Int J Thyroidol.
2024 May;17(1):193-207. 10.11106/ijt.2024.17.1.193.
Korean Thyroid Association Guidelines on the Management of Differentiated Thyroid Cancers; Part V. Pediatric Differentiated Thyroid Cancer 2024
- Affiliations
-
- 1Department of Pediatrics, Kyungpook National University Chilgok Hospital, Daegu, Korea
- 2Department of Nuclear Medicine, Seoul National University Boramae Medical Center, Seoul, Korea
- 3Department of Internal Medicine, Chonnam National University Hwasun Hospital, Hwasun, Korea
- 4Department of Otolaryngology-Head and Neck Surgery, Chungnam National University Hospital, Daejeon, Korea
- 5Department of Nuclear Medicine, Pusan National University Hospital, Busan, Korea
- 6Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 7Department of Surgery, Asan Medical Center, Seoul, Korea
- 8Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 9Department of Radiology, Gangneung Asan Hospital, Gangneung, Korea
- 10Department of Nuclear Medicine, National Cancer Center, Goyang, Korea
- 11Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 12Department of Otolaryngology-Head and Neck Surgery, Eunpyeong St. Mary’s Hospital, Seoul, Korea
- 13Department of Nuclear Medicine, CHA Bundang Medical Center, Seongnam, Korea
- 14Department of Surgery, Chung-Ang University Gwangmyeong Hospital, Gwangmyeong, Korea
- 15Department of Nuclear Medicine, Chungnam National University Sejong Hospital, Sejong, Korea
- 16Department of Internal Medicine, Seoul National University Boramae Medical Center, Seoul, Korea
- 17Department of Otolaryngology-Head and Neck Surgery, Dankook University Hospital, Cheonan, Korea
- 18Department of Otolaryngology-Head and Neck Surgery, Chungnam National University Sejong Hospital, Sejong, Korea
- 19Department of Otolaryngology-Head and Neck Surgery, National Cancer Center, Goyang, Korea
- 20Department of Nuclear Medicine, Kyungpook National University Chilgok Hospital, Daegu, Korea
- 21Department of Internal Medicine, National Cancer Center, Goyang, Korea
- 22Department of Pediatrics, Inje University Ilsan Paik Hospital, Goyang, Korea
- 23Department of Surgery, Yongin Severance Hospital, Yongin, Korea
- 24Department of Internal Medicine, Seoul St. Mary’s Hospital, Seoul, Korea
- 25Department of Otolaryngology-Head and Neck Surgery, Gangnam Severance Hospital, Seoul, Korea
- 26Department of Nuclear Medicine, Chosun University Hospital, Gwangju, Korea
- 27Department of Internal Medicine, Chung-Ang University Hospital, Seoul, Korea
- 28Department of Nuclear Medicine, Kyungpook National University Hospital, Daegu, Korea
- 29Department of Surgery, Ewha Womans University Mokdong Hospital, Seoul, Korea
- 30Department of Pediatrics, Seoul National University Children’s Hospital, Seoul, Korea
- KMID: 2556516
- DOI: http://doi.org/10.11106/ijt.2024.17.1.193
Abstract
- Pediatric differentiated thyroid cancers (DTCs), mostly papillary thyroid cancer (PTC, 80-90%), are diagnosed at more advanced stages with larger tumor sizes and higher rates of locoregional and/or lung metastasis. Despite the higher recurrence rates of pediatric cancers than of adult thyroid cancers, pediatric patients demonstrate a lower mortality rate and more favorable prognosis. Considering the more advanced stage at diagnosis in pediatric patients, preoperative evaluation is crucial to determine the extent of surgery required. Furthermore, if hereditary tumor syndrome is suspected, genetic testing is required. Recommendations for pediatric DTCs focus on the surgical principles, radioiodine therapy according to the postoperative risk level, treatment and follow-up of recurrent or persistent diseases, and treatment of patients with radioiodine-refractory PTCs on the basis of genetic drivers that are unique to pediatric patients.
