Neurointervention.
2024 Jul;19(2):74-81. 10.5469/neuroint.2024.00066.
Initial Experience with a New Self-Expanding Open-Cell Stent System with Antithrombotic Hydrophilic Polymer Coating (pEGASUS Stent) in the Treatment of Wide-Necked Intracranial Aneurysms
- Affiliations
-
- 1Department of Radiology and Neuroradiology, Sana Kliniken Duisburg, Duisburg, Germany
- 2Interventional Neuroradiology Department, Queen Elizabeth Hospital Birmingham, Birmingham, UK
- 3Department of Diagnostic and Interventional Neuroradiology, Medical School Hannover, Hannover, Germany
- KMID: 2556659
- DOI: http://doi.org/10.5469/neuroint.2024.00066
Abstract
- Purpose
We report our initial experience with endovascular embolization of intracranial aneurysms using this new self-expanding open-cell stent system (pEGASUS stent system) with the antithrombogenic hydrophilic polymer coating.
Materials and Methods
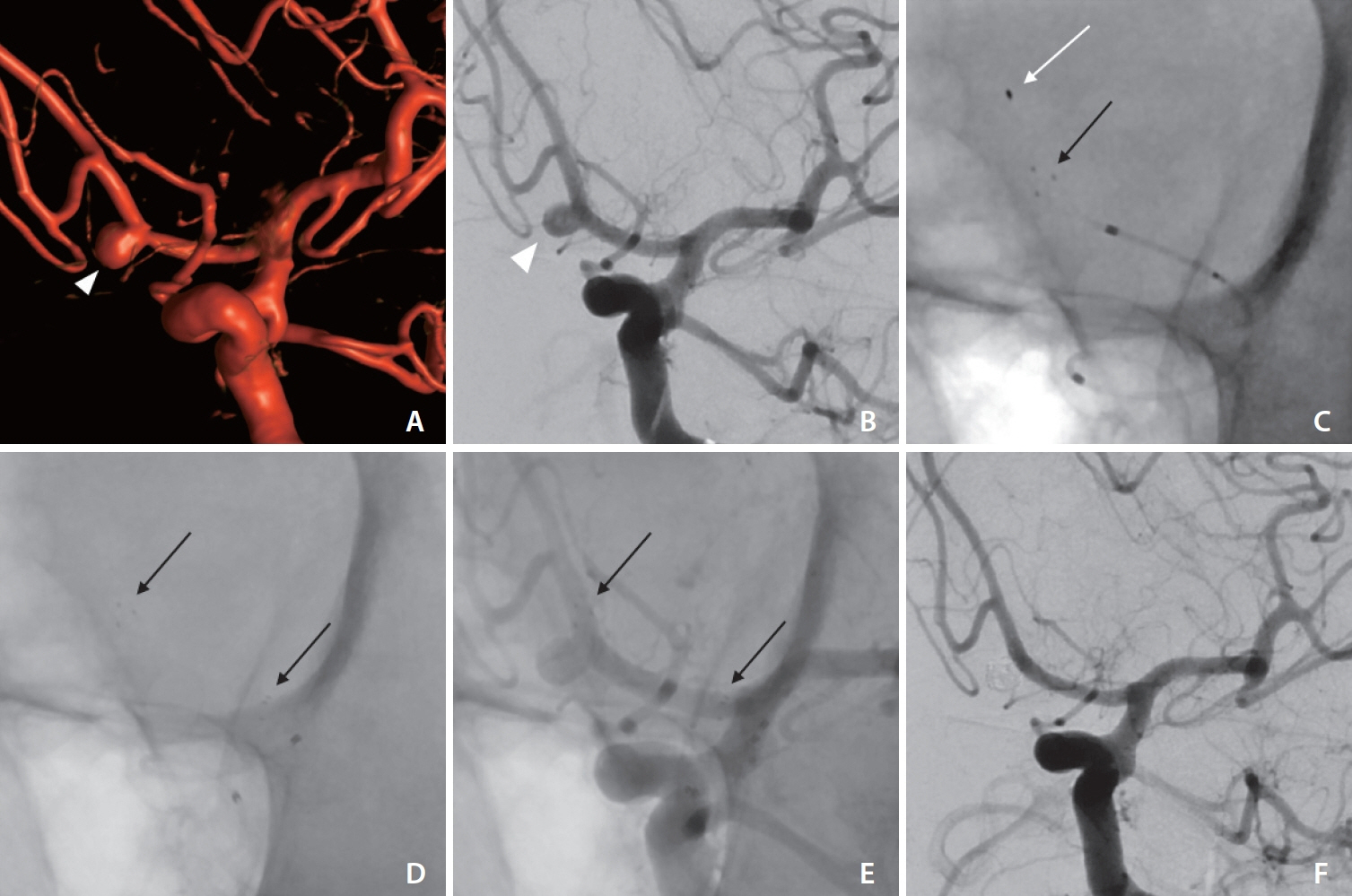
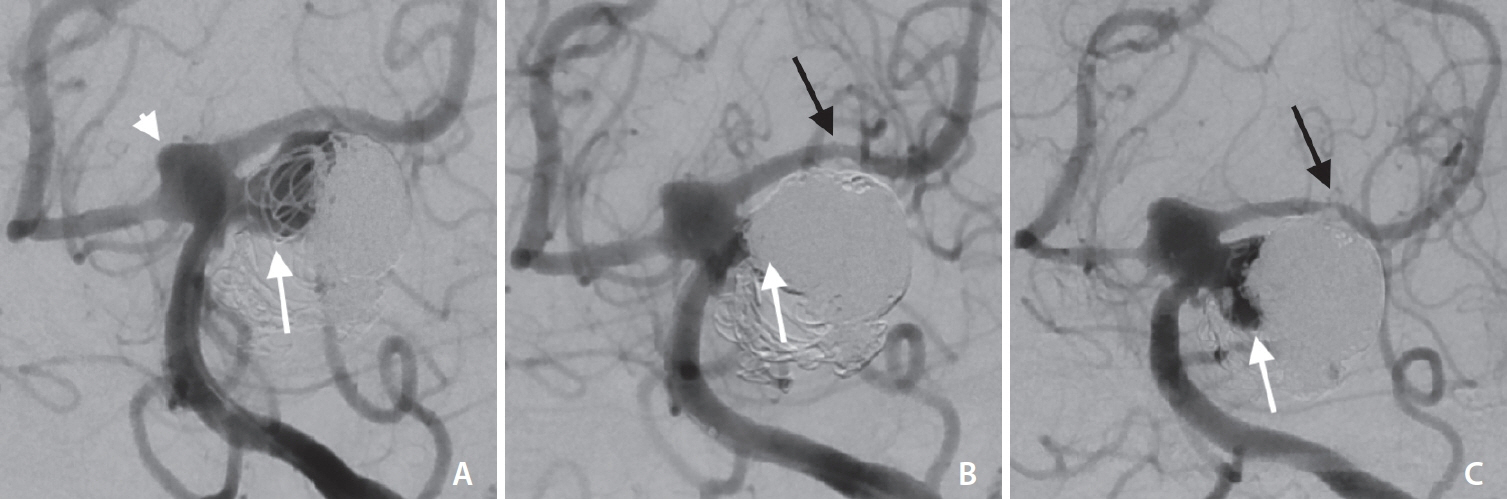
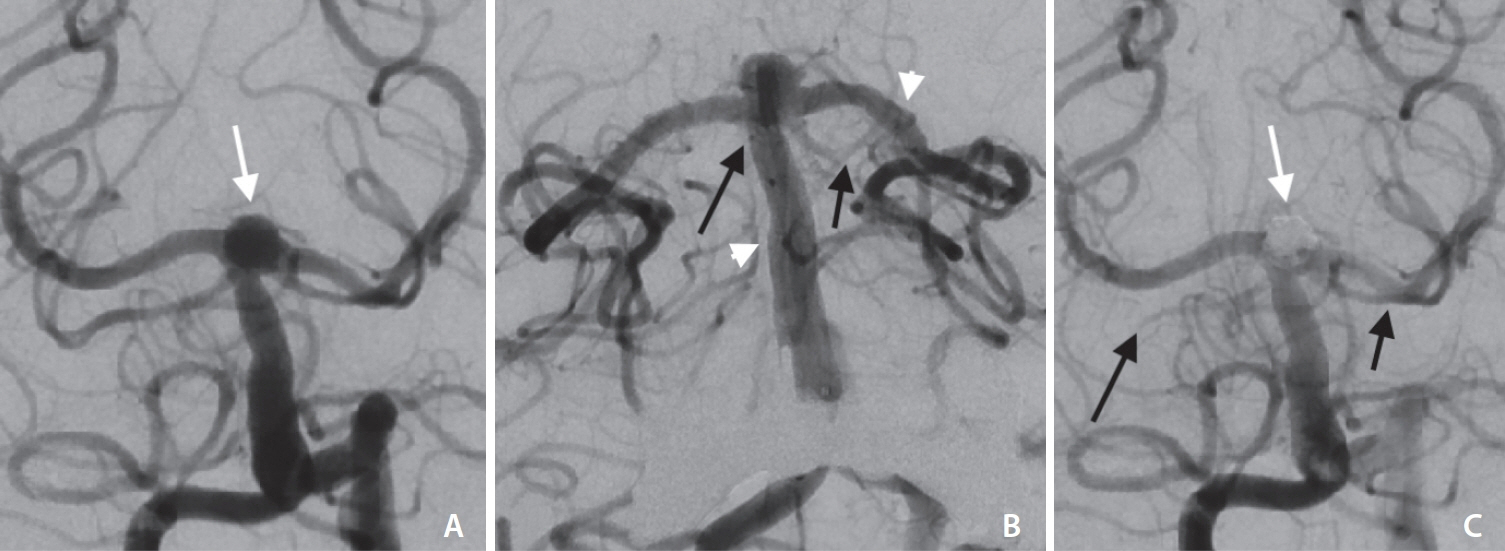
We retrospectively reviewed all patients treated with stent-assisted coiling or the Woven EndoBridge device using the pEGASUS stent system between September 2022 and June 2023. Demographic, clinical, and angiographic data were analyzed as well as short-term follow-up, including procedural complication rates and aneurysmal occlusion rates using the Raymond–Roy occlusion classification (RROC).
