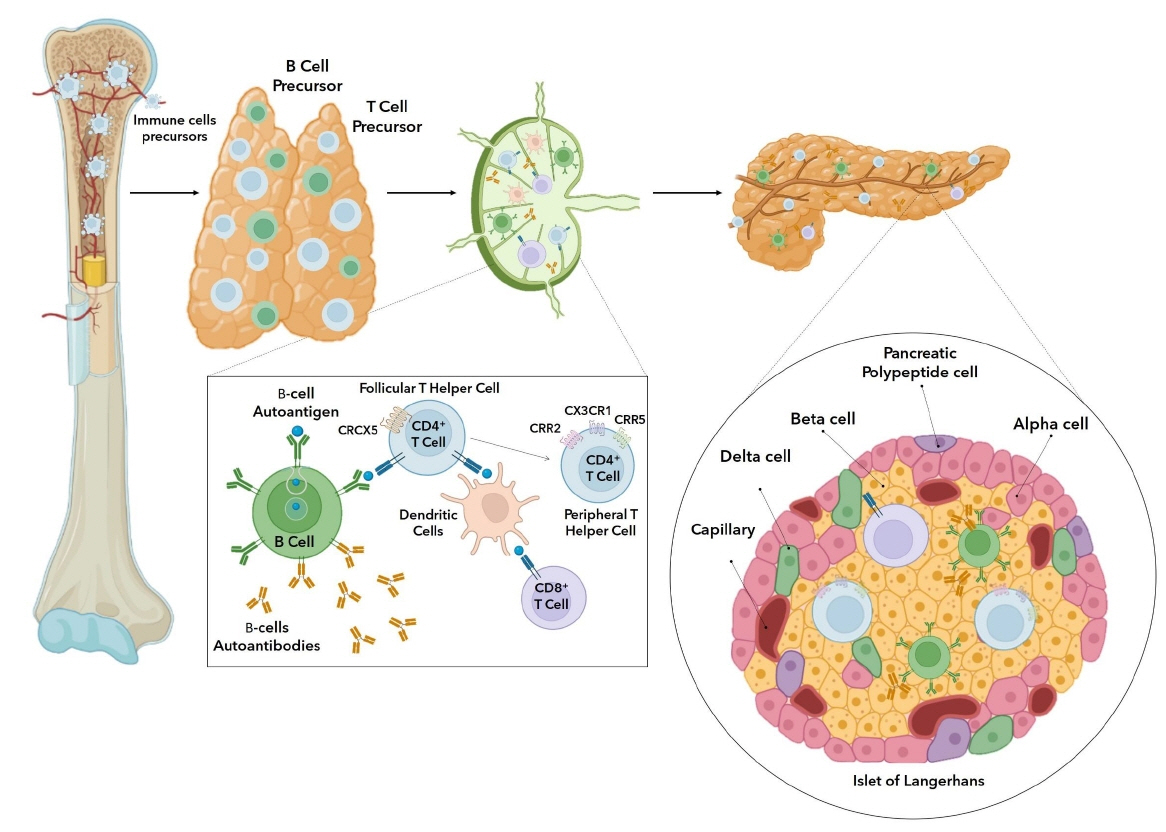
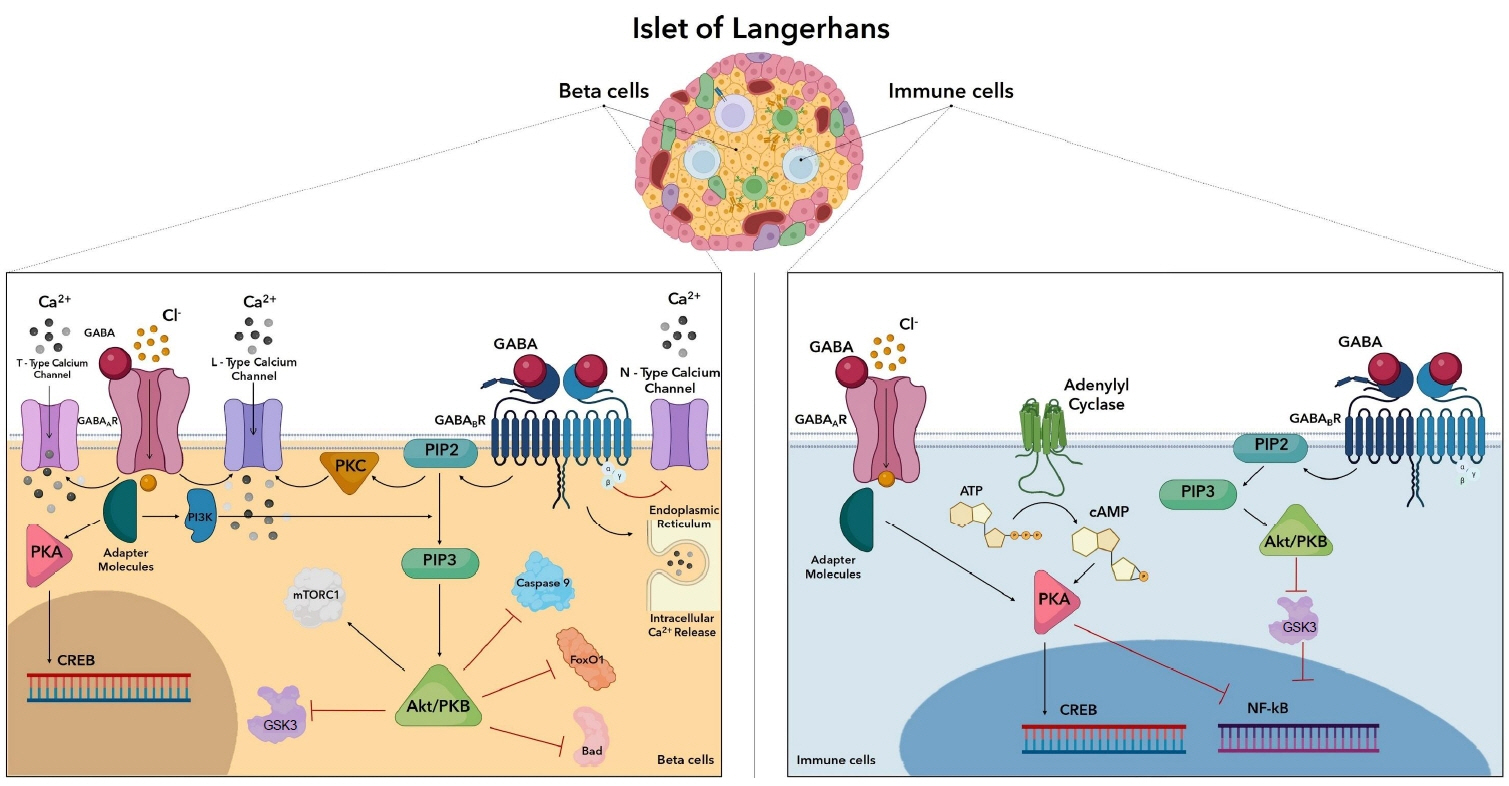
- The current gold-standard management of hyperglycemia in individuals with type 1 diabetes mellitus (T1DM) is insulin therapy. However, this therapy is associated with a high incidence of complications, and delaying the onset of this disease produces a substantially positive impact on quality of life for individuals with a predisposition to T1DM, especially children. This review aimed to assess the use of gamma-aminobutyric acid (GABA) to delay the onset of T1DM in children. GABA produces protective and proliferative effects in 2 ways, β cell and immune cell modulation. Various in vitro and in vivo studies have shown that GABA induces proliferation of β cells, increases insulin levels, inhibits β-cell apoptosis, and suppresses T helper 1 cell activity against islet antigens. Oral GABA is safe as no serious adverse effects were reported in any of the studies included in this review. These findings demonstrate promising results for the use of GABA treatment to delay T1DM, specifically in genetically predisposed children, through immunoregulatory effects and the ability to induce β-cell proliferation.
