Neurointervention.
2024 Jul;19(2):92-101. 10.5469/neuroint.2024.00108.
Feasibility, Safety, and Efficacy of Endovascular vs. Surgical Treatment of Unruptured Multi-Sac Intracranial Aneurysms in a Single-Center Retrospective Series
- Affiliations
-
- 1Department of Diagnostic and Interventional Radiology, Faculty of Medicine and University Hospital Cologne, University of Cologne, Köln, Germany
- 2Department of General Neurosurgery, Center of Neurosurgery, Faculty of Medicine and University Hospital Cologne, University of Cologne, Köln, Germany
- KMID: 2556660
- DOI: http://doi.org/10.5469/neuroint.2024.00108
Abstract
- Purpose
Multi-sac aneurysms (MSAs) are not uncommon, but studies on their management are scarce. This study aims to evaluate and compare the feasibility, safety, and efficacy of MSAs treated with either clipping or coiling after interdisciplinary case discussion at our center.
Materials and Methods
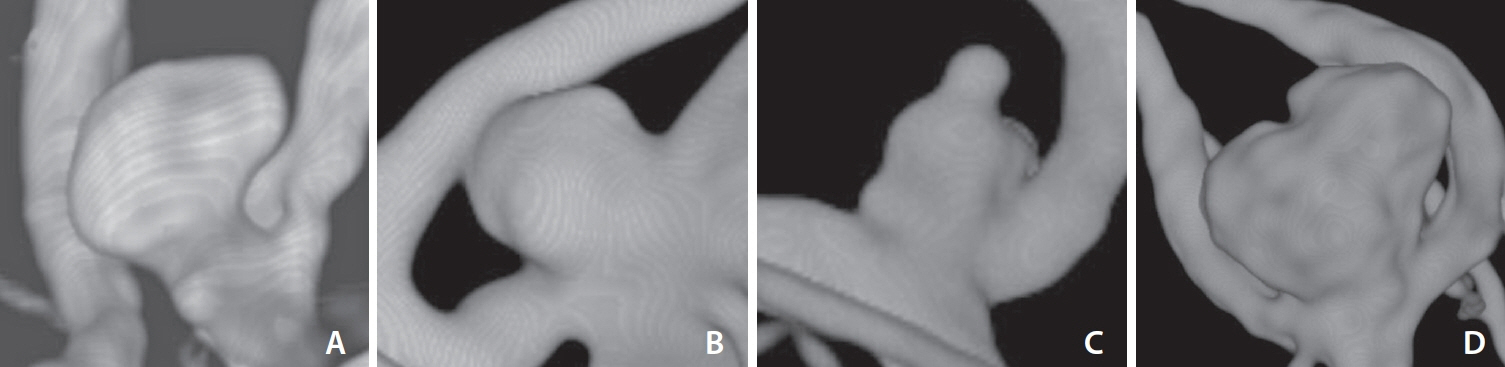
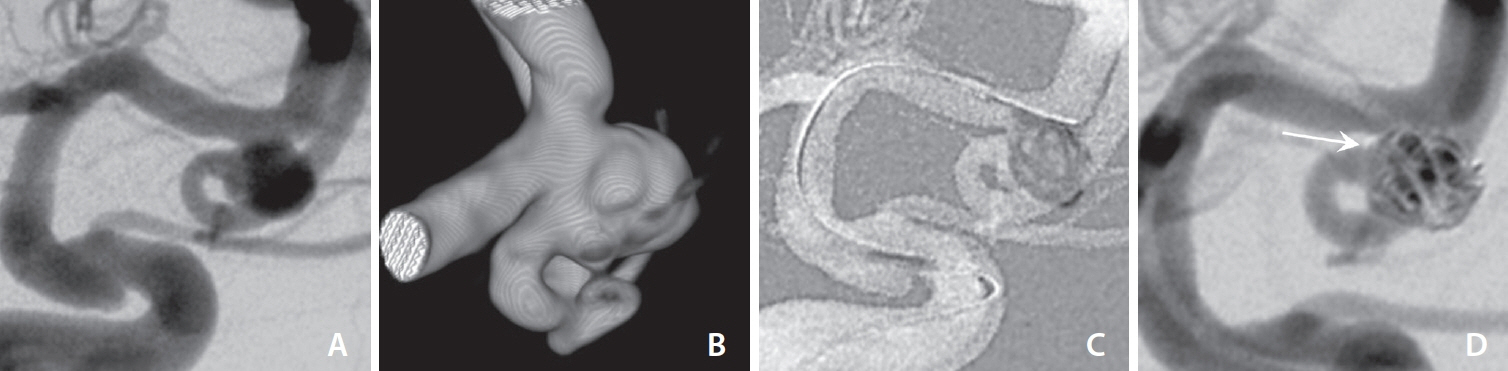
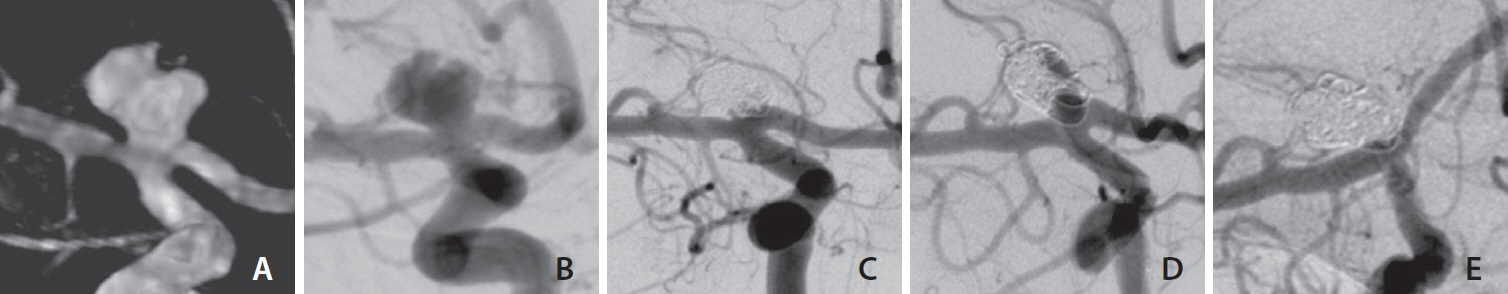
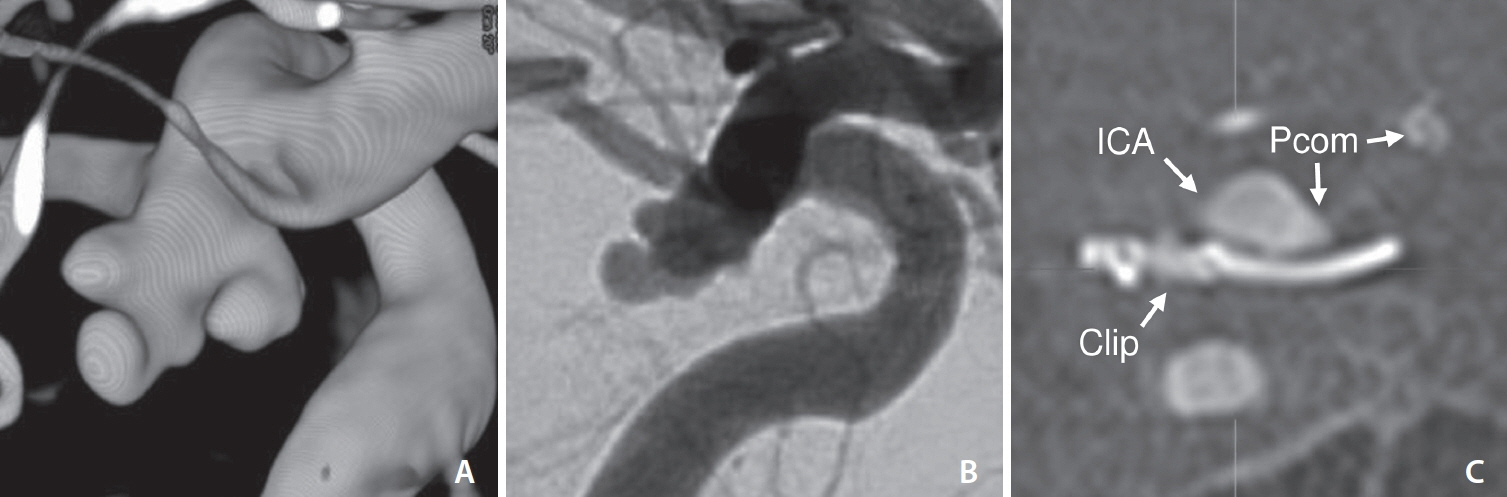
We retrospectively analyzed MSAs treated by microsurgical clipping, coiling, or stent-assisted coiling (SAC). Treatment modalities, complications, angiographic results, and clinical outcomes were evaluated. Major neurological events were defined as a safety endpoint and complete occlusion as an efficacy endpoint.