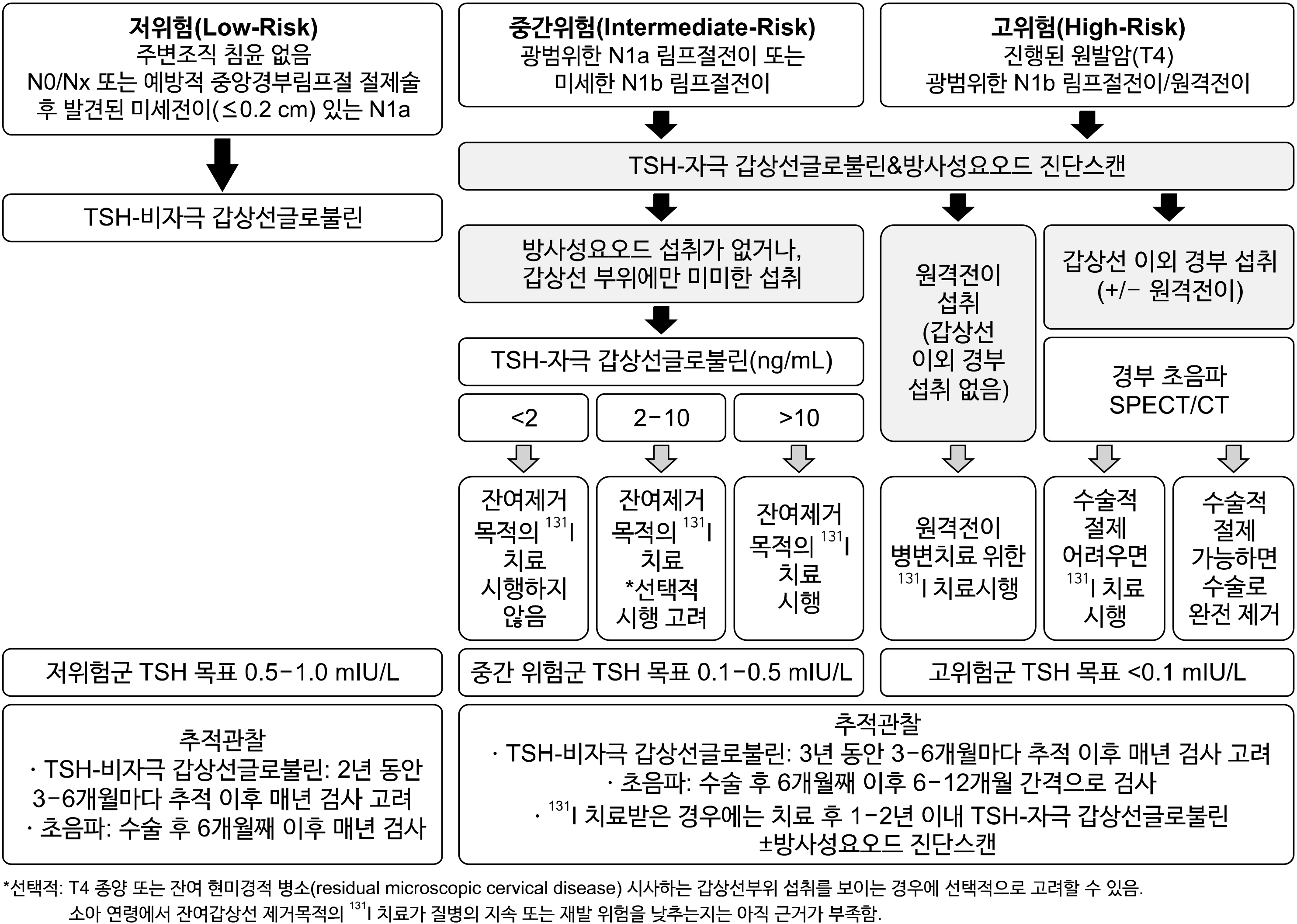
Figure
Reference
-
References
1. Lee YA, Jung HW, Kim HY, Choi H, Kim HY, Hah JH, et al. 2015; Pediatric patients with multifocal papillary thyroid cancer have higher recurrence rates than adult patients: a retrospective analysis of a large pediatric thyroid cancer cohort over 33 years. J Clin Endocrinol Metab. 100(4):1619–29. DOI: 10.1210/jc.2014-3647. PMID: 25632969.
Article2. Redlich A, Luster M, Lorenz K, Lessel L, Rohrer TR, Schmid KW, et al. 2022; Age, American Thyroid Association risk group, and response to therapy are prognostic factors in children with differentiated thyroid cancer. J Clin Endocrinol Metab. 107(1):e165–e77. DOI: 10.1210/clinem/dgab622. PMID: 34415989.
Article3. Rangel-Pozzo A, Sisdelli L, Cordioli MIV, Vaisman F, Caria P, Mai S, et al. 2020; Genetic landscape of papillary thyroid carcinoma and nuclear architecture: an overview comparing pediatric and adult populations. Cancers (Basel). 12(11):3146. DOI: 10.3390/cancers12113146. PMID: 33120984. PMCID: PMC7693829.
Article4. Lee YA, Im SW, Jung KC, Chung EJ, Shin CH, Kim JI, et al. 2020; Predominant DICER1 pathogenic variants in pediatric follicular thyroid carcinomas. Thyroid. 30(8):1120–31. DOI: 10.1089/thy.2019.0233. PMID: 32228164.
Article5. van de Berg DJ, Kuijpers AMJ, Engelsman AF, Drukker CA, van Santen HM, Terwisscha van Scheltinga S, et al. 2022; Long-term oncological outcomes of papillary thyroid cancer and follicular thyroid cancer in children: a nationwide population- based study. Front Endocrinol (Lausanne). 13:899506. DOI: 10.3389/fendo.2022.899506. PMID: 35600573. PMCID: PMC9114695.6. Stack BC Jr, Twining C, Rastatter J, Angelos P, Baloch Z, Diercks G, et al. 2021; Consensus statement by the American Association of Clinical Endocrinology (AACE) and the American Head and Neck Society Endocrine Surgery Section (AHNS-ES) on pediatric benign and malignant thyroid surgery. Head Neck. 43(4):1027–42. DOI: 10.1002/hed.26586. PMID: 33386657.