Figure
Reference
-
References
1. Kahanovitz L, Sluss PM, Russell SJ. Type 1 diabetes - a clinical perspective. Point Care. 2017; 16:37–40.2. Gregory GA, Robinson TIG, Linklater SE, Wang F, Colagiuri S, de Beaufort C, et al. Global incidence, prevalence, and mortality of type 1 diabetes in 2021 with projection to 2040: a modelling study. Lancet Diabetes Endocrinol. 2022; 10:741–60.
Article3. Rafferty J, Stephens JW, Atkinson MD, Luzio SD, Akbari A, Gregory JW, et al. A retrospective epidemiological study of type 1 diabetes mellitus in Wales, UK between 2008 and 2018. Int J Popul Data Sci. 2021; 6:1387.
Article4. Karras SN, Koufakis T, Zebekakis P, Kotsa K. Pharmacologic adjunctive to insulin therapies in type 1 diabetes: the journey has just begun. World J Diabetes. 2019; 10:234–40.
Article5. Espes D, Liljebäck H, Hill H, Elksnis A, Caballero-Corbalan J, Birnir B, et al. GABA induces a hormonal counterregulatory response in subjects with long-standing type 1 diabetes. BMJ Open Diabetes Res Care. 2021; 9:e002442.
Article6. Rachdi L, Maugein A, Pechberty S, Armanet M, Hamroune J, Ravassard P, et al. Regulated expression and function of the GABAB receptor in human pancreatic beta cell line and islets. Sci Rep. 2020; 10:13469.7. Badri H, Gibbard C, Denton D, Satia I, Al-Sheklly B, Dockry RJ, et al. A double-blind randomised placebocontrolled trial investigating the effects of lesogaberan on the objective cough frequency and capsaicin-evoked coughs in patients with refractory chronic cough. ERJ Open Res. 2022; 8:00546–2021.
Article8. Tian J, Dang H, Hu A, Xu W, Kaufman DL. Repurposing Lesogaberan to promote human islet cell survival and β-cell replication. J Diabetes Res. 2017; 2017:6403539.9. Insel RA, Dunne JL, Atkinson MA, Chiang JL, Dabelea D, Gottlieb PA, et al. Staging presymptomatic type 1 diabetes: a scientific statement of JDRF, the Endocrine Society, and the American Diabetes Association. Diabetes Care. 2015; 38:1964–74.
Article10. Katsarou A, Gudbjörnsdottir S, Rawshani A, Dabelea D, Bonifacio E, Anderson BJ, et al. Type 1 diabetes mellitus. Nat Rev Dis Prim. 2017; 3:17016.
Article11. Yahaya T, Adedayo T. Genes predisposing to type 1 diabetes mellitus and pathophysiology: a narrative review. Med J Indones. 2020; 29:100–9.
Article12. Krischer JP, Lynch KF, Lernmark Å, Hagopian WA, Rewers MJ, She JX, et al. Genetic and environmental interactions modify the risk of diabetes-related autoimmunity by 6 years of age: the TEDDY study. Diabetes Care. 2017; 40:1194–202.
Article13. Zaccardi F, Webb DR, Yates T, Davies MJ. Pathophysiology of type 1 and type 2 diabetes mellitus: a 90-year perspective. Postgrad Med J. 2016; 92:63–9.
Article14. Steck AK, Johnson K, Barriga KJ, Miao D, Yu L, Hutton JC, et al. Age of islet autoantibody appearance and mean levels of insulin, but not GAD or IA-2 autoantibodies, predict age of diagnosis of type 1 diabetes: diabetes autoimmunity study in the young. Diabetes Care. 2011; 34:1397–9.15. Fousteri G, Ippolito E, Ahmed R, Hamad ARA. Beta-cell specific autoantibodies: are they just an indicator of type 1 diabetes? Curr Diabetes Rev. 2017; 13:322–9.