Results
Ninety patients (mean age, 53.2±11.0 years; 73 [81.1%] females) with MSAs met our inclusion criteria (clipping, 50; coiling, 19; SAC, 21). Most aneurysms were located in the middle cerebral artery (48.9%). All clipping procedures were technically successful, but endovascular treatment failed in 1 coiling case, and a switch from coiling to SAC was required in 2 cases. The major event rates were 4.0% after clipping (1 major stroke and 1 intracranial hemorrhage) and 0% after endovascular therapy (P=0.667). At mid-term angiographic follow-up (mean 12.0±8.9 months), all 37 followed clipped aneurysms were completely occluded, compared to 8/17 (41.7%) after coiling and 11/15 (73.3%) after SAC (P<0.001). Coiling was significantly associated with incomplete occlusion in the adjusted analysis (odds ratio, 11.7; 95% confidence interval, 2.7–52.6; P=0.001).
Conclusion
Both endovascular and surgical treatment were feasible and safe for MSAs. As coiling was associated with comparatively high recanalization rates, endovascular treatment may be preferred with stent support.
Figure
Reference
-
1. Abboud T, Rustom J, Bester M, Czorlich P, Vittorazzi E, Pinnschmidt HO, et al. Morphology of ruptured and unruptured intracranial aneurysms. World Neurosurg. 2017; 99:610–617.2. Forbes G, Fox AJ, Huston J 3rd, Wiebers DO, Torner J. Interobserver variability in angiographic measurement and morphologic characterization of intracranial aneurysms: a report from the International Study of Unruptured Intracranial Aneurysms. AJNR Am J Neuroradiol. 1996; 17:1407–1415.3. Dhar S, Tremmel M, Mocco J, Kim M, Yamamoto J, Siddiqui AH, et al. Morphology parameters for intracranial aneurysm rupture risk assessment. Neurosurgery. 2008; 63:185–196. discussion 196-197.4. Etminan N, Beseoglu K, Barrow DL, Bederson J, Brown RD Jr, Connolly ES Jr, et al. Multidisciplinary consensus on assessment of unruptured intracranial aneurysms: proposal of an international research group. Stroke. 2014; 45:1523–1530.5. Sorenson T, Brinjikji W, Lanzino G. Newer endovascular tools: a review of experimental and clinical aspects. J Neurosurg Sci. 2016; 60:116–125.6. Jiang B, Paff M, Colby GP, Coon AL, Lin LM. Cerebral aneurysm treatment: modern neurovascular techniques. Stroke Vasc Neurol. 2016; 1:93–100.7. Kwon OK, Han MH, Lee KJ, Oh CW, Ko YC. A technique of GDC embolization for deeply bilobulated aneurysms. AJNR Am J Neuroradiol. 2002; 23:693–696.8. Wang JT, Yang HC, Lin CF, Guo WY, Luo CB, Chen MH, et al. Bilobulated paraclinoid aneurysm mimics double aneurysms: a comparison of endovascular coiling and surgical clipping treatments. J Chin Med Assoc. 2014; 77:544–547.9. Mercado M, de Jesús O. Bilobulated aneurysms at the origin of the posterior communicating artery. P R Health Sci J. 2003; 22:405–408.10. Her Y, Jeon JP, Choi HJ, Cho YJ. Stent-assisted modified coil protection technique for bilobulated aneurysm: technical note. Radiol Case Rep. 2016; 12:146–149.11. Uricchio M, Gupta S, Jakowenko N, Levito M, Vu N, Doucette J, et al. Computed tomography angiography versus digital subtraction angiography for postclipping aneurysm obliteration detection. Stroke. 2019; 50:381–388.12. Kotowski M, Farzin B, Fahed R, Guilbert F, Chagnon M, Darsaut TE, et al. Residual cerebral aneurysms after microsurgical clipping: a new scale, an agreement study, and a systematic review of the literature. World Neurosurg. 2019; 121:e302–e321.