Article7. Peiling Yang S, Ngeow J. 2016; Familial non-medullary thyroid cancer: unraveling the genetic maze. Endocr Relat Cancer. 23(12):R577–R95. DOI: 10.1530/ERC-16-0067. PMID: 27807061.
Article8. Schultz KAP, Williams GM, Kamihara J, Stewart DR, Harris AK, Bauer AJ, et al. 2018; DICER1 and associated conditions: identification of at-risk individuals and recommended surveillance strategies. Clin Cancer Res. 24(10):2251–61. DOI: 10.1158/1078-0432.CCR-17-3089. PMID: 29343557. PMCID: PMC6260592.9. Jonker LA, Lebbink CA, Jongmans MCJ, Nievelstein RAJ, Merks JHM, Nieveen van Dijkum EJM, et al. 2020; Recommendations on surveillance for differentiated thyroid carcinoma in children with PTEN hamartoma tumor syndrome. Eur Thyroid J. 9(5):234–42. DOI: 10.1159/000508872. PMID: 33088791. PMCID: PMC7548843.
Article10. Tischkowitz M, Colas C, Pouwels S, Hoogerbrugge N. PHTS Guideline Development Group; European Reference Network GENTURIS. 2020; Cancer surveillance guideline for individuals with PTEN hamartoma tumour syndrome. Eur J Hum Genet. 28(10):1387–93. DOI: 10.1038/s41431-020-0651-7. PMID: 32533092. PMCID: PMC7608293.
Article11. Correa R, Salpea P, Stratakis CA. 2015; Carney complex: an update. Eur J Endocrinol. 173(4):M85–97. DOI: 10.1530/EJE-15-0209. PMID: 26130139. PMCID: PMC4553126.
Article12. Geurts JL, Strong EA, Wang TS, Evans DB, Clarke CN. 2020; Screening guidelines and recommendations for patients at high risk of developing endocrine cancers. J Surg Oncol. 121(6):975–83. DOI: 10.1002/jso.25869. PMID: 32090344.
Article13. Francis GL, Waguespack SG, Bauer AJ, Angelos P, Benvenga S, Cerutti JM, et al. 2015; Management guidelines for children with thyroid nodules and differentiated thyroid cancer. Thyroid. 25(7):716–59. DOI: 10.1089/thy.2014.0460. PMID: 25900731. PMCID: PMC4854274.
Article14. Howard SR, Freeston S, Harrison B, Izatt L, Natu S, Newbold K, et al. 2022; Paediatric differentiated thyroid carcinoma: a UK national clinical practice consensus guideline. Endocr Relat Cancer. 29(11):G1–G33. DOI: 10.1530/ERC-22-0035. PMID: 35900783. PMCID: PMC9513650.
Article15. Lebbink CA, Links TP, Czarniecka A, Dias RP, Elisei R, Izatt L, et al. 2022; 2022 European Thyroid Association guidelines for the management of pediatric thyroid nodules and differentiated thyroid carcinoma. Eur Thyroid J. 11(6):e220146. DOI: 10.1530/ETJ-22-0146. PMID: 36228315. PMCID: PMC9716393.
Article16. Bae JS, Jung SH, Hirokawa M, Bychkov A, Miyauchi A, Lee S, et al. 2021; High prevalence of DICER1 mutations and low frequency of gene fusions in pediatric follicular-patterned tumors of the thyroid. Endocr Pathol. 32(3):336–46. DOI: 10.1007/s12022-021-09688-9. PMID: 34313965.
Article17. Martucci C, Crocoli A, De Pasquale MD, Spinelli C, Strambi S, Brazzarola P, et al. 2022; Thyroid cancer in children: a multicenter international study highlighting clinical features and surgical outcomes of primary and secondary tumors. Front Pediatr. 10:914942. DOI: 10.3389/fped.2022.914942. PMID: 35935364. PMCID: PMC9354958.
Article18. Clement SC, Lebbink CA, Klein Hesselink MS, Teepen JC, Links TP, Ronckers CM, et al. 2020; Presentation and outcome of subsequent thyroid cancer among childhood cancer survivors compared to sporadic thyroid cancer: a matched national study. Eur J Endocrinol. 183(2):169–80. DOI: 10.1530/EJE-20-0153. PMID: 32449692.
Article19. van Santen HM, Alexander EK, Rivkees SA, Frey E, Clement SC, Dierselhuis MP, et al. 2020; Clinical considerations for the treatment of secondary differentiated thyroid carcinoma in childhood cancer survivors. Eur J Endocrinol. 183(3):P1–P10. DOI: 10.1530/EJE-20-0237. PMID: 32508309.