Article16. Bluestone JA, Herold K, Eisenbarth G. Genetics, pathogenesis and clinical interventions in type 1 diabetes. Nature. 2010; 464:1293–300.
Article17. Vandamme C, Kinnunen T. B cell helper T cells and type 1 diabetes. Scand J Immunol. 2020; 92:e12943.
Article18. Greaves RB, Chen D, Green EA. Thymic B cells as a new player in the type 1 diabetes response. Front Immunol. 2021; 12:772017.
Article19. Perera J, Huang H. The development and function of thymic B cells. Cell Mol Life Sci. 2015; 72:2657–63.
Article20. Colli ML, Szymczak F, Eizirik DL. Molecular footprints of the immune assault on pancreatic beta cells in type 1 diabetes. Front Endocrinol (Lausanne) 2020:11:568446.21. Zajec A, Trebušak Podkrajšek K, Tesovnik T, Šket R, Čugalj Kern B, Jenko Bizjan B, et al. Pathogenesis of type 1 diabetes: established facts and new insights. Genes (Basel). 2022; 13:706.
Article22. Ilonen J, Lempainen J, Veijola R. The heterogeneous pathogenesis of type 1 diabetes mellitus. Nat Rev Endocrinol. 2019; 15:635–50.
Article23. Culina S, Lalanne AI, Afonso G, Cerosaletti K, Pinto S, Sebastiani G, et al. Islet-reactive CD8+ T cell frequencies in the pancreas, but not in blood, distinguish type 1 diabetic patients from healthy donors. Sci Immunol. 2018; 3:eaao4013.24. Yu W, Jiang N, Ebert PJ, Kidd BA, Müller S, Lund PJ, et al. Clonal deletion prunes but does not eliminate self-specific αβ CD8(+) T lymphocytes. Immunity. 2015; 42:929–41.
Article25. Gonzalez-Duque S, Azoury ME, Colli ML, Afonso G, Turatsinze JV, Nigi L, et al. Conventional and neo-antigenic peptides presented by β cells are targeted by circulating naïve CD8+ T cells in type 1 diabetic and healthy donors. Cell Metab. 2018; 28:946–60.e6.
Article26. Roep BO, Thomaidou S, van Tienhoven R, Zaldumbide A. Type 1 diabetes mellitus as a disease of the β-cell (do not blame the immune system?). Nat Rev Endocrinol. 2021; 17:150–61.
Article27. Coppieters KT, Dotta F, Amirian N, Campbell PD, Kay TW, Atkinson MA, et al. Demonstration of islet-autoreactive CD8 T cells in insulitic lesions from recent onset and longterm type 1 diabetes patients. J Exp Med. 2012; 209:51–60.
Article28. Willcox A, Gillespie KM. Histology of type 1 diabetes pancreas. Methods Mol Biol. 2016; 1433:105–17.
Article29. Writing Group for the TRIGR Study Group. Effect of hydrolyzed infant formula vs conventional formula on risk of type 1 diabetes: the TRIGR randomized clinical trial. JAMA. 2018; 319:38–48.30. Hummel S, Pflüger M, Hummel M, Bonifacio E, Ziegler AG. Primary dietary intervention study to reduce the risk of islet autoimmunity in children at increased risk for type 1 diabetes: the BABYDIET study. Diabetes Care. 2011; 34:1301–5.31. Lampeter EF, Klinghammer A, Scherbaum WA, Heinze E, Haastert B, Giani G, et al. The Deutsche Nicotinamide Intervention Study: an attempt to prevent type 1 diabetes. DENIS Group. Diabetes. 1998; 47:980–4.
Article32. Simpson M, Brady H, Yin X, Seifert J, Barriga K, Hoffman M, et al. No association of vitamin D intake or 25-hydroxyvitamin D levels in childhood with risk of islet autoimmunity and type 1 diabetes: the Diabetes Autoimmunity Study in the Young (DAISY). Diabetologia. 2011; 54:2779–88.
