Int J Thyroidol.
2024 May;17(1):115-146. 10.11106/ijt.2024.17.1.115.
Korean Thyroid Association Guidelines on the Management of Differentiated Thyroid Cancers; Part II. Follow-up Surveillance after Initial Treatment 2024
- Affiliations
-
- 1Department of Internal Medicine, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea
- 2Department of Nuclear Medicine, CHA Bundang Medical Center, Seongnam, Korea
- 3Department of Internal Medicine, Chonnam National University Hwasun Hospital, Hwasun, Korea
- 4Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 5Department of Radiology, Gangneung Asan Hospital, Gangneung, Korea
- 6Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 7Department of Nuclear Medicine, Chungnam National University Sejong Hospital, Sejong, Korea
- 8Department of Internal Medicine, Seoul National University Boramae Medical Center, Seoul, Korea
- 9Department of Nuclear Medicine, Seoul National University Boramae Medical Center, Seoul, Korea
- 10Department of Nuclear Medicine, Kyungpook National University Chilgok Hospital, Daegu, Korea
- 11Department of Internal Medicine, National Cancer Center, Goyang, Korea
- 12Department of Radiology, Seoul National University Hospital, Seoul, Korea
- 13Department of Internal Medicine, Seoul St. Mary’s Hospital, Seoul, Korea
- 14Department of Nuclear Medicine, Chosun University Hospital, Gwangju, Korea
- 15Department of Internal Medicine, Chung-Ang University Hospital, Seoul, Korea
- 16Department of Nuclear Medicine, Kyungpook National University Hospital, Daegu, Korea
- 17Department of Radiology, Yeouido St. Mary’s Hospital, Seoul, Korea
- KMID: 2556510
- DOI: http://doi.org/10.11106/ijt.2024.17.1.115
Abstract
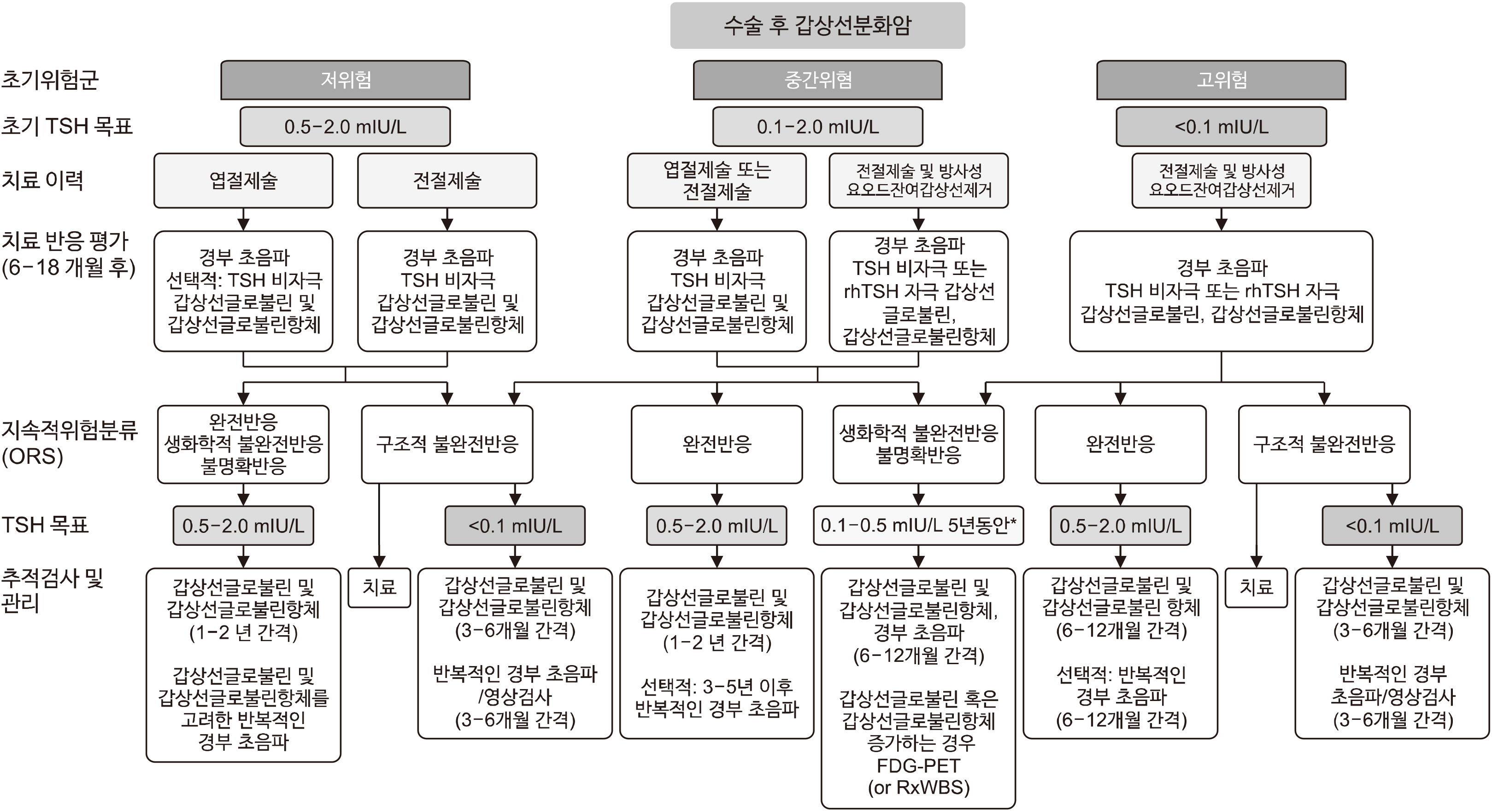
- Based on the clinical, histopathological, and perioperative data of a patient with differentiated thyroid cancer (DTC), risk stratification based on their initial recurrence risk is a crucial follow-up (FU) strategy during the first 1–2 years after initial therapy. However, restratifiying the recurrence risk on the basis of current clinical data that becomes available after considering the response to treatment (ongoing risk stratification, ORS) provides a more accurate prediction of the status at the final FU and a more tailored management approach. Since the 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and DTC, the latest guidelines that include the National Comprehensive Cancer Network clinical practice and European Association for Medical Oncology guidelines have been updated to reflect several recent evidence in ORS and thyroid-stimulating hormone (TSH) suppression of DTC. The current clinical practice guideline was developed by extracting FU surveillance after the initial treatment section from the previous version of guidelines and updating it to reflect recent evidence. The current revised guideline includes recommendations for recent ORS, TSH target level based on risk stratification, FU tools for detection of recurrence and assessment of disease status, and long-term FU strategy for consideration of the disease status. These evidence-based recommendations are expected to avoid overtreatment and intensive FU of the majority of patients who will have a very good prognosis after the initial treatment of DTC patients, thereby ensuring that patients receive the most appropriate and effective treatment and FU options.
Keyword
Figure
Reference
-
References
1. Kim S, Wei JP, Braveman JM, Brams DM. 2004; Predicting outcome and directing therapy for papillary thyroid carcinoma. Arch Surg. 139(4):390–4. discussion 3–4. DOI: 10.1001/archsurg.139.4.390. PMID: 15078706.
Article2. Links TP, van Tol KM, Jager PL, Plukker JT, Piers DA, Boezen HM, et al. 2005; Life expectancy in differentiated thyroid cancer: a novel approach to survival analysis. Endocr Relat Cancer. 12(2):273–80. DOI: 10.1677/erc.1.00892. PMID: 15947102.
Article3. Bogdanovski AK, Sturgeon C, James BC. 2023; Financial toxicity in thyroid cancer survivors. Curr Opin Endocrinol Diabetes Obes. 30(5):238–43. DOI: 10.1097/MED.0000000000000826. PMID: 37470486.
Article4. Mongelli MN, Giri S, Peipert BJ, Helenowski IB, Yount SE, Sturgeon C. 2020; Financial burden and quality of life among thyroid cancer survivors. Surgery. 167(3):631–7. DOI: 10.1016/j.surg.2019.11.014. PMID: 31862171.
Article5. Tuttle RM, Tala H, Shah J, Leboeuf R, Ghossein R, Gonen M, et al. 2010; Estimating risk of recurrence in differentiated thyroid cancer after total thyroidectomy and radioactive iodine remnant ablation: using response to therapy variables to modify the initial risk estimates predicted by the new American Thyroid Association staging system. Thyroid. 20(12):1341–9. DOI: 10.1089/thy.2010.0178. PMID: 21034228. PMCID: PMC4845674.