Results
Twelve patients with 12 wide-necked intracranial aneurysms were treated with the pEGASUS stent system, including 2 acutely ruptured aneurysms embolized in an emergency setting. The treated aneurysms were located at the anterior communicating artery (25.0%), the basilar artery (50.0%), the middle cerebral artery (16.7%), and the internal carotid artery (8.3%). All stents were deployed successfully. Immediate complete aneurysmal occlusion (RROC class I) was achieved in 83.3% (10/12) and near-complete occlusion (RROC II) in 16.7% (2/12). No periprocedural complications occurred in patients treated in the elective setting. A single case of intraoperative in-stent thrombus formation occurred during the treatment of an acutely ruptured basilar aneurysm and was resolved with intravenous Tirofiban. No other periprocedural complications occurred. Eleven out of 12 patients were available for follow up (mean 7.4 months). Complete aneurysmal occlusion without in-stent stenosis (ISS) was seen in 10 patients (90.9%). One patient (9.1%) showed aneurysmal reperfusion (RROC IIIb) with asymptomatic moderate ISS.
Conclusion
Our initial results demonstrate that the pEGASUS stent system appears to be a safe and effective device for stent assisted embolization of wide-necked intracranial aneurysms. More data is necessary to evaluate long-term follow-up.
Keyword
Figure
Reference
-
1. Poncyljusz W, Biliński P, Safranow K, Baron J, Zbroszczyk M, Jaworski M, et al. The LVIS/LVIS Jr. stents in the treatment of wideneck intracranial aneurysms: multicentre registry. J Neurointerv Surg. 2015; 7:524–529.
Article2. Zhou G, Zhu YQ, Su M, Gao KD, Li MH. Flow-diverting devices versus coil embolization for intracranial aneurysms: a systematic literature review and meta-analysis. World Neurosurg. 2016; 88:640–645.
Article3. Arthur AS, Molyneux A, Coon AL, Saatci I, Szikora I, Baltacioglu F, WEB-IT Study Investigators, et al. The safety and effectiveness of the Woven EndoBridge (WEB) system for the treatment of wide-necked bifurcation aneurysms: final 12-month results of the pivotal WEB Intrasaccular Therapy (WEB-IT) Study. J Neurointerv Surg. 2019; 11:924–930.
Article4. Piotin M, Blanc R, Spelle L, Mounayer C, Piantino R, Schmidt PJ, et al. Stent-assisted coiling of intracranial aneurysms: clinical and angiographic results in 216 consecutive aneurysms. Stroke. 2010; 41:110–115.5. Tanemura H, Ishida F, Miura Y, Umeda Y, Fukazawa K, Suzuki H, et al. Changes in hemodynamics after placing intracranial stents. Neurol Med Chir (Tokyo). 2013; 53:171–178.
Article6. Wang F, Chen X, Wang Y, Bai P, Wang HZ, Sun T, et al. Stent-assisted coiling and balloon-assisted coiling in the management of intracranial aneurysms: a systematic review & meta-analysis. J Neurol Sci. 2016; 364:160–166.