Article33. Cazeau RM, Huang H, Bauer JA, Hoffman RP. Effect of vitamins C and E on endothelial function in type 1 diabetes mellitus. J Diabetes Res. 2016; 2016:3271293.
Article34. Skyler JS, Krischer JP, Wolfsdorf J, Cowie C, Palmer JP, Greenbaum C, et al. Effects of oral insulin in relatives of patients with type 1 diabetes: the diabetes prevention trial--type 1. Diabetes Care. 2005; 28:1068–76.35. Krischer JP, Schatz DA, Bundy B, Skyler JS, Greenbaum CJ. Effect of oral insulin on prevention of diabetes in relatives of patients with type 1 diabetes: a randomized clinical trial. JAMA. 2017; 318:1891–902.
Article36. Elding Larsson H, Lundgren M, Jonsdottir B, Cuthbertson D, Krischer J. Safety and efficacy of autoantigen-specific therapy with 2 doses of alum-formulated glutamate decarboxylase in children with multiple islet autoantibodies and risk for type 1 diabetes: a randomized clinical trial. Pediatr Diabetes. 2018; 19:410–9.
Article37. Quattrin T, Haller MJ, Steck AK, Felner EI, Li Y, Xia Y, et al. Golimumab and beta-cell function in youth with newonset type 1 diabetes. N Engl J Med. 2020; 383:2007–17.
Article38. Gitelman SE, Bundy BN, Ferrannini E, Lim N, Blanchfield JL, DiMeglio LA, et al. Imatinib therapy for patients with recent-onset type 1 diabetes: a multicentre, randomised, double-blind, placebo-controlled, phase 2 trial. lancet Diabetes Endocrinol. 2021; 9:502–14.39. Cook JJ, Hudson I, Harrison LC, Dean B, Colman PG, Werther G, et al. Double-blind controlled trial of azathioprine in children with newly diagnosed type i diabetes. Diabetes. 1989; 38:779–83.
Article40. de Groot P, Nikolic T, Pellegrini S, Sordi V, Imangaliyev S, Rampanelli E, et al. Faecal microbiota transplantation halts progression of human new-onset type 1 diabetes in a randomised controlled trial. Gut. 2021; 70:92–105.
Article41. Boggi U, Baronti W, Amorese G, Pilotti S, Occhipinti M, Perrone V, et al. Treating type 1 diabetes by pancreas transplant alone: a cohort study on actual long-term (10 years) efficacy and safety. Transplantation. 2022; 106:147–57.
Article42. Wang X, Kang J, Liu Q, Tong T, Quan H. Fighting diabetes mellitus: pharmacological and non-pharmacological approaches. Curr Pharm Des. 2020; 26:4992–5001.
Article43. Ziegler AG, Schmid S, Huber D, Hummel M, Bonifacio E. Early infant feeding and risk of developing type 1 diabetesassociated autoantibodies. JAMA. 2003; 290:1721–8.
Article44. Knip M, Virtanen SM, Seppä K, Ilonen J, Savilahti E, Vaarala O, et al. Dietary intervention in infancy and later signs of beta-cell autoimmunity. N Engl J Med. 2010; 363:1900–8.
Article45. Orban T, Bundy B, Becker DJ, Dimeglio LA, Gitelman SE, Goland R, et al. Costimulation modulation with abatacept in patients with recent-onset type 1 diabetes: followup 1 year after cessation of treatment. Diabetes Care. 2014; 37:1069–75.
Article46. Rigby MR, Harris KM, Pinckney A, DiMeglio LA, Rendell MS, Felner EI, et al. Alefacept provides sustained clinical and immunological effects in new-onset type 1 diabetes patients. J Clin Invest. 2015; 125:3285–96.
Article47. Pescovitz MD, Greenbaum CJ, Bundy B, Becker DJ, Gitelman SE, Goland R, et al. B-lymphocyte depletion with rituximab and β-cell function: two-year results. Diabetes Care. 2014; 37:453–9.