Article6. Tuttle RM, Leboeuf R. 2008; Follow up approaches in thyroid cancer: a risk adapted paradigm. Endocrinol Metab Clin North Am. 37(2):419–35. ix–x. DOI: 10.1016/j.ecl.2008.02.008. PMID: 18502335.
Article7. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2016; 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 26(1):1–133. DOI: 10.1089/thy.2015.0020. PMID: 26462967. PMCID: PMC4739132.
Article8. Momesso DP, Tuttle RM. 2014; Update on differentiated thyroid cancer staging. Endocrinol Metab Clin North Am. 43(2):401–21. DOI: 10.1016/j.ecl.2014.02.010. PMID: 24891169.
Article9. Verburg FA, Stokkel MP, Duren C, Verkooijen RB, Mader U, van Isselt JW, et al. 2010; No survival difference after successful (131)I ablation between patients with initially low-risk and high-risk differentiated thyroid cancer. Eur J Nucl Med Mol Imaging. 37(2):276–83. DOI: 10.1007/s00259-009-1315-6. PMID: 20091165.
Article10. Shen FC, Hsieh CJ, Huang IC, Chang YH, Wang PW. 2017; Dynamic risk estimates of outcome in Chinese patients with well-differentiated thyroid cancer after total thyroidectomy and radioactive iodine remnant ablation. Thyroid. 27(4):531–6. DOI: 10.1089/thy.2016.0479. PMID: 28007013.
Article11. Vaisman F, Momesso D, Bulzico DA, Pessoa CH, Dias F, Corbo R, et al. 2012; Spontaneous remission in thyroid cancer patients after biochemical incomplete response to initial therapy. Clin Endocrinol (Oxf). 77(1):132–8. DOI: 10.1111/j.1365-2265.2012.04342.x. PMID: 22248037.
Article12. Llamas-Olier AE, Cuellar DI, Buitrago G. 2018; Intermediate-risk papillary thyroid cancer: risk factors for early recurrence in patients with excellent response to initial therapy. Thyroid. 28(10):1311–7. DOI: 10.1089/thy.2017.0578. PMID: 30105948.
Article13. Robbins RJ, Wan Q, Grewal RK, Reibke R, Gonen M, Strauss HW, et al. 2006; Real-time prognosis for metastatic thyroid carcinoma based on 2-[18F]fluoro-2-deoxy-D-glucose-positron emission tomography scanning. J Clin Endocrinol Metab. 91(2):498–505. DOI: 10.1210/jc.2005-1534. PMID: 16303836.
Article14. Deandreis D, Al Ghuzlan A, Leboulleux S, Lacroix L, Garsi JP, Talbot M, et al. 2011; Do histological, immunohistochemical, and metabolic (radioiodine and fluorodeoxyglucose uptakes) patterns of metastatic thyroid cancer correlate with patient outcome? Endocr Relat Cancer. 18(1):159–69. DOI: 10.1677/ERC-10-0233. PMID: 21118976.
Article15. Miyauchi A, Kudo T, Miya A, Kobayashi K, Ito Y, Takamura Y, et al. 2011; Prognostic impact of serum thyroglobulin doubling-time under thyrotropin suppression in patients with papillary thyroid carcinoma who underwent total thyroidectomy. Thyroid. 21(7):707–16. DOI: 10.1089/thy.2010.0355. PMID: 21649472.
Article16. Chou R, Dana T, Brent GA, Goldner W, Haymart M, Leung AM, et al. 2022; Serum thyroglobulin measurement following surgery without radioactive iodine for differentiated thyroid cancer: a systematic review. Thyroid. 32(6):613–39. DOI: 10.1089/thy.2021.0666. PMID: 35412871.
Article17. Filetti S, Durante C, Hartl D, Leboulleux S, Locati LD, Newbold K, et al. 2019; Thyroid cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 30(12):1856–83. DOI: 10.1093/annonc/mdz400. PMID: 31549998.
Article18. Pitoia F, Jerkovich F. 2019; Dynamic risk assessment in patients with differentiated thyroid cancer. Endocr Relat Cancer. 26(10):R553–R66. DOI: 10.1530/ERC-19-0213. PMID: 31394499.
Article19. Castagna MG, Maino F, Cipri C, Belardini V, Theodoropoulou A, Cevenini G, et al. 2011; Delayed risk stratification, to include the response to initial treatment (surgery and radioiodine ablation), has better outcome predictivity in differentiated thyroid cancer patients. Eur J Endocrinol. 165(3):441–6. DOI: 10.1530/EJE-11-0466. PMID: 21750043.
Article20. Vaisman F, Tala H, Grewal R, Tuttle RM. 2011; In differentiated thyroid cancer, an incomplete structural response to therapy is associated with significantly worse clinical outcomes than only an incomplete thyroglobulin response. Thyroid. 21(12):1317–22. DOI: 10.1089/thy.2011.0232. PMID: 22136267.
Article21. Cano-Palomares A, Castells I, Capel I, Bella MR, Barcons S, Serrano A, et al. 2014; Response to initial therapy of differentiated thyroid cancer predicts the long-term outcome better than classical risk stratification systems. Int J Endocrinol. 2014:591285. DOI: 10.1155/2014/591285. PMID: 25114681. PMCID: PMC4121103.
Article22. Jeon MJ, Kim WG, Park WR, Han JM, Kim TY, Song DE, et al. 2014; Modified dynamic risk stratification for predicting recurrence using the response to initial therapy in patients with differentiated thyroid carcinoma. Eur J Endocrinol. 170(1):23–30. DOI: 10.1530/EJE-13-0524. PMID: 24088549.
Article23. Schlumberger M, Leboulleux S, Catargi B, Deandreis D, Zerdoud S, Bardet S, et al. 2018; Outcome after ablation in patients with low-risk thyroid cancer (ESTIMABL1): 5-year follow-up results of a randomised, phase 3, equivalence trial. Lancet Diabetes Endocrinol. 6(8):618–26. DOI: 10.1016/S2213-8587(18)30113-X. PMID: 29807824.
Article24. Han JM, Kim WB, Yim JH, Kim WG, Kim TY, Ryu JS, et al. 2012; Long-term clinical outcome of differentiated thyroid cancer patients with undetectable stimulated thyroglobulin level one year after initial treatment. Thyroid. 22(8):784–90. DOI: 10.1089/thy.2011.0322. PMID: 22780573. PMCID: PMC3407383.
Article25. Rosario PW, Furtado MS, Mineiro Filho AF, Lacerda RX, Calsolari MR. 2012; Value of repeat stimulated thyroglobulin testing in patients with differentiated thyroid carcinoma considered to be free of disease in the first year after ablation. Thyroid. 22(5):482–6. DOI: 10.1089/thy.2011.0214. PMID: 22175271.
Article26. Momesso DP, Vaisman F, Yang SP, Bulzico DA, Corbo R, Vaisman M, et al. 2016; Dynamic risk stratification in patients with differentiated thyroid cancer treated without radioactive iodine. J Clin Endocrinol Metab. 101(7):2692–700. DOI: 10.1210/jc.2015-4290. PMID: 27023446. PMCID: PMC6287503.
Article27. Park S, Kim WG, Song E, Oh HS, Kim M, Kwon H, et al. 2017; Dynamic risk stratification for predicting recurrence in patients with differentiated thyroid cancer treated without radioactive iodine remnant ablation therapy. Thyroid. 27(4):524–30. DOI: 10.1089/thy.2016.0477. PMID: 27869547.
Article28. Sung TY, Cho JW, Lee YM, Lee YH, Kwon H, Jeon MJ, et al. 2017; Dynamic risk stratification in stage I papillary thyroid cancer patients younger than 45 years of age. Thyroid. 27(11):1400–7. DOI: 10.1089/thy.2017.0199. PMID: 28847226.
Article29. Cho JW, Lee YM, Lee YH, Hong SJ, Yoon JH. 2018; Dynamic risk stratification system in post-lobectomy low-risk and intermediate-risk papillary thyroid carcinoma patients. Clin Endocrinol (Oxf). 89(1):100–9. DOI: 10.1111/cen.13721. PMID: 29672893.
Article30. Dong P, Wang L, Xiao L, Yang L, Huang R, Li L. 2021; A new dynamic response to therapy assessment in postoperative patients with low-risk differentiated thyroid cancer treated without radioactive iodine. Front Oncol. 11:764258. DOI: 10.3389/fonc.2021.764258. PMID: 34912712. PMCID: PMC8667687.