Article7. Chalouhi N, Drueding R, Starke RM, Jabbour P, Dumont AS, Gonzalez LF, et al. In-stent stenosis after stent-assisted coiling: incidence, predictors and clinical outcomes of 435 cases. Neurosurgery. 2013; 72:390–396.8. Lobsien D, Holtmannspoetter M, Eff F, Berlis A, Maurer CJ, Behme D, et al. The pEGASUS-HPC stent system for stent-assisted coiling of cerebral aneurysms: a multicenter case series. [published online ahead of print Jan 3, 2024] J Neurointerv Surg. 2024.
Article9. phenox. pEGASUS Stent System [Internet]. phenox [cited 2023 Dec 1]. Available from: https://phenox.net/international/pegasus-stent-system/.10. Poncyljusz W, Kubiak K. Initial experience with LVIS EVO stents for the treatment of intracranial aneurysms. J Clin Med. 2020; 9:3966.
Article11. Kabbasch C, Liebig T, Faymonville A, Dorn F, Mpotsaris A. Initial clinical experience with a new self-expanding nitinol microstent for the treatment of wide-neck intracranial cerebral aneurysms: the Acandis Acclino stent. J Vasc Interv Neurol. 2015; 8:1–6.12. Behme D, Weber A, Kowoll A, Berlis A, Burke TH, Weber W. Low-profile Visualized Intraluminal Support device (LVIS Jr) as a novel tool in the treatment of wide-necked intracranial aneurysms: initial experience in 32 cases. J Neurointerv Surg. 2015; 7:281–285.13. Fiorella D, Albuquerque FC, Deshmukh VR, McDougall CG. Usefulness of the Neuroform stent for the treatment of cerebral aneurysms: results at initial (3-6-mo) follow-up. Neurosurgery. 2005; 56:1191–1201. discussion 1201-1202.
Article14. Kadkhodayan Y, Rhodes N, Blackburn S, Derdeyn CP, Cross DT 3rd, Moran CJ. Comparison of Enterprise with Neuroform stent-assisted coiling of intracranial aneurysms. AJR Am J Roentgenol. 2013; 200:872–878.
Article15. Mocco J, Snyder KV, Albuquerque FC, Bendok BR, Boulos AS, Carpenter JS, et al. Treatment of intracranial aneurysms with the Enterprise stent: a multicenter registry. J Neurosurg. 2009; 110:35–39.
Article16. Weber W, Bendszus M, Kis B, Boulanger T, Solymosi L, Kühne D. A new self-expanding nitinol stent (Enterprise) for the treatment of wide-necked intracranial aneurysms: initial clinical and angiographic results in 31 aneurysms. Neuroradiology. 2007; 49:555–561.
Article17. Juszkat R, Nowak S, Smól S, Kociemba W, Blok T, Zarzecka A. Leo stent for endovascular treatment of broad-necked and fusiform intracranial aneurysms. Interv Neuroradiol. 2007; 13:255–269.18. Hou K, Yu J. Application of the Neuroform atlas stent in intracranial aneurysms: current status. Front Neurol. 2022; 13:829143.
Article19. Melber K, Boxberg FW, Schlunz-Hendann M, Brassel F, Grieb DFJ. Long-term results of wide-necked intracranial bifurcation aneurysms treated with stent-assisted coiling using low-profile acandis acclino stents. Interv Neuroradiol. 2023; 29:623–630.
Article20. Poncyljusz W, Kubiak K, Sagan L, Limanówka B, Kołaczyk K. Evaluation of the Accero stent for stent-assisted coiling of unruptured wide-necked intracranial aneurysm treatment with shortterm follow-up. J Clin Med. 2020; 9:2808.
Article21. Peltonen S, Juvela S, Kaste M, Lassila R. Hemostasis and fibrinolysis activation after subarachnoid hemorrhage. J Neurosurg. 1997; 87:207–214.
Article22. Ryu CW, Park S, Shin HS, Koh JS. Complications in stent-assisted endovascular therapy of ruptured intracranial aneurysms and relevance to antiplatelet administration: a systematic review. AJNR Am J Neuroradiol. 2015; 36:1682–1688.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Self-expanding Nitinol Stent (Enterprise) for the Treatment of Wide-necked Intracranial Aneurysms: Angiographic and Clinical Results in 40 Aneurysms
- Clinical and Angiographic Outcomes of Wide-necked Aneurysms Treated with the Solitaire AB Stent
- Endovascular Treatment of Wide-Necked Intracranial Aneurysms : Techniques and Outcomes in 15 Patients
- Preliminary Experience of Lvis Blue in the Internal Carotid Artery for The Treatment Of Wide-Necked Intracranial Aneurysms
- Y-Stenting Endovascular Treatment for Ruptured Intracranial Aneurysms : A Single-Institution Experience in Korea