Article48. Janež A, Guja C, Mitrakou A, Lalic N, Tankova T, Czupryniak L, et al. Insulin therapy in adults with type 1 diabetes mellitus: a narrative review. Diabetes Ther Res Treat Educ diabetes Relat Disord. 2020; 11:387–409.
Article49. Qiao YC, Chen YL, Pan YH, Tian F, Xu Y, Zhang XX, et al. The change of serum tumor necrosis factor alpha in patients with type 1 diabetes mellitus: a systematic review and meta-analysis. PLoS One. 2017; 12:e0176157.
Article50. Fountas A, Diamantopoulos LN, Tsatsoulis A. Tyrosine kinase inhibitors and diabetes: a novel treatment paradigm? Trends Endocrinol Metab. 2015; 26:643–56.
Article51. Zeng Q, Song J, Wang D, Sun X, Xiao Y, Zhang H, et al. Identification of sorafenib as a treatment for type 1 diabetes. Front Immunol. 2022; 13:740805.
Article52. Kolb H, von Herrath M. Immunotherapy for type 1 diabetes: why do current protocols not halt the underlying disease process? Cell Metab. 2017; 25:233–41.
Article53. Bottino R, Knoll MF, Knoll CA, Bertera S, Trucco MM. The future of islet transplantation is now. Front Med. 2018; 5:202.
Article54. Uusi-Oukari M, Korpi ER. Regulation of GABA(A) receptor subunit expression by pharmacological agents. Pharmacol Rev. 2010; 62:97–135.
Article55. Dwyer TM. Chapter 4 - Chemical signaling in the nervous system. In : Haines DE, Mihailoff GA, editors. Fundamental neuroscience for basic and clinical applications (fifth edition). Amsterdam (Netherlands): Elsevier;2018. p. 54–71.e1.56. Purwana I, Zheng J, Li X, Deurloo M, Son DO, Zhang Z, et al. GABA promotes human β-cell proliferation and modulates glucose homeostasis. Diabetes. 2014; 63:4197–205.
Article57. Karls A, Mynlieff M. GABAB receptors couple to Gαq to mediate increases in voltage-dependent calcium current during development. J Neurochem. 2015; 135:88–100.
Article58. Leng S, Xie F, Liu J, Shen J, Quan G, Wen T. LLGL2 increases Ca(2+) influx and exerts oncogenic activities via PI3K/AKT signaling pathway in hepatocellular carcinoma. Front Oncol. 2021; 11:683629.
Article59. Marat AL, Haucke V. Phosphatidylinositol 3-phosphates-at the interface between cell signalling and membrane traffic. EMBO J. 2016; 35:561–79.
Article60. Camaya I, Donnelly S, O'Brien B. Targeting the PI3K/Akt signaling pathway in pancreatic β-cells to enhance their survival and function: an emerging therapeutic strategy for type 1 diabetes. J Diabetes. 2022; 14:247–60.61. Zhang B, Sun P, Shen C, Liu X, Sun J, Li D, et al. Role and mechanism of PI3K/AKT/FoxO1/PDX-1 signaling pathway in functional changes of pancreatic islets in rats after severe burns. Life Sci. 2020; 258:118145.
Article62. Dasari S, Tchounwou PB. Cisplatin in cancer therapy: molecular mechanisms of action. Eur J Pharmacol. 2014; 740:364–78.
Article63. Wang J, Liu H, Zhang X, Li X, Geng L, Zhang H, et al. Sulfated hetero-polysaccharides protect SH-SY5Y cells from H2O2-induced apoptosis by affecting the PI3K/Akt signaling pathway. Mar Drugs. 2017; 15:110.
Article64. Ardestani A, Lupse B, Kido Y, Leibowitz G, Maedler K. mTORC1 signaling: a double-edged sword in diabetic β cells. Cell Metab. 2018; 27:314–31.
Article65. Bhat R, Axtell R, Mitra A, Miranda M, Lock C, Tsien RW, et al. Inhibitory role for GABA in autoimmune inflammation. Proc Natl Acad Sci. 2010; 107:2580–5.