Article20. Haddy N, Diallo S, El-Fayech C, Schwartz B, Pein F, Hawkins M, et al. 2016; Cardiac diseases following childhood cancer treatment: cohort study. Circulation. 133(1):31–8. DOI: 10.1161/CIRCULATIONAHA.115.016686. PMID: 26487757.
Article21. Dietz AC, Chen Y, Yasui Y, Ness KK, Hagood JS, Chow EJ, et al. 2016; Risk and impact of pulmonary complications in survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Cancer. 122(23):3687–96. DOI: 10.1002/cncr.30200. PMID: 27504874. PMCID: PMC5115933.
Article22. van Dorp W, Mulder RL, Kremer LC, Hudson MM, van den Heuvel-Eibrink MM, van den Berg MH, et al. 2016; Recommendations for premature ovarian insufficiency surveillance for female survivors of childhood, adolescent, and young adult cancer: a report from the international late effects of childhood cancer guideline harmonization group in collaboration with the PanCareSurFup consortium. J Clin Oncol. 34(28):3440–50. DOI: 10.1200/JCO.2015.64.3288. PMID: 27458300. PMCID: PMC5569686.
Article23. Skinner R, Mulder RL, Kremer LC, Hudson MM, Constine LS, Bardi E, et al. 2017; Recommendations for gonadotoxicity surveillance in male childhood, adolescent, and young adult cancer survivors: a report from the international late effects of childhood cancer guideline harmonization group in collaboration with the PanCareSurFup consortium. Lancet Oncol. 18(2):e75–e90. DOI: 10.1016/S1470-2045(17)30026-8. PMID: 28214419.
Article24. Turcotte LM, Neglia JP, Reulen RC, Ronckers CM, van Leeuwen FE, Morton LM, et al. 2018; Risk, risk factors, and surveillance of subsequent malignant neoplasms in survivors of childhood cancer: a review. J Clin Oncol. 36(21):2145–52. DOI: 10.1200/JCO.2017.76.7764. PMID: 29874133. PMCID: PMC6075849.
Article25. Pasqual E, Schonfeld S, Morton LM, Villoing D, Lee C, Berrington de Gonzalez A, et al. 2022; Association between radioactive iodine treatment for pediatric and young adulthood differentiated thyroid cancer and risk of second primary malignancies. J Clin Oncol. 40(13):1439–49. DOI: 10.1200/JCO.21.01841. PMID: 35044839. PMCID: PMC9061144.
Article26. Machens A, Elwerr M, Schneider R, Lorenz K, Dralle H. 2018; Disease impacts more than age on operative morbidity in children with Graves' disease after total thyroidectomy. Surgery. 164(5):993–7. DOI: 10.1016/j.surg.2018.07.021. PMID: 30174139.
Article27. Bal CS, Garg A, Chopra S, Ballal S, Soundararajan R. Prognostic factors in pediatric differentiated thyroid cancer patients with pulmonary metastases. J Pediatr Endocrinol Metab. 2015; 28(7-8):745–51. DOI: 10.1515/jpem-2014-0247. PMID: 25210762.
Article28. Sugino K, Nagahama M, Kitagawa W, Shibuya H, Ohkuwa K, Uruno T, et al. 2015; Papillary thyroid carcinoma in children and adolescents: long-term follow-up and clinical characteristics. World J Surg. 39(9):2259–65. DOI: 10.1007/s00268-015-3042-4. PMID: 25802237.
Article29. Qu N, Zhang L, Lu ZW, Ji QH, Yang SW, Wei WJ, et al. 2016; Predictive factors for recurrence of differentiated thyroid cancer in patients under 21 years of age and a meta-analysis of the current literature. Tumour Biol. 37(6):7797–808. DOI: 10.1007/s13277-015-4532-6. PMID: 26695148.30. Sugino K, Nagahama M, Kitagawa W, Ohkuwa K, Uruno T, Matsuzu K, et al. 2020; Risk stratification of pediatric patients with differentiated thyroid cancer: is total thyroidectomy necessary for patients at any risk? Thyroid. 30(4):548–56. DOI: 10.1089/thy.2019.0231. PMID: 31910105.
Article31. Rubinstein JC, Dinauer C, Herrick-Reynolds K, Morotti R, Callender GG, Christison-Lagay ER. 2019; Lymph node ratio predicts recurrence in pediatric papillary thyroid cancer. J Pediatr Surg. 54(1):129–32. DOI: 10.1016/j.jpedsurg.2018.10.010. PMID: 30361076.
Article32. Olmsted C, Arunachalam R, Gao X, Pesce L, Lal G. 2017; Pediatric differentiated thyroid carcinoma: trends in practice and outcomes over 40 years at a single tertiary care institution. J Pediatr Endocrinol Metab. 30(10):1067–74. DOI: 10.1515/jpem-2016-0327. PMID: 28902626.