Article13. Goertz L, Hamisch C, Pflaeging M, Kabbasch C, Borggrefe J, Timmer M, et al. Angiographic characteristics of lobulated intracranial aneurysms. World Neurosurg. 2019; 131:e353–e361.14. Smith TR, Cote DJ, Dasenbrock HH, Hamade YJ, Zammar SG, El Tecle NE, et al. Comparison of the efficacy and safety of endovascular coiling versus microsurgical clipping for unruptured middle cerebral artery aneurysms: a systematic review and meta-analysis. World Neurosurg. 2015; 84:942–953.15. Blackburn SL, Abdelazim AM, Cutler AB, Brookins KT, Fargen KM, Hoh BL, et al. Endovascular and surgical treatment of unruptured MCA aneurysms: meta-analysis and review of the literature. Stroke Res Treat. 2014; 2014:348147.16. Nanda A, Patra DP, Bir SC, Maiti TK, Kalakoti P, Bollam P. Microsurgical clipping of unruptured intracranial aneurysms: a single surgeon’s experience over 16 years. World Neurosurg. 2017; 100:85–99.
Article17. Kotowski M, Naggara O, Darsaut TE, Nolet S, Gevry G, Kouznetsov E, et al. Safety and occlusion rates of surgical treatment of unruptured intracranial aneurysms: a systematic review and meta-analysis of the literature from 1990 to 2011. J Neurol Neurosurg Psychiatry. 2013; 84:42–48.
Article18. Kerezoudis P, McCutcheon BA, Murphy M, Rayan T, Gilder H, Rinaldo L, et al. Predictors of 30-day perioperative morbidity and mortality of unruptured intracranial aneurysm surgery. Clin Neurol Neurosurg. 2016; 149:75–80.19. Vendrell JF, Menjot N, Costalat V, Hoa D, Moritz J, Brunel H, et al. Endovascular treatment of 174 middle cerebral artery aneurysms: clinical outcome and radiologic results at long-term follow-up. Radiology. 2009; 253:191–198.20. Naggara ON, White PM, Guilbert F, Roy D, Weill A, Raymond J. Endovascular treatment of intracranial unruptured aneurysms: systematic review and meta-analysis of the literature on safety and efficacy. Radiology. 2010; 256:887–897.
Article21. Birski M, Wałęsa C, Gaca W, Paczkowski D, Birska J, Harat A. Clipping versus coiling for intracranial aneurysms. Neurol Neurochir Pol. 2014; 48:122–129.
Article22. Molyneux AJ, Birks J, Clarke A, Sneade M, Kerr RS. The durability of endovascular coiling versus neurosurgical clipping of ruptured cerebral aneurysms: 18 year follow-up of the UK cohort of the International Subarachnoid Aneurysm Trial (ISAT). Lancet. 2015; 385:691–697.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Guideline for Management of Unruptured Intracranial Aneurysms: Preliminary Report
- Current Update on the Randomized Controlled Trials of Intracranial Aneurysms
- Clinical Analysis of Surgical and Endovascular Treatment of Unruptured Intracranial Aneurysm
- Surgical Treatment of Unruptured Cerebral Aneurysms
- Feasibility of single antiplatelet therapy after stent assisted coiling for ruptured intracranial aneurysms