Article66. Bhandage AK, Jin Z, Korol SV, Shen Q, Pei Y, Deng Q, et al. GABA regulates release of inflammatory cytokines from peripheral blood mononuclear cells and CD4+ T cells and is immunosuppressive in type 1 diabetes. EBioMedicine. 2018; 30:283–94.
Article67. Dionisio L, José De Rosa M, Bouzat C, Esandi Mdel C. An intrinsic GABAergic system in human lymphocytes. Neuropharmacology. 2011; 60:513–9.
Article68. Bhandage AK, Jin Z, Hellgren C, Korol SV, Nowak K, Williamsson L, et al. AMPA, NMDA and kainate glutamate receptor subunits are expressed in human peripheral blood mononuclear cells (PBMCs) where the expression of GluK4 is altered by pregnancy and GluN2D by depression in pregnant women. J Neuroimmunol. 2017; 305:51–8.
Article69. Halls ML, Cooper DM. Regulation by Ca2+-signaling pathways of adenylyl cyclases. Cold Spring Harb Perspect Biol. 2011; 3:a004143.
Article70. Wehbi VL, Taskén K. Molecular mechanisms for cAMPmediated immunoregulation in T cells - role of anchored protein kinase A signaling units. Front Immunol. 2016; 7:222.
Article71. Barnabei L, Laplantine E, Mbongo W, Rieux-Laucat F, Weil R. NF-κB: at the borders of autoimmunity and inflammation. Front Immunol. 2021; 12:716469.
Article72. Shu Q, Liu J, Liu X, Zhao S, Li H, Tan Y, et al. GABAB R/GSK-3β/NF-κB signaling pathway regulates the proliferation of colorectal cancer cells. Cancer Med. 2016; 5:1259–67.73. Reyes-García MG, Hernández-Hernández F, Hernández-Téllez B, García-Tamayo F. GABA (A) receptor subunits RNA expression in mice peritoneal macrophages modulate their IL-6/IL-12 production. J Neuroimmunol. 2007; 188:64–8.
Article74. Wei M, Li L, Meng R, Fan Y, Liu Y, Tao L, et al. Suppressive effect of diazepam on IFN-gamma production by human T cells. Int Immunopharmacol. 2010; 10:267–71.75. Bhandage AK, Barragan A. GABAergic signaling by cells of the immune system: more the rule than the exception. Cell Mol Life Sci. 2021; 78:5667–79.
Article76. Goto M, Murakawa M, Kadoshima-Yamaoka K, Tanaka Y, Inoue H, Murafuji H, et al. Phosphodiesterase 7A inhibitor ASB16165 suppresses proliferation and cytokine production of NKT cells. Cell Immunol. 2009; 258:147–51.
Article77. Zhao W, Huang Y, Liu Z, Cao BB, Peng YP, Qiu YH. Dopamine Receptors modulate cytotoxicity of natural killer cells via cAMP-PKA-CREB signaling pathway. PLoS One. 2013; 8:e65860.
Article78. I Ciftci H, G Sierra R, Yoon CH, Su Z, Tateishi H, Koga R, et al. Serial femtosecond x-ray diffraction of HIV-1 gag MAIP6 microcrystals at ambient temperature. Int J Mol Sci. 2019; 20:1675.
Article79. Oger S, Méhats C, Dallot E, Cabrol D, Leroy MJ. Evidence for a role of phosphodiesterase 4 in lipopolysaccharidestimulated prostaglandin E2 production and matrix metalloproteinase-9 activity in human amniochorionic membranes. J Immunol. 2005; 174:8082–9.
Article80. Lamichhane S, Sen P, Dickens AM, Alves MA, Härkönen T, Honkanen J, et al. Dysregulation of secondary bile acid metabolism precedes islet autoimmunity and type 1 diabetes. Cell Reports Med. 2022; 3:100762.