Article33. Baumgarten HD, Bauer AJ, Isaza A, Mostoufi-Moab S, Kazahaya K, Adzick NS. 2019; Surgical management of pediatric thyroid disease: complication rates after thyroidectomy at the Children's Hospital of Philadelphia high-volume Pediatric Thyroid Center. J Pediatr Surg. 54(10):1969–75. DOI: 10.1016/j.jpedsurg.2019.02.009. PMID: 30902456.
Article34. Spinelli C, Tognetti F, Strambi S, Morganti R, Massimino M, Collini P. 2018; Cervical lymph node metastases of papillary thyroid carcinoma, in the central and lateral compartments, in children and adolescents: predictive factors. World J Surg. 42(8):2444–53. DOI: 10.1007/s00268-018-4487-z. PMID: 29383423.
Article35. Propst EJ, Wasserman JD, Gorodensky J, Ngan BY, Wolter NE. 2021; Patterns and predictors of metastatic spread to the neck in pediatric thyroid carcinoma. Laryngoscope. 131(3):E1002–E9. DOI: 10.1002/lary.28937.
Article36. Tuggle CT, Roman SA, Wang TS, Boudourakis L, Thomas DC, Udelsman R, et al. 2008; Pediatric endocrine surgery: who is operating on our children? Surgery. 144(6):869–77. discussion 77DOI: 10.1016/j.surg.2008.08.033. PMID: 19040991.
Article37. Kao KT, Ferguson EC, Blair G, Chadha NK, Chanoine JP. 2021; Risk factors for the development of hypocalcemia in pediatric patients after total thyroidectomy - a systematic review. Int J Pediatr Otorhinolaryngol. 143:110666. DOI: 10.1016/j.ijporl.2021.110666. PMID: 33706109.
Article38. Lorenz K, Raffaeli M, Barczynski M, Lorente-Poch L, Sancho J. 2020; Volume, outcomes, and quality standards in thyroid surgery: an evidence-based analysis-European Society of Endocrine Surgeons (ESES) positional statement. Langenbecks Arch Surg. 405(4):401–25. DOI: 10.1007/s00423-020-01907-x. PMID: 32524467. PMCID: PMC8275525.
Article39. Back K, Kim TH, Lee J, Kim JS, Choe JH, Oh YL, et al. 2023; Optimal value of lymph node ratio and metastatic lymph node size to predict risk of recurrence in pediatric thyroid cancer with lateral neck metastasis. J Pediatr Surg. 58(3):568–73. DOI: 10.1016/j.jpedsurg.2022.07.010. PMID: 35973863.
Article40. Gui Y, Huang D, Hou Y, Wei X, Zhang J, Wang J. 2022; Predictive factors for recurrence of papillary thyroid carcinoma in children and adolescents. Front Oncol. 12:833775. DOI: 10.3389/fonc.2022.833775. PMID: 35280803. PMCID: PMC8909140.
Article41. Zanella A, Scheffel RS, Pasa MW, Dora JM, Maia AL. 2017; Role of postoperative stimulated thyroglobulin as prognostic factor for differentiated thyroid cancer in children and adolescents. Thyroid. 27(6):787–92. DOI: 10.1089/thy.2016.0559. PMID: 28292215.
Article42. Karapanou O, Tzanela M, Rondogianni P, Dacou-Voutetakis C, Chiotis D, Vlassopoulou B, et al. 2020; Long-term outcome of differentiated thyroid cancer in children and young adults: risk stratification by ATA criteria and assessment of pre-ablation stimulated thyroglobulin as predictors of disease persistence. Endocrine. 70(3):566–74. DOI: 10.1007/s12020-020-02378-2. PMID: 32533509.
Article43. Lazar L, Lebenthal Y, Segal K, Steinmetz A, Strenov Y, Cohen M, et al. 2016; Pediatric thyroid cancer: postoperative classifications and response to initial therapy as prognostic factors. J Clin Endocrinol Metab. 101(5):1970–9. DOI: 10.1210/jc.2015-3960. PMID: 26930182.
Article44. Pires BP, Alves PA Jr, Bordallo MA, Bulzico DA, Lopes FP, Farias T, et al. 2016; Prognostic factors for early and long-term remission in pediatric differentiated thyroid carcinoma: the role of sex, age, clinical presentation, and the newly proposed American Thyroid Association risk stratification system. Thyroid. 26(10):1480–7. DOI: 10.1089/thy.2016.0302. PMID: 27540892.
Article45. Sung TY, Jeon MJ, Lee YH, Lee YM, Kwon H, Yoon JH, et al. 2017; Initial and dynamic risk stratification of pediatric patients with differentiated thyroid cancer. J Clin Endocrinol Metab. 102(3):793–800.
Article46. Zanella AB, Scheffel RS, Nava CF, Golbert L, Laurini de Souza Meyer E, Punales M, et al. 2018; Dynamic risk stratification in the follow-up of children and adolescents with differentiated thyroid cancer. Thyroid. 28(10):1285–92. DOI: 10.1089/thy.2018.0075. PMID: 30129889.
Article47. Majeed AK, Satapathy S, Ballal S, Bal C. 2023; Dynamic risk stratification for predicting long-term outcomes in pediatric differentiated thyroid cancers. J Clin Endocrinol Metab. 108(6):e208–e15. DOI: 10.1210/clinem/dgac731. PMID: 36577747.
Article48. Padovani RP, Robenshtok E, Brokhin M, Tuttle RM. 2012; Even without additional therapy, serum thyroglobulin concentrations often decline for years after total thyroidectomy and radioactive remnant ablation in patients with differentiated thyroid cancer. Thyroid. 22(8):778–83. DOI: 10.1089/thy.2011.0522. PMID: 22780333.
Article49. Dekker BL, Muller Kobold AC, Brouwers AH, Williams GR, Nies M, Klein Hesselink MS, et al. 2021; Bone mineral density in adult survivors of pediatric differentiated thyroid carcinoma: a longitudinal follow-up study. Thyroid. 31(11):1707–14. DOI: 10.1089/thy.2021.0179. PMID: 34514857.
Article50. Chow SM, Law SC, Mendenhall WM, Au SK, Yau S, Mang O, et al. 2004; Differentiated thyroid carcinoma in childhood and adolescence-clinical course and role of radioiodine. Pediatr Blood Cancer. 42(2):176–83. DOI: 10.1002/pbc.10410. PMID: 14752883.
Article51. Jarzab B, Handkiewicz-Junak D, Wloch J. 2005; Juvenile differentiated thyroid carcinoma and the role of radioiodine in its treatment: a qualitative review. Endocr Relat Cancer. 12(4):773–803. DOI: 10.1677/erc.1.00880. PMID: 16322322.
Article52. Handkiewicz-Junak D, Wloch J, Roskosz J, Krajewska J, Kropinska A, Pomorski L, et al. 2007; Total thyroidectomy and adjuvant radioiodine treatment independently decrease locoregional recurrence risk in childhood and adolescent differentiated thyroid cancer. J Nucl Med. 48(6):879–88. DOI: 10.2967/jnumed.106.035535. PMID: 17536106.
Article53. Newman KD, Black T, Heller G, Azizkhan RG, Holcomb GW 3rd, Sklar C, et al. 1998; Differentiated thyroid cancer: determinants of disease progression in patients <21 years of age at diagnosis: a report from the Surgical Discipline Committee of the Children's Cancer Group. Ann Surg. 227(4):533–41. DOI: 10.1097/00000658-199804000-00014. PMID: 9563542. PMCID: PMC1191309.54. Haymart MR, Muenz DG, Stewart AK, Griggs JJ, Banerjee M. 2013; Disease severity and radioactive iodine use for thyroid cancer. J Clin Endocrinol Metab. 98(2):678–86. DOI: 10.1210/jc.2012-3160. PMID: 23322816. PMCID: PMC3565122.
Article55. Van Nostrand D, Wartofsky L. 2007; Radioiodine in the treatment of thyroid cancer. Endocrinol Metab Clin North Am. 36(3):807–22. DOI: 10.1016/j.ecl.2007.04.006. PMID: 17673129.
Article56. Reiners C, Biko J, Haenscheid H, Hebestreit H, Kirinjuk S, Baranowski O, et al. 2013; Twenty-five years after Chernobyl: outcome of radioiodine treatment in children and adolescents with very high-risk radiation-induced differentiated thyroid carcinoma. J Clin Endocrinol Metab. 98(7):3039–48. DOI: 10.1210/jc.2013-1059. PMID: 23616148.
Article57. Verburg FA, Biko J, Diessl S, Demidchik Y, Drozd V, Rivkees SA, et al. 2011; I-131 activities as high as safely administrable (AHASA) for the treatment of children and adolescents with advanced differentiated thyroid cancer. J Clin Endocrinol Metab. 96(8):E1268–71. DOI: 10.1210/jc.2011-0520. PMID: 21613356.
Article58. Sgouros G, Kolbert KS, Sheikh A, Pentlow KS, Mun EF, Barth A, et al. 2004; Patient-specific dosimetry for 131I thyroid cancer therapy using 124I PET and 3-dimensional-internal dosimetry (3D-ID) software. J Nucl Med. 45(8):1366–72.59. Jentzen W, Freudenberg L, Eising EG, Sonnenschein W, Knust J, Bockisch A. 2008; Optimized 124I PET dosimetry protocol for radioiodine therapy of differentiated thyroid cancer. J Nucl Med. 49(6):1017–23. DOI: 10.2967/jnumed.107.047159. PMID: 18483099.
Article60. Pettinato C, Monari F, Nanni C, Allegri V, Marcatili S, Civollani S, et al. 2012; Usefulness of 124I PET/CT imaging to predict absorbed doses in patients affected by metastatic thyroid cancer and treated with 131I. Q J Nucl Med Mol Imaging. 56(6):509–14.61. Iorcansky S, Herzovich V, Qualey RR, Tuttle RM. 2005; Serum thyrotropin (TSH) levels after recombinant human TSH injections in children and teenagers with papillary thyroid cancer. J Clin Endocrinol Metab. 90(12):6553–5. DOI: 10.1210/jc.2005-1550. PMID: 16174712.
Article62. Rosario PW, Mineiro Filho AF, Lacerda RX, Calsolari MR. 2012; Recombinant human TSH for thyroid remnant ablation with (131)I in children and adolescents with papillary carcinoma. Horm Res Paediatr. 77(1):59–62. DOI: 10.1159/000335088. PMID: 22236503.
Article63. Hoe FM, Charron M, Moshang T Jr. 2006; Use of the recombinant human TSH stimulated thyroglobulin level and diagnostic whole body scan in children with differentiated thyroid carcinoma. J Pediatr Endocrinol Metab. 19(1):25–30. DOI: 10.1515/JPEM.2006.19.1.25. PMID: 16509525.
Article64. Schumm MA, Pyo HQ, Kim J, Tseng CH, Yeh MW, Leung AM, et al. 2021; Recombinant human thyroid-stimulating hormone versus thyroid hormone withdrawal preparation for radioiodine ablation in differentiated thyroid cancer in children, adolescents and young adults. Clin Endocrinol (Oxf). 95(2):344–53. DOI: 10.1111/cen.14457. PMID: 33704813.
Article65. Hall P, Holm LE, Lundell G, Bjelkengren G, Larsson LG, Lindberg S, et al. 1991; Cancer risks in thyroid cancer patients. Br J Cancer. 64(1):159–63. DOI: 10.1038/bjc.1991.261. PMID: 1854616. PMCID: PMC1977300.
Article66. Travis CC, Stabin MG. 2006; 131I ablation treatment in young females after the Chernobyl accident. J Nucl Med. 47(10):1723–7.67. Seo GH, Kong KA, Kim BS, Kang SY, Moon BS, Yoon HJ, et al. 2021; radioactive iodine treatment for children and young adults with thyroid cancer in South Korea: a population-based study. J Clin Endocrinol Metab. 106(7):e2580–e8. DOI: 10.1210/clinem/dgab192. PMID: 33755732.
Article68. Canale D, Ceccarelli C, Caglieresi C, Moscatelli A, Gavioli S, Santini P, et al. 2015; Effects of radioiodine treatment for differentiated thyroid cancer on testis function. Clin Endocrinol (Oxf). 82(2):295–9. DOI: 10.1111/cen.12514. PMID: 25138547.
Article69. Hyer S, Vini L, O'Connell M, Pratt B, Harmer C. 2002; Testicular dose and fertility in men following I(131) therapy for thyroid cancer. Clin Endocrinol (Oxf). 56(6):755–8. DOI: 10.1046/j.1365-2265.2002.t01-1-01545.x. PMID: 12072044.70. Bourcigaux N, Rubino C, Berthaud I, Toubert ME, Donadille B, Leenhardt L, et al. 2018; Impact on testicular function of a single ablative activity of 3.7 GBq radioactive iodine for differentiated thyroid carcinoma. Hum Reprod. 33(8):1408–16. DOI: 10.1093/humrep/dey222. PMID: 29912343.
Article71. Lushbaugh CC, Casarett GW. 1976; The effects of gonadal irradiation in clinical radiation therapy: a review. Cancer. 37(2 Suppl):1111–25. DOI: 10.1002/1097-0142(197602)37:2+<1111::AID-CNCR2820370821>3.0.CO;2-E. PMID: 766956.
Article72. Sarkar SD, Beierwaltes WH, Gill SP, Cowley BJ. 1976; Subsequent fertility and birth histories of children and adolescents treated with 131I for thyroid cancer. J Nucl Med. 17(6):460–4.73. Nies M, Arts E, van Velsen EFS, Burgerhof JGM, Muller Kobold AC, Corssmit EPM, et al. 2021; Long-term male fertility after treatment with radioactive iodine for differentiated thyroid carcinoma. Eur J Endocrinol. 185(6):775–82. DOI: 10.1530/EJE-21-0315. PMID: 34582359.
Article74. Sioka C, Fotopoulos A. 2011; Effects of I-131 therapy on gonads and pregnancy outcome in patients with thyroid cancer. Fertil Steril. 95(5):1552–9. DOI: 10.1016/j.fertnstert.2011.01.017. PMID: 21300333.
Article75. Yaish I, Azem F, Gutfeld O, Silman Z, Serebro M, Sharon O, et al. 2018; A single radioactive iodine treatment has a deleterious effect on ovarian reserve in women with thyroid cancer: results of a prospective pilot study. Thyroid. 28(4):522–7. DOI: 10.1089/thy.2017.0442. PMID: 29466932.
Article76. Acibucu F, Acibucu DO, Akkar OB, Dokmetas HS. 2016; Evaluation of ovarian reserve with AMH level in patients with well-differentiated thyroid cancer receiving radioactive iodine ablation treatment. Exp Clin Endocrinol Diabetes. 124(10):593–6. DOI: 10.1055/s-0042-115639. PMID: 27711957.
Article77. Giusti M, Mittica M, Comite P, Campana C, Gay S, Mussap M. 2018; Anti-Mullerian hormone in pre-menopausal females after ablative radioiodine treatment for differentiated thyroid cancer. Endocrine. 60(3):516–23. DOI: 10.1007/s12020-017-1510-3. PMID: 29302874.
Article78. Nies M, Cantineau AEP, Arts E, van den Berg MH, van Leeuwen FE, Muller Kobold AC, et al. 2020; Long-term effects of radioiodine treatment on female fertility in survivors of childhood differentiated thyroid carcinoma. Thyroid. 30(8):1169–76. DOI: 10.1089/thy.2019.0560. PMID: 32079487.
Article79. Yan L, Zhang Y, Jiang B, Luo Y. 2021; Radiofrequency ablation for cervical metastatic lymph nodes in children and adolescents with papillary thyroid carcinoma: a preliminary study. Front Endocrinol (Lausanne). 12:624054. DOI: 10.3389/fendo.2021.624054. PMID: 34084150. PMCID: PMC8167037.
Article80. Pawelczak M, David R, Franklin B, Kessler M, Lam L, Shah B. 2010; Outcomes of children and adolescents with well-differentiated thyroid carcinoma and pulmonary metastases following 131I treatment: a systematic review. Thyroid. 20(10):1095–101. DOI: 10.1089/thy.2009.0446. PMID: 20860418.
Article81. Nies M, Vassilopoulou-Sellin R, Bassett RL, Yedururi S, Zafereo ME, Cabanillas ME, et al. 2021; Distant metastases from childhood differentiated thyroid carcinoma: clinical course and mutational landscape. J Clin Endocrinol Metab. 106(4):e1683–e97. DOI: 10.1210/clinem/dgaa935. PMID: 33382403. PMCID: PMC7993569.
Article82. Hebestreit H, Biko J, Drozd V, Demidchik Y, Burkhardt A, Trusen A, et al. 2011; Pulmonary fibrosis in youth treated with radioiodine for juvenile thyroid cancer and lung metastases after Chernobyl. Eur J Nucl Med Mol Imaging. 38(9):1683–90. DOI: 10.1007/s00259-011-1841-x. PMID: 21626048.
Article83. Lee YA, Lee H, Im SW, Song YS, Oh DY, Kang HJ, et al. 2021; NTRK and RET fusion-directed therapy in pediatric thyroid cancer yields a tumor response and radioiodine uptake. J Clin Invest. 131(18):e133847. DOI: 10.1172/JCI144847. PMID: 34237031. PMCID: PMC8439610.84. Franco AT, Ricarte-Filho JC, Isaza A, Jones Z, Jain N, Mostoufi-Moab S, et al. 2022; Fusion oncogenes are associated with increased metastatic capacity and persistent disease in pediatric thyroid cancers. J Clin Oncol. 40(10):1081–90. DOI: 10.1200/JCO.21.01861. PMID: 35015563. PMCID: PMC8966969.
Article85. Papini E, Guglielmi R, Bianchini A, Crescenzi A, Taccogna S, Nardi F, et al. 2002; Risk of malignancy in nonpalpable thyroid nodules: predictive value of ultrasound and color-Doppler features. J Clin Endocrinol Metab. 87(5):1941–6. DOI: 10.1210/jcem.87.5.8504. PMID: 11994321.
Article86. Cherella CE, Wassner AJ. 2023; Pediatric thyroid cancer: recent developments. Best Pract Res Clin Endocrinol Metab. 37(1):101715. DOI: 10.1016/j.beem.2022.101715. PMID: 36404191.
Article87. Waguespack SG, Tewari SO, Busaidy NL, Zafereo ME. 2022; Larotrectinib before initial radioactive iodine therapy in pediatric TRK fusion-positive papillary thyroid carcinoma: time to reconsider the treatment paradigm for distantly metastatic disease? JCO Precis Oncol. 6:e2100467. DOI: 10.1200/PO.21.00467. PMID: 35420905. PMCID: PMC9029926.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- ATA Guideline in a View Point of Nuclear Medicine
- Preoperative Staging of Well Differentiated Thyroid Cancer: US Is Enough?
- Differentiated Thyroid Cancer and Radioactive Iodine: Past, Present and Future
- Second Primary Malignancy after Radioiodine Treatment of Thyroid Disease: Current Status
- Evaluation and Management of Bone Health in Patients with Thyroid Diseases: A Position Statement of the Korean Thyroid Association