Article31. Abelleira E, Jerkovich F. 2024; Dynamic risk assessment in patients with differentiated thyroid cancer. Rev Endocr Metab Disord. 25(1):79–93. DOI: 10.1007/s11154-023-09857-7. PMID: 38015344.
Article32. Park S, Jeon MJ, Oh HS, Lee YM, Sung TY, Han M, et al. 2018; Changes in serum thyroglobulin levels after lobectomy in patients with low-risk papillary thyroid cancer. Thyroid. 28(8):997–1003. DOI: 10.1089/thy.2018.0046. PMID: 29845894.
Article33. Schuff KG, Weber SM, Givi B, Samuels MH, Andersen PE, Cohen JI. 2008; Efficacy of nodal dissection for treatment of persistent/recurrent papillary thyroid cancer. Laryngoscope. 118(5):768–75. DOI: 10.1097/MLG.0b013e318162cae9. PMID: 18197134.
Article34. Al-Saif O, Farrar WB, Bloomston M, Porter K, Ringel MD, Kloos RT. 2010; Long-term efficacy of lymph node reoperation for persistent papillary thyroid cancer. J Clin Endocrinol Metab. 95(5):2187–94. DOI: 10.1210/jc.2010-0063. PMID: 20332244. PMCID: PMC5399471.
Article35. Yim JH, Kim WB, Kim EY, Kim WG, Kim TY, Ryu JS, et al. 2011; The outcomes of first reoperation for locoregionally recurrent/persistent papillary thyroid carcinoma in patients who initially underwent total thyroidectomy and remnant ablation. J Clin Endocrinol Metab. 96(7):2049–56. DOI: 10.1210/jc.2010-2298. PMID: 21508143.
Article36. Landa I, Ibrahimpasic T, Boucai L, Sinha R, Knauf JA, Shah RH, et al. 2016; Genomic and transcriptomic hallmarks of poorly differentiated and anaplastic thyroid cancers. J Clin Invest. 126(3):1052–66. DOI: 10.1172/JCI85271. PMID: 26878173. PMCID: PMC4767360.
Article37. Kim TH, Ki CS, Kim HS, Kim K, Choe JH, Kim JH, et al. 2017; Refining dynamic risk stratification and prognostic groups for differentiated thyroid cancer with TERT promoter mutations. J Clin Endocrinol Metab. 102(5):1757–64. DOI: 10.1210/jc.2016-3434. PMID: 28323925.
Article38. Song YS, Lim JA, Choi H, Won JK, Moon JH, Cho SW, et al. 2016; Prognostic effects of TERT promoter mutations are enhanced by coexistence with BRAF or RAS mutations and strengthen the risk prediction by the ATA or TNM staging system in differentiated thyroid cancer patients. Cancer. 122(9):1370–9. DOI: 10.1002/cncr.29934. PMID: 26969876.
Article39. Diessl S, Holzberger B, Mader U, Grelle I, Smit JW, Buck AK, et al. 2012; Impact of moderate vs stringent TSH suppression on survival in advanced differentiated thyroid carcinoma. Clin Endocrinol (Oxf). 76(4):586–92. DOI: 10.1111/j.1365-2265.2011.04272.x. PMID: 22059804.40. McGriff NJ, Csako G, Gourgiotis L, Lori CG, Pucino F, Sarlis NJ. Effects of thyroid hormone suppression therapy on adverse clinical outcomes in thyroid cancer. Ann Med. 2002; 34(7-8):554–64. DOI: 10.1080/078538902321117760. PMID: 12553495.
Article41. Haymart MR, Repplinger DJ, Leverson GE, Elson DF, Sippel RS, Jaume JC, et al. 2008; Higher serum thyroid stimulating hormone level in thyroid nodule patients is associated with greater risks of differentiated thyroid cancer and advanced tumor stage. J Clin Endocrinol Metab. 93(3):809–14. DOI: 10.1210/jc.2007-2215. PMID: 18160464. PMCID: PMC2266959.
Article42. Brabant G. 2008; Thyrotropin suppressive therapy in thyroid carcinoma: what are the targets? J Clin Endocrinol Metab. 93(4):1167–9. DOI: 10.1210/jc.2007-2228. PMID: 18390811.
Article43. Toft AD. 2001; Clinical practice. Subclinical hyperthyroidism. N Engl J Med. 345(7):512–6. DOI: 10.1056/NEJMcp010145. PMID: 11519506.44. Biondi B, Cooper DS. 2010; Benefits of thyrotropin suppression versus the risks of adverse effects in differentiated thyroid cancer. Thyroid. 20(2):135–46. DOI: 10.1089/thy.2009.0311. PMID: 20151821.
Article45. Biondi B, Fazio S, Cuocolo A, Sabatini D, Nicolai E, Lombardi G, et al. 1996; Impaired cardiac reserve and exercise capacity in patients receiving long-term thyrotropin suppressive therapy with levothyroxine. J Clin Endocrinol Metab. 81(12):4224–8. DOI: 10.1210/jcem.81.12.8954019. PMID: 8954019.
Article46. Pajamaki N, Metso S, Hakala T, Ebeling T, Huhtala H, Ryodi E, et al. 2018; Long-term cardiovascular morbidity and mortality in patients treated for differentiated thyroid cancer. Clin Endocrinol (Oxf). 88(2):303–10. DOI: 10.1111/cen.13519. PMID: 29154445.
Article47. Lee EK, Ahn HY, Ku EJ, Yoo WS, Lee YK, Nam KH, et al. 2021; Cardiovascular outcomes in thyroid cancer patients treated with thyroidectomy: a meta-analysis. J Clin Endocrinol Metab. 106(12):3644–54. DOI: 10.1210/clinem/dgab576. PMID: 34347085.
Article48. Vestergaard P, Mosekilde L. 2002; Fractures in patients with hyperthyroidism and hypothyroidism: a nationwide follow-up study in 16,249 patients. Thyroid. 12(5):411–9. DOI: 10.1089/105072502760043503. PMID: 12097203.
Article49. Biondi B, Cooper DS. 2019; Thyroid hormone suppression therapy. Endocrinol Metab Clin North Am. 48(1):227–37. DOI: 10.1016/j.ecl.2018.10.008. PMID: 30717904.
Article50. Heemstra KA, Hamdy NA, Romijn JA, Smit JW. 2006; The effects of thyrotropin-suppressive therapy on bone metabolism in patients with well-differentiated thyroid carcinoma. Thyroid. 16(6):583–91. DOI: 10.1089/thy.2006.16.583. PMID: 16839260.
Article51. Yoon BH, Lee Y, Oh HJ, Kim SH, Lee YK. 2019; Influence of thyroid-stimulating hormone suppression therapy on bone mineral density in patients with differentiated thyroid cancer: a meta-analysis. J Bone Metab. 26(1):51–60. DOI: 10.11005/jbm.2019.26.1.51. PMID: 30899725. PMCID: PMC6416150.
Article52. Wang LY, Smith AW, Palmer FL, Tuttle RM, Mahrous A, Nixon IJ, et al. 2015; Thyrotropin suppression increases the risk of osteoporosis without decreasing recurrence in ATA low- and intermediate-risk patients with differentiated thyroid carcinoma. Thyroid. 25(3):300–7. DOI: 10.1089/thy.2014.0287. PMID: 25386760. PMCID: PMC6916125.
Article53. Ku EJ, Yoo WS, Lee EK, Ahn HY, Woo SH, Hong JH, et al. 2021; Effect of TSH suppression therapy on bone mineral density in differentiated thyroid cancer: a systematic review and meta-analysis. J Clin Endocrinol Metab. 106(12):3655–67. DOI: 10.1210/clinem/dgab539. PMID: 34302730.
Article54. Kwak D, Ha J, Won Y, Kwon Y, Park S. 2021; Effects of thyroid-stimulating hormone suppression after thyroidectomy for thyroid cancer on bone mineral density in postmenopausal women: a systematic review and meta-analysis. BMJ Open. 11(5):e043007. DOI: 10.1136/bmjopen-2020-043007. PMID: 33986046. PMCID: PMC8126273.
Article55. Tagay S, Herpertz S, Langkafel M, Erim Y, Freudenberg L, Schopper N, et al. 2005; Health-related quality of life, anxiety and depression in thyroid cancer patients under short-term hypothyroidism and TSH-suppressive levothyroxine treatment. Eur J Endocrinol. 153(6):755–63. DOI: 10.1530/eje.1.02047. PMID: 16322380.
Article56. Lee JK, Ku EJ, Kim SJ, Kim W, Cho JW, Jung KY, et al. 2024; Effect of thyroid-stimulating hormone suppression on quality of life in thyroid lobectomy patients: interim analysis of a multicenter, randomized controlled trial in low- to intermediate-risk thyroid cancer patients (MASTER study). Ann Surg Treat Res. 106(1):19–30. DOI: 10.4174/astr.2024.106.1.19. PMID: 38205091. PMCID: PMC10774702.
Article57. Thyroid cancer: assessment and management. NICE guideline, No. 230. London: National Institute for Health and Care Excellence (NICE);2022.58. Watson-Brown P, Anderson D. Differentiated thyroid cancer: a guide to survivorship care. Aust J Gen Pract. 2023; 52(1-2):47–51. DOI: 10.31128/AJGP-02-22-6327. PMID: 36796772.
Article59. Carhill AA, Litofsky DR, Ross DS, Jonklaas J, Cooper DS, Brierley JD, et al. 2015; Long-term outcomes following therapy in differentiated thyroid carcinoma: NTCTCS registry analysis 1987-2012. J Clin Endocrinol Metab. 100(9):3270–9. DOI: 10.1210/JC.2015-1346. PMID: 26171797. PMCID: PMC5393522.
Article60. Sugitani I, Fujimoto Y. 2010; Does postoperative thyrotropin suppression therapy truly decrease recurrence in papillary thyroid carcinoma? A randomized controlled trial. J Clin Endocrinol Metab. 95(10):4576–83. DOI: 10.1210/jc.2010-0161. PMID: 20660039.
Article61. Abo-Touk NA, Zayed DH. 2015; The efficacy of thyrotropin suppression therapy in treatment of differentiated thyroid cancer after total thyroidectomy. Forum Clin Oncol. 6(2):24–33. DOI: 10.1515/fco-2015-0010.
Article62. Lamartina L, Montesano T, Falcone R, Biffoni M, Grani G, Maranghi M, et al. 2019; Is it worth suppressing TSH in low- and intermediate-risk papillary thyroid cancer patients before the first disease assessment? Endocr Pract. 25(2):165–9. DOI: 10.4158/EP-2018-0393. PMID: 30383494.
Article63. Lee MC, Kim MJ, Choi HS, Cho SW, Lee GH, Park YJ, et al. 2019; Postoperative thyroid-stimulating hormone levels did not affect recurrence after thyroid lobectomy in patients with papillary thyroid cancer. Endocrinol Metab (Seoul). 34(2):150–7. DOI: 10.3803/EnM.2019.34.2.150. PMID: 31099202. PMCID: PMC6599911.
Article64. Park JH, Lee YM, Lee YH, Hong SJ, Yoon JH. 2018; The prognostic value of serum thyroid-stimulating hormone level post-lobectomy in low- and intermediate-risk papillary thyroid carcinoma. J Surg Oncol. 118(3):390–6. DOI: 10.1002/jso.25164. PMID: 30114333.
Article65. Park S, Kim WG, Han M, Jeon MJ, Kwon H, Kim M, et al. 2017; Thyrotropin suppressive therapy for low-risk small thyroid cancer: a propensity score-matched cohort study. Thyroid. 27(9):1164–70. DOI: 10.1089/thy.2017.0177. PMID: 28699428.
Article66. Xu S, Huang Y, Huang H, Zhang X, Qian J, Wang X, et al. 2022; Optimal serum thyrotropin level for patients with papillary thyroid carcinoma after lobectomy. Thyroid. 32(2):138–44. DOI: 10.1089/thy.2021.0404. PMID: 34617446.
Article67. Ahn D, Lee GJ, Sohn JH, Jeon JH. 2020; Oncological impact of hypothyroidism and levothyroxine supplementation following hemithyroidectomy in patients with papillary thyroid carcinoma. Head Neck. 42(5):1004–13. DOI: 10.1002/hed.26075. PMID: 31930773.
Article68. Klubo-Gwiezdzinska J, Auh S, Gershengorn M, Daley B, Bikas A, Burman K, et al. 2019; Association of thyrotropin suppression with survival outcomes in patients with intermediate- and high-risk differentiated thyroid cancer. JAMA Netw Open. 2(2):e187754. DOI: 10.1001/jamanetworkopen.2018.7754. PMID: 30707227. PMCID: PMC6484595.
Article69. Abiri A, Nguyen T, Goshtasbi K, Torabi SJ, Kuan EC, Armstrong WB, et al. 2023; A comparative analysis of treatment efficacy in intermediate-risk thyroid cancer. Eur Arch Otorhinolaryngol. 280(5):2525–33. DOI: 10.1007/s00405-023-07832-1. PMID: 36651960.
Article70. Ito Y, Masuoka H, Fukushima M, Inoue H, Kihara M, Tomoda C, et al. 2010; Prognosis and prognostic factors of patients with papillary carcinoma showing distant metastasis at surgery (M1 patients) in Japan. Endocr J. 57(6):523–31. DOI: 10.1507/endocrj.K10E-019. PMID: 20379035.
Article71. Mukhtar N, Aljamei H, Aljomaiah A, Moria Y, Alzahrani AS. 2021; Natural course of the American Thyroid Association response to therapy statuses (dynamic risk stratification) in differentiated thyroid cancer. Eur Thyroid J. 10(3):198–207. DOI: 10.1159/000511708. PMID: 34178705. PMCID: PMC8216009.
Article72. Won HR, Jeon E, Chang JW, Kang YE, Song K, Kim SW, et al. 2022; Is maintaining thyroid-stimulating hormone effective in patients undergoing thyroid lobectomy for low-risk differentiated thyroid cancer? A systematic review and meta-analysis. Cancers (Basel). 14(6):1470. DOI: 10.3390/cancers14061470. PMID: 35326621. PMCID: PMC8946503.
Article73. Jonklaas J, Sarlis NJ, Litofsky D, Ain KB, Bigos ST, Brierley JD, et al. 2006; Outcomes of patients with differentiated thyroid carcinoma following initial therapy. Thyroid. 16(12):1229–42. DOI: 10.1089/thy.2006.16.1229. PMID: 17199433.
Article74. Hovens GC, Stokkel MP, Kievit J, Corssmit EP, Pereira AM, Romijn JA, et al. 2007; Associations of serum thyrotropin concentrations with recurrence and death in differentiated thyroid cancer. J Clin Endocrinol Metab. 92(7):2610–5. DOI: 10.1210/jc.2006-2566. PMID: 17426094.
Article75. Lee EK, Kang YE, Park YJ, Koo BS, Chung KW, Ku EJ, et al. 2021; A multicenter, randomized, controlled trial for assessing the usefulness of suppressing thyroid stimulating hormone target levels after thyroid lobectomy in low to intermediate risk thyroid cancer patients (MASTER): a study protocol. Endocrinol Metab (Seoul). 36(3):574–81. DOI: 10.3803/EnM.2020.943. PMID: 34034365. PMCID: PMC8258337.
Article76. Papaleontiou M, Chen DW, Banerjee M, Reyes-Gastelum D, Hamilton AS, Ward KC, et al. 2021; Thyrotropin suppression for papillary thyroid cancer: a physician survey study. Thyroid. 31(9):1383–90. DOI: 10.1089/thy.2021.0033. PMID: 33779292. PMCID: PMC8558057.
Article77. Klein Hesselink EN, Klein Hesselink MS, de Bock GH, Gansevoort RT, Bakker SJ, Vredeveld EJ, et al. 2013; Long-term cardiovascular mortality in patients with differentiated thyroid carcinoma: an observational study. J Clin Oncol. 31(32):4046–53. DOI: 10.1200/JCO.2013.49.1043. PMID: 24101052.
Article78. Yu J, Kaur R, Ayeni FE, Eslick GD, Edirimanne S. 2023; Cardiovascular outcomes of differentiated thyroid cancer patients on long term TSH suppression: a systematic review and meta-analysis. Horm Metab Res. 55(6):379–87. DOI: 10.1055/a-2084-3408. PMID: 37295414.
Article79. Shargorodsky M, Serov S, Gavish D, Leibovitz E, Harpaz D, Zimlichman R. 2006; Long-term thyrotropin-suppressive therapy with levothyroxine impairs small and large artery elasticity and increases left ventricular mass in patients with thyroid carcinoma. Thyroid. 16(4):381–6. DOI: 10.1089/thy.2006.16.381. PMID: 16646685.
Article80. Taillard V, Sardinoux M, Oudot C, Fesler P, Rugale C, Raingeard I, et al. 2011; Early detection of isolated left ventricular diastolic dysfunction in high-risk differentiated thyroid carcinoma patients on TSH-suppressive therapy. Clin Endocrinol (Oxf). 75(5):709–14. DOI: 10.1111/j.1365-2265.2011.04138.x. PMID: 21645022.
Article81. Gigliotti BJ, Jasim S. 2024; Differentiated thyroid cancer: a focus on post-operative thyroid hormone replacement and thyrotropin suppression therapy. Endocrine. 83(2):251–8. DOI: 10.1007/s12020-023-03548-8. PMID: 37824045.
Article82. Feldt-Rasmussen U, Klose M. Feingold KR, Anawalt B, Blackman MR, Boyce A, Chrousos G, Corpas E, editors. Clinical strategies in the testing of thyroid function. Endotext. South Dartmouth (MA): 2000.83. Cox C, Bosley M, Southerland LB, Ahmadi S, Perkins J, Roman S, et al. 2018; Lobectomy for treatment of differentiated thyroid cancer: can patients avoid postoperative thyroid hormone supplementation and be compliant with the American Thyroid Association guidelines? Surgery. 163(1):75–80. DOI: 10.1016/j.surg.2017.04.039. PMID: 29122328.
Article84. Morris LF, Iupe IM, Edeiken-Monroe BS, Warneke CL, Hansen MO, Evans DB, et al. 2013; Pre-operative ultrasound identification of thyroiditis helps predict the need for thyroid hormone replacement after thyroid lobectomy. Endocr Pract. 19(6):1015–20. DOI: 10.4158/EP12334.OR. PMID: 24013973.
Article85. Kim SY, Kim HJ, Kim SM, Chang H, Lee YS, Chang HS, et al. 2020; Thyroid hormone supplementation therapy for differentiated thyroid cancer after lobectomy: 5 years of follow-up. Front Endocrinol (Lausanne). 11:520. DOI: 10.3389/fendo.2020.00520. PMID: 32849303. PMCID: PMC7412630.
Article86. Lawton RI, Sabatini BL, Hochbaum DR. 2024; Longevity, demographic characteristics, and socio-economic status are linked to triiodothyronine levels in the general population. Proc Natl Acad Sci U S A. 121(2):e2308652121. DOI: 10.1073/pnas.2308652121. PMID: 38175866. PMCID: PMC10786306.
Article87. Wiersinga WM. 2014; Paradigm shifts in thyroid hormone replacement therapies for hypothyroidism. Nat Rev Endocrinol. 10(3):164–74. DOI: 10.1038/nrendo.2013.258. PMID: 24419358.
Article88. DiStefano J 3rd, Jonklaas J. 2019; Predicting optimal combination LT4 + LT3 therapy for hypothyroidism based on residual thyroid function. Front Endocrinol (Lausanne). 10:746. DOI: 10.3389/fendo.2019.00746. PMID: 31803137. PMCID: PMC6873785.
Article89. Salvatore D, Porcelli T, Ettleson MD, Bianco AC. 2022; The relevance of T(3) in the management of hypothyroidism. Lancet Diabetes Endocrinol. 10(5):366–72. DOI: 10.1016/S2213-8587(22)00004-3. PMID: 35240052.
Article90. Baudin E, Do Cao C, Cailleux AF, Leboulleux S, Travagli JP, Schlumberger M. 2003; Positive predictive value of serum thyroglobulin levels, measured during the first year of follow-up after thyroid hormone withdrawal, in thyroid cancer patients. J Clin Endocrinol Metab. 88(3):1107–11. DOI: 10.1210/jc.2002-021365. PMID: 12629092.91. Schaap J, Eustatia-Rutten CF, Stokkel M, Links TP, Diamant M, van der Velde EA, et al. 2002; Does radioiodine therapy have disadvantageous effects in non-iodine accumulating differentiated thyroid carcinoma? Clin Endocrinol (Oxf). 57(1):117–24. DOI: 10.1046/j.1365-2265.2002.01574.x. PMID: 12100079.
Article92. Pacini F, Sabra MM, Tuttle RM. 2011; Clinical relevance of thyroglobulin doubling time in the management of patients with differentiated thyroid cancer. Thyroid. 21(7):691–2. DOI: 10.1089/thy.2011.2107.ed1. PMID: 21707434.
Article93. van Kinschot CMJ, Peeters RP, van den Berg SAA, Verburg FA, van Noord C, van Ginhoven TM, et al. 2022; Thyroglobulin and thyroglobulin antibodies: assay-dependent management consequences in patients with differentiated thyroid carcinoma. Clin Chem Lab Med. 60(5):756–65. DOI: 10.1515/cclm-2021-1046. PMID: 35108464.
Article94. Spencer CA. 2011; Clinical review: clinical utility of thyroglobulin antibody (TgAb) measurements for patients with differentiated thyroid cancers (DTC). J Clin Endocrinol Metab. 96(12):3615–27. DOI: 10.1210/jc.2011-1740. PMID: 21917876.95. Gorges R, Maniecki M, Jentzen W, Sheu SN, Mann K, Bockisch A, et al. 2005; Development and clinical impact of thyroglobulin antibodies in patients with differentiated thyroid carcinoma during the first 3 years after thyroidectomy. Eur J Endocrinol. 153(1):49–55. DOI: 10.1530/eje.1.01940. PMID: 15994745.
Article96. Latrofa F, Ricci D, Montanelli L, Rocchi R, Piaggi P, Sisti E, et al. 2012; Lymphocytic thyroiditis on histology correlates with serum thyroglobulin autoantibodies in patients with papillary thyroid carcinoma: impact on detection of serum thyroglobulin. J Clin Endocrinol Metab. 97(7):2380–7. DOI: 10.1210/jc.2011-2812. PMID: 22539585.
Article97. Spencer C, Fatemi S. 2013; Thyroglobulin antibody (TgAb) methods - strengths, pitfalls and clinical utility for monitoring TgAb-positive patients with differentiated thyroid cancer. Best Pract Res Clin Endocrinol Metab. 27(5):701–12. DOI: 10.1016/j.beem.2013.07.003. PMID: 24094640.
Article98. Kim WG, Yoon JH, Kim WB, Kim TY, Kim EY, Kim JM, et al. 2008; Change of serum antithyroglobulin antibody levels is useful for prediction of clinical recurrence in thyroglobulin- negative patients with differentiated thyroid carcinoma. J Clin Endocrinol Metab. 93(12):4683–9. DOI: 10.1210/jc.2008-0962. PMID: 18812478.99. Verburg FA, Luster M, Cupini C, Chiovato L, Duntas L, Elisei R, et al. 2013; Implications of thyroglobulin antibody positivity in patients with differentiated thyroid cancer: a clinical position statement. Thyroid. 23(10):1211–25. DOI: 10.1089/thy.2012.0606. PMID: 23692026.
Article100. Spencer CA, Takeuchi M, Kazarosyan M, Wang CC, Guttler RB, Singer PA, et al. 1998; Serum thyroglobulin autoantibodies: prevalence, influence on serum thyroglobulin measurement, and prognostic significance in patients with differentiated thyroid carcinoma. J Clin Endocrinol Metab. 83(4):1121–7. DOI: 10.1210/jc.83.4.1121. PMID: 9543128.
Article101. Chiovato L, Latrofa F, Braverman LE, Pacini F, Capezzone M, Masserini L, et al. 2003; Disappearance of humoral thyroid autoimmunity after complete removal of thyroid antigens. Ann Intern Med. 139(5 Pt 1):346–51. DOI: 10.7326/0003-4819-139-5_Part_1-200309020-00010. PMID: 12965943.
Article102. Thomas D, Liakos V, Vassiliou E, Hatzimarkou F, Tsatsoulis A, Kaldrimides P. 2007; Possible reasons for different pattern disappearance of thyroglobulin and thyroid peroxidase autoantibodies in patients with differentiated thyroid carcinoma following total thyroidectomy and iodine-131 ablation. J Endocrinol Invest. 30(3):173–80. DOI: 10.1007/BF03347421. PMID: 17505148.
Article103. Chung JK, Park YJ, Kim TY, So Y, Kim SK, Park DJ, et al. 2002; Clinical significance of elevated level of serum antithyroglobulin antibody in patients with differentiated thyroid cancer after thyroid ablation. Clin Endocrinol (Oxf). 57(2):215–21. DOI: 10.1046/j.1365-2265.2002.01592.x. PMID: 12153600.
Article104. Adil A, Jafri RA, Waqar A, Abbasi SA, Matiul H, Asghar AH, et al. 2003; Frequency and clinical importance of anti-Tg auto-antibodies (ATG). J Coll Physicians Surg Pak. 13(9):504–6.105. Lee ZJO, Eslick GD, Edirimanne S. 2020; Investigating antithyroglobulin antibody as a prognostic marker for differentiated thyroid cancer: a meta-analysis and systematic review. Thyroid. 30(11):1601–12. DOI: 10.1089/thy.2019.0368. PMID: 32345152.
Article106. Webb RC, Howard RS, Stojadinovic A, Gaitonde DY, Wallace MK, Ahmed J, et al. 2012; The utility of serum thyroglobulin measurement at the time of remnant ablation for predicting disease-free status in patients with differentiated thyroid cancer: a meta-analysis involving 3947 patients. J Clin Endocrinol Metab. 97(8):2754–63. DOI: 10.1210/jc.2012-1533. PMID: 22639291.
Article107. Eustatia-Rutten CF, Smit JW, Romijn JA, van der Kleij-Corssmit EP, Pereira AM, Stokkel MP, et al. 2004; Diagnostic value of serum thyroglobulin measurements in the follow-up of differentiated thyroid carcinoma, a structured meta-analysis. Clin Endocrinol (Oxf). 61(1):61–74. DOI: 10.1111/j.1365-2265.2004.02060.x. PMID: 15212646.
Article108. Schlumberger M, Berg G, Cohen O, Duntas L, Jamar F, Jarzab B, et al. 2004; Follow-up of low-risk patients with differentiated thyroid carcinoma: a European perspective. Eur J Endocrinol. 150(2):105–12. DOI: 10.1530/eje.0.1500105. PMID: 14763906.
Article109. Bachelot A, Leboulleux S, Baudin E, Hartl DM, Caillou B, Travagli JP, et al. 2005; Neck recurrence from thyroid carcinoma: serum thyroglobulin and high-dose total body scan are not reliable criteria for cure after radioiodine treatment. Clin Endocrinol (Oxf). 62(3):376–9. DOI: 10.1111/j.1365-2265.2005.02228.x. PMID: 15730423.
Article110. Giovanella L, Suriano S, Ceriani L, Verburg FA. 2011; Undetectable thyroglobulin in patients with differentiated thyroid carcinoma and residual radioiodine uptake on a postablation whole-body scan. Clin Nucl Med. 36(2):109–12. DOI: 10.1097/RLU.0b013e318203bb84. PMID: 21220971.
Article111. Cherk MH, Francis P, Topliss DJ, Bailey M, Kalff V. 2012; Incidence and implications of negative serum thyroglobulin but positive I-131 whole-body scans in patients with well- differentiated thyroid cancer prepared with rhTSH or thyroid hormone withdrawal. Clin Endocrinol (Oxf). 76(5):734–40. DOI: 10.1111/j.1365-2265.2011.04278.x. PMID: 22050475.112. Torlontano M, Crocetti U, Augello G, D'Aloiso L, Bonfitto N, Varraso A, et al. 2006; Comparative evaluation of recombinant human thyrotropin-stimulated thyroglobulin levels, 131I whole-body scintigraphy, and neck ultrasonography in the follow-up of patients with papillary thyroid microcarcinoma who have not undergone radioiodine therapy. J Clin Endocrinol Metab. 91(1):60–3. DOI: 10.1210/jc.2005-1185. PMID: 16219716.113. Pacini F, Agate L, Elisei R, Capezzone M, Ceccarelli C, Lippi F, et al. 2001; Outcome of differentiated thyroid cancer with detectable serum Tg and negative diagnostic (131)I whole body scan: comparison of patients treated with high (131)I activities versus untreated patients. J Clin Endocrinol Metab. 86(9):4092–7. DOI: 10.1210/jcem.86.9.7831. PMID: 11549631.
Article114. Frasoldati A, Pesenti M, Gallo M, Caroggio A, Salvo D, Valcavi R. 2003; Diagnosis of neck recurrences in patients with differentiated thyroid carcinoma. Cancer. 97(1):90–6. DOI: 10.1002/cncr.11031. PMID: 12491509.
Article115. Castagna MG, Brilli L, Pilli T, Montanaro A, Cipri C, Fioravanti C, et al. 2008; Limited value of repeat recombinant human thyrotropin (rhTSH)-stimulated thyroglobulin testing in differentiated thyroid carcinoma patients with previous negative rhTSH-stimulated thyroglobulin and undetectable basal serum thyroglobulin levels. J Clin Endocrinol Metab. 93(1):76–81. DOI: 10.1210/jc.2007-1404. PMID: 17971424.
Article116. Kloos RT, Mazzaferri EL. 2005; A single recombinant human thyrotropin-stimulated serum thyroglobulin measurement predicts differentiated thyroid carcinoma metastases three to five years later. J Clin Endocrinol Metab. 90(9):5047–57. DOI: 10.1210/jc.2005-0492. PMID: 15972576.
Article117. Klubo-Gwiezdzinska J, Burman KD, Van Nostrand D, Wartofsky L. 2011; Does an undetectable rhTSH-stimulated Tg level 12 months after initial treatment of thyroid cancer indicate remission? Clin Endocrinol (Oxf). 74(1):111–7. DOI: 10.1111/j.1365-2265.2010.03898.x. PMID: 21054476.118. Diaz-Soto G, Puig-Domingo M, Martinez-Pino I, Martinez de Osaba MJ, Mora M, Rivera-Fillat F, et al. 2011; Do thyroid cancer patients with basal undetectable Tg measured by current immunoassays require rhTSH testing? Exp Clin Endocrinol Diabetes. 119(6):348–52. DOI: 10.1055/s-0030-1269881. PMID: 21264807.
Article119. Castagna MG, Tala Jury HP, Cipri C, Belardini V, Fioravanti C, Pasqui L, et al. 2011; The use of ultrasensitive thyroglobulin assays reduces but does not abolish the need for TSH stimulation in patients with differentiated thyroid carcinoma. J Endocrinol Invest. 34(8):e219–23.120. Nascimento C, Borget I, Al Ghuzlan A, Deandreis D, Chami L, Travagli JP, et al. 2011; Persistent disease and recurrence in differentiated thyroid cancer patients with undetectable postoperative stimulated thyroglobulin level. Endocr Relat Cancer. 18(2):R29–40. DOI: 10.1677/ERC-10-0292. PMID: 21183629.
Article121. Padovani RP, Robenshtok E, Brokhin M, Tuttle RM. 2012; Even without additional therapy, serum thyroglobulin concentrations often decline for years after total thyroidectomy and radioactive remnant ablation in patients with differentiated thyroid cancer. Thyroid. 22(8):778–83. DOI: 10.1089/thy.2011.0522. PMID: 22780333.
Article122. Mazzaferri EL, Robbins RJ, Spencer CA, Braverman LE, Pacini F, Wartofsky L, et al. 2003; A consensus report of the role of serum thyroglobulin as a monitoring method for low-risk patients with papillary thyroid carcinoma. J Clin Endocrinol Metab. 88(4):1433–41. DOI: 10.1210/jc.2002-021702. PMID: 12679418.
Article123. Haugen BR, Pacini F, Reiners C, Schlumberger M, Ladenson PW, Sherman SI, et al. 1999; A comparison of recombinant human thyrotropin and thyroid hormone withdrawal for the detection of thyroid remnant or cancer. J Clin Endocrinol Metab. 84(11):3877–85. DOI: 10.1210/jc.84.11.3877. PMID: 10566623.
Article124. David A, Blotta A, Bondanelli M, Rossi R, Roti E, Braverman LE, et al. 2001; Serum thyroglobulin concentrations and (131)I whole-body scan results in patients with differentiated thyroid carcinoma after administration of recombinant human thyroid-stimulating hormone. J Nucl Med. 42(10):1470–5.125. Mazzaferri EL, Kloos RT. 2002; Is diagnostic iodine-131 scanning with recombinant human TSH useful in the follow-up of differentiated thyroid cancer after thyroid ablation? J Clin Endocrinol Metab. 87(4):1490–8. DOI: 10.1210/jcem.87.4.8338. PMID: 11932270.
Article126. Haugen BR, Ridgway EC, McLaughlin BA, McDermott MT. 2002; Clinical comparison of whole-body radioiodine scan and serum thyroglobulin after stimulation with recombinant human thyrotropin. Thyroid. 12(1):37–43. DOI: 10.1089/105072502753451959. PMID: 11838729.
Article127. Lima N, Cavaliere H, Tomimori E, Knobel M, Medeiros- Neto G. 2002; Prognostic value of serial serum thyroglobulin determinations after total thyroidectomy for differentiated thyroid cancer. J Endocrinol Invest. 25(2):110–5. DOI: 10.1007/BF03343973. PMID: 11929080.
Article128. Wartofsky L. rhTSH-Stimulated Thyroglobulin Study Group. 2002; Management of low-risk well-differentiated thyroid cancer based only on thyroglobulin measurement after recombinant human thyrotropin. Thyroid. 12(7):583–90. DOI: 10.1089/105072502320288438. PMID: 12193302.
Article129. Durante C, Montesano T, Attard M, Torlontano M, Monzani F, Costante G, et al. 2012; Long-term surveillance of papillary thyroid cancer patients who do not undergo postoperative radioiodine remnant ablation: is there a role for serum thyroglobulin measurement? J Clin Endocrinol Metab. 97(8):2748–53. DOI: 10.1210/jc.2012-1123. PMID: 22679061.
Article130. Giovanella L, Ceriani L, Garo ML. 2022; Is thyroglobulin a reliable biomarker of differentiated thyroid cancer in patients treated by lobectomy? A systematic review and meta-analysis. Clin Chem Lab Med. 60(7):1091–100. DOI: 10.1515/cclm-2022-0154. PMID: 35475431.
Article131. Ullmann TM, Papaleontiou M, Sosa JA. 2023; Current controversies in low-risk differentiated thyroid cancer: reducing overtreatment in an era of overdiagnosis. J Clin Endocrinol Metab. 108(2):271–80. DOI: 10.1210/clinem/dgac646. PMID: 36327392. PMCID: PMC10091361.
Article132. Rosario PW, Cortes MCS, Franco Mourao G. 2021; Follow-up of patients with thyroid cancer and antithyroglobulin antibodies: a review for clinicians. Endocr Relat Cancer. 28(4):R111–R9. DOI: 10.1530/ERC-21-0012. PMID: 33690160.
Article133. American Institute of Ultrasound in Medicine. 2003; AIUM Practice Guideline for the performance of thyroid and parathyroid ultrasound examination. J Ultrasound Med. 22(10):1126–30. DOI: 10.7863/jum.2003.22.10.1126. PMID: 14606572.134. Lee JY, Baek JH, Ha EJ, Sung JY, Shin JH, Kim JH, et al. 2021; 2020 imaging guidelines for thyroid nodules and differentiated thyroid cancer: Korean Society of Thyroid Radiology. Korean J Radiol. 22(5):840–60. DOI: 10.3348/kjr.2020.0578. PMID: 33660459. PMCID: PMC8076832.
Article135. Yeh MW, Bauer AJ, Bernet VA, Ferris RL, Loevner LA, Mandel SJ, et al. 2015; American Thyroid Association statement on preoperative imaging for thyroid cancer surgery. Thyroid. 25(1):3–14. DOI: 10.1089/thy.2014.0096. PMID: 25188202. PMCID: PMC5248547.
Article136. Lepoutre-Lussey C, Maddah D, Golmard JL, Russ G, Tissier F, Tresallet C, et al. 2014; Post-operative neck ultrasound and risk stratification in differentiated thyroid cancer patients with initial lymph node involvement. Eur J Endocrinol. 170(6):837–46. DOI: 10.1530/EJE-13-0888. PMID: 24659355.
Article137. Jiang HJ, Wu CW, Chiang FY, Chiou HC, Chen IJ, Hsiao PJ. 2018; Reliable sonographic features for nodal thyroglobulin to diagnose recurrent lymph node metastasis from papillary thyroid carcinoma. Clin Otolaryngol. 43(4):1065–72. DOI: 10.1111/coa.13103. PMID: 29575557.
Article138. Hoang JK, Oldan JD, Mandel SJ, Policeni B, Agarwal V, et al. Expert Panel on Neurological Imaging. 2019; ACR Appropriateness Criteria((R)) thyroid disease. J Am Coll Radiol. 16(5S):S300–S14. DOI: 10.1016/j.jacr.2019.02.004. PMID: 31054756.139. Perros P, Boelaert K, Colley S, Evans C, Evans RM, Gerrard Ba G, et al. 2014; Guidelines for the management of thyroid cancer. Clin Endocrinol (Oxf). 81 Suppl 1:1–122. DOI: 10.1111/cen.12515. PMID: 24989897.
Article140. Leenhardt L, Erdogan MF, Hegedus L, Mandel SJ, Paschke R, Rago T, et al. 2013; 2013 European Thyroid Association guidelines for cervical ultrasound scan and ultrasound-guided techniques in the postoperative management of patients with thyroid cancer. Eur Thyroid J. 2(3):147–59. DOI: 10.1159/000354537. PMID: 24847448. PMCID: PMC4017749.
Article141. Yoo RE, Kim JH, Bae JM, Hwang I, Kang KM, Yun TJ, et al. 2020; Ultrasonographic indeterminate lymph nodes in preoperative thyroid cancer patients: malignancy risk and ultrasonographic findings predictive of malignancy. Korean J Radiol. 21(5):598–604. DOI: 10.3348/kjr.2019.0755. PMID: 32323505. PMCID: PMC7183832.
Article142. Leboulleux S, Girard E, Rose M, Travagli JP, Sabbah N, Caillou B, et al. 2007; Ultrasound criteria of malignancy for cervical lymph nodes in patients followed up for differentiated thyroid cancer. J Clin Endocrinol Metab. 92(9):3590–4. DOI: 10.1210/jc.2007-0444. PMID: 17609301.
Article143. Park JS, Son KR, Na DG, Kim E, Kim S. 2009; Performance of preoperative sonographic staging of papillary thyroid carcinoma based on the sixth edition of the AJCC/UICC TNM classification system. AJR Am J Roentgenol. 192(1):66–72. DOI: 10.2214/AJR.07.3731. PMID: 19098181.
Article144. Rosario PW, de Faria S, Bicalho L, Alves MF, Borges MA, Purisch S, et al. 2005; Ultrasonographic differentiation between metastatic and benign lymph nodes in patients with papillary thyroid carcinoma. J Ultrasound Med. 24(10):1385–9. DOI: 10.7863/jum.2005.24.10.1385. PMID: 16179622.
Article145. Sohn YM, Kwak JY, Kim EK, Moon HJ, Kim SJ, Kim MJ. 2010; Diagnostic approach for evaluation of lymph node metastasis from thyroid cancer using ultrasound and fine-needle aspiration biopsy. AJR Am J Roentgenol. 194(1):38–43. DOI: 10.2214/AJR.09.3128. PMID: 20028903.
Article146. Chung SR, Baek JH, Rho YH, Choi YJ, Sung TY, Song DE, et al. 2022; Sonographic diagnosis of cervical lymph node metastasis in patients with thyroid cancer and comparison of European and Korean guidelines for stratifying the risk of malignant lymph node. Korean J Radiol. 23(11):1102–11. DOI: 10.3348/kjr.2022.0358. PMID: 36126955. PMCID: PMC9614289.
Article147. Lee JY, Yoo RE, Rhim JH, Lee KH, Choi KS, Hwang I, et al. 2022; Validation of ultrasound risk stratification systems for cervical lymph node metastasis in patients with thyroid cancer. Cancers (Basel). 14(9):2106. DOI: 10.3390/cancers14092106. PMID: 35565235. PMCID: PMC9105025.
Article148. Hahn SY, Shin JH, Han BK, Ko EY, Kang SS, Chung JH, et al. 2011; Predictive factors related to the recurrence at US-guided fine needle aspiration in postoperative patients with differentiated thyroid cancer. Clin Endocrinol (Oxf). 74(2):270–5. DOI: 10.1111/j.1365-2265.2010.03915.x. PMID: 21044120.
Article149. Lee JH, Lee HK, Lee DH, Choi CG, Gong G, Shong YK, et al. 2007; Ultrasonographic findings of a newly detected nodule on the thyroid bed in postoperative patients for thyroid carcinoma: correlation with the results of ultrasonography-guided fine- needle aspiration biopsy. Clin Imaging. 31(2):109–13. DOI: 10.1016/j.clinimag.2006.11.001. PMID: 17320777.150. Frates MC, Parziale MP, Alexander EK, Barletta JA, Benson CB. 2021; Role of sonographic characteristics of thyroid bed lesions identified following thyroidectomy in the diagnosis or exclusion of recurrent cancer. Radiology. 299(2):374–80. DOI: 10.1148/radiol.2021201596. PMID: 33650902.
Article151. Ha EJ, Chung SR, Na DG, Ahn HS, Chung J, Lee JY, et al. 2021; 2021 Korean Thyroid Imaging Reporting and Data System and imaging-based management of thyroid nodules: Korean Society of Thyroid Radiology consensus statement and recommendations. Korean J Radiol. 22(12):2094–123. DOI: 10.3348/kjr.2021.0713. PMID: 34719893. PMCID: PMC8628155.
Article152. Lee JI, Chung YJ, Cho BY, Chong S, Seok JW, Park SJ. 2013; Postoperative-stimulated serum thyroglobulin measured at the time of 131I ablation is useful for the prediction of disease status in patients with differentiated thyroid carcinoma. Surgery. 153(6):828–35. DOI: 10.1016/j.surg.2012.12.008. PMID: 23489940.
Article153. Pacini F, Basolo F, Bellantone R, Boni G, Cannizzaro MA, De Palma M, et al. 2018; Italian consensus on diagnosis and treatment of differentiated thyroid cancer: joint statements of six Italian societies. J Endocrinol Invest. 41(7):849–76. DOI: 10.1007/s40618-018-0884-2. PMID: 29729004.
Article154. Lee SG, Lee WK, Lee HS, Moon J, Lee CR, Kang SW, et al. 2017; Practical performance of the 2015 American Thyroid Association guidelines for predicting tumor recurrence in patients with papillary thyroid cancer in South Korea. Thyroid. 27(2):174–81. DOI: 10.1089/thy.2016.0252. PMID: 27750028.
Article155. Rondeau G, Fish S, Hann LE, Fagin JA, Tuttle RM. 2011; Ultrasonographically detected small thyroid bed nodules identified after total thyroidectomy for differentiated thyroid cancer seldom show clinically significant structural progression. Thyroid. 21(8):845–53. DOI: 10.1089/thy.2011.0011. PMID: 21809914. PMCID: PMC6916526.
Article156. Robenshtok E, Fish S, Bach A, Dominguez JM, Shaha A, Tuttle RM. 2012; Suspicious cervical lymph nodes detected after thyroidectomy for papillary thyroid cancer usually remain stable over years in properly selected patients. J Clin Endocrinol Metab. 97(8):2706–13. DOI: 10.1210/jc.2012-1553. PMID: 22639292.
Article157. Chung SR, Baek JH, Choi YJ, Sung TY, Song DE, Kim TY, et al. 2021; Diagnostic algorithm for metastatic lymph nodes of differentiated thyroid carcinoma. Cancers (Basel). 13(6):1338. DOI: 10.3390/cancers13061338. PMID: 33809585. PMCID: PMC8000218.
Article158. Moon JH, Kim YI, Lim JA, Choi HS, Cho SW, Kim KW, et al. 2013; Thyroglobulin in washout fluid from lymph node fine- needle aspiration biopsy in papillary thyroid cancer: large-scale validation of the cutoff value to determine malignancy and evaluation of discrepant results. J Clin Endocrinol Metab. 98(3):1061–8. DOI: 10.1210/jc.2012-3291. PMID: 23393171.159. Kim MJ, Kim EK, Kim BM, Kwak JY, Lee EJ, Park CS, et al. 2009; Thyroglobulin measurement in fine-needle aspirate washouts: the criteria for neck node dissection for patients with thyroid cancer. Clin Endocrinol (Oxf). 70(1):145–51. DOI: 10.1111/j.1365-2265.2008.03297.x. PMID: 18466347.
Article160. Xu Y, Wu D, Wu W, Jiang J, Xi C, Ye N, et al. 2019; Diagnostic value of cytology, thyroglobulin, and combination of them in fine-needle aspiration of metastatic lymph nodes in patients with differentiated thyroid cancer: a systematic review and network meta-analysis. Medicine (Baltimore). 98(45):e17859. DOI: 10.1097/MD.0000000000017859. PMID: 31702649. PMCID: PMC6855606.161. Sun J, Li P, Chen X, Yu Q, Li L. 2022; The influence of thyroid status, serum Tg, TSH, and TgAb on FNA-Tg in cervical metastatic lymph nodes of papillary thyroid carcinoma. Laryngoscope Investig Otolaryngol. 7(1):274–82. DOI: 10.1002/lio2.717. PMID: 35155808. PMCID: PMC8823256.162. Boi F, Baghino G, Atzeni F, Lai ML, Faa G, Mariotti S. 2006; The diagnostic value for differentiated thyroid carcinoma metastases of thyroglobulin (Tg) measurement in washout fluid from fine-needle aspiration biopsy of neck lymph nodes is maintained in the presence of circulating anti-Tg antibodies. J Clin Endocrinol Metab. 91(4):1364–9. DOI: 10.1210/jc.2005-1705. PMID: 16434461.
Article163. Duval M, Zanella AB, Cristo AP, Faccin CS, Graudenz MS, Maia AL. 2017; Impact of serum TSH and anti-thyroglobulin antibody levels on lymph node fine-needle aspiration thyroglobulin measurements in differentiated thyroid cancer patients. Eur Thyroid J. 6(6):292–7. DOI: 10.1159/000479682. PMID: 29234622. PMCID: PMC5704678.
Article164. Snozek CL, Chambers EP, Reading CC, Sebo TJ, Sistrunk JW, Singh RJ, et al. 2007; Serum thyroglobulin, high-resolution ultrasound, and lymph node thyroglobulin in diagnosis of differentiated thyroid carcinoma nodal metastases. J Clin Endocrinol Metab. 92(11):4278–81. DOI: 10.1210/jc.2007-1075. PMID: 17684045.
Article165. Uruno T, Miyauchi A, Shimizu K, Tomoda C, Takamura Y, Ito Y, et al. 2005; Usefulness of thyroglobulin measurement in fine-needle aspiration biopsy specimens for diagnosing cervical lymph node metastasis in patients with papillary thyroid cancer. World J Surg. 29(4):483–5. DOI: 10.1007/s00268-004-7701-0. PMID: 15776292.
Article166. Sigstad E, Heilo A, Paus E, Holgersen K, Groholt KK, Jorgensen LH, et al. 2007; The usefulness of detecting thyroglobulin in fine-needle aspirates from patients with neck lesions using a sensitive thyroglobulin assay. Diagn Cytopathol. 35(12):761–7. DOI: 10.1002/dc.20726. PMID: 18008339.
Article167. Grani G, Fumarola A. 2014; Thyroglobulin in lymph node fine-needle aspiration washout: a systematic review and meta-analysis of diagnostic accuracy. J Clin Endocrinol Metab. 99(6):1970–82. DOI: 10.1210/jc.2014-1098. PMID: 24617715.
Article168. Torres MR, Nobrega Neto SH, Rosas RJ, Martins AL, Ramos AL, da Cruz TR. 2014; Thyroglobulin in the washout fluid of lymph-node biopsy: what is its role in the follow-up of differentiated thyroid carcinoma? Thyroid. 24(1):7–18. DOI: 10.1089/thy.2013.0244. PMID: 24044517.
Article169. Baloch ZW, Barroeta JE, Walsh J, Gupta PK, Livolsi VA, Langer JE, et al. 2008; Utility of thyroglobulin measurement in fine-needle aspiration biopsy specimens of lymph nodes in the diagnosis of recurrent thyroid carcinoma. Cytojournal. 5:1. DOI: 10.1186/1742-6413-5-1. PMID: 18237420. PMCID: PMC2276229.
Article170. Borel AL, Boizel R, Faure P, Barbe G, Boutonnat J, Sturm N, et al. 2008; Significance of low levels of thyroglobulin in fine needle aspirates from cervical lymph nodes of patients with a history of differentiated thyroid cancer. Eur J Endocrinol. 158(5):691–8. DOI: 10.1530/EJE-07-0749. PMID: 18426828.
Article171. Baldini E