Article81. Yi Z, Waseem Ghani M, Ghani H, Jiang W, Waseem Birmani M, Ye L, et al. Gimmicks of gamma-aminobutyric acid (GABA) in pancreatic β-cell regeneration through transdifferentiation of pancreatic α- to β-cells. Cell Biol Int. 2020; 44:926–36.
Article82. Soltani N, Qiu H, Aleksic M, Glinka Y, Zhao F, Liu R, et al. GABA exerts protective and regenerative effects on islet beta cells and reverses diabetes. Proc Natl Acad Sci. 2011; 108:11692–7.
Article83. Wang Q, Prud'homme G, Wan Y. GABAergic system in the endocrine pancreas: a new target for diabetes treatment. Diabetes Metab Syndr Obes Targets Ther. 2015; 8:79–87.
Article84. Weir GC, Bonner-Weir S. GABA signaling stimulates β cell regeneration in diabetic mice. Cell. 2017; 168:7–9.
Article85. Ghani MW, Yi Z, Jiang W, Bin L, Cun LG, Birmany MW, et al. Gamma-aminobutyric acid (GABA) induced in vitro differentiation of rat pancreatic ductal stem cells into insulin-secreting islet-like cell clusters. Folia Biol (Praha). 2019; 65:246–55.86. Liu W, Lau HK, Son DO, Jin T, Yang Y, Zhang Z, et al. Combined use of GABA and sitagliptin promotes human β-cell proliferation and reduces apoptosis. J Endocrinol. 2021; 248:133–43.
Article87. Tian J, Middleton B, Lee VS, Park HW, Zhang Z, Kim B, et al. GABA(B)-receptor agonist-based immunotherapy for type 1 diabetes in NOD mice. Biomedicines. 2021; 9:43.
Article88. Tian J, Lu Y, Zhang H, Chau CH, Dang HN, Kaufman DL. Gamma-aminobutyric acid inhibits T cell autoimmunity and the development of inflammatory responses in a mouse type 1 diabetes model. J Immunol. 2004; 173:5298–304.89. Ben-Othman N, Vieira A, Courtney M, Record F, Gjernes E, Avolio F, et al. Long-term GABA administration induces alpha cell-mediated beta-like cell neogenesis. Cell. 2017; 168:73–85.e11.
Article90. Untereiner A, Xu J, Bhattacharjee A, Cabrera O, Hu C, Dai FF, et al. Gamma-aminobutyric acid stimulates β-cell proliferation through the mTORC1/p70S6K pathway, an effect amplified by Ly49, a novel γ-aminobutyric acid type A receptor positive allosteric modulator. Diabetes Obes Metab. 2020; 22:2021–31.91. Choat HM, Martin A, Mick GJ, Heath KE, Tse HM, McGwin GJ, et al. Effect of gamma aminobutyric acid (GABA) or GABA with glutamic acid decarboxylase (GAD) on the progression of type 1 diabetes mellitus in children: Trial design and methodology. Contemp Clin Trials. 2019; 82:93–100.
Article92. Hagan DW, Ferreira SM, Santos GJ, Phelps EA. The role of GABA in islet function. Front Endocrinol (Lausanne). 2022; 13:972115.
Article93. Allen MJ, Sabir S, Sharma S. GABA receptor. 2023 Feb 13. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; Jan–.94. Oketch-Rabah HA, Madden EF, Roe AL, Betz JM. United States Pharmacopeia (USP) safety review of gammaaminobutyric acid (GABA). Nutrients. 2021; 13:2742.
Article95. Janković SM, Dješević M, Janković SV. Experimental GABA A receptor agonists and allosteric modulators for the treatment of focal epilepsy. J Exp Pharmacol. 2021; 13:235–44.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effects of Zolpidem on Akinesia in a Parkinson Disease Patient: A Case Report
- GABA, benzodiazepine receptors and their functions
- GABA Receptor Functions IN the Cectral Nervous System
- The Gut-Brain Axis: The Missing Link in Depression
- PPARgamma2 gene polymorphism in type 2 diabetes mellitus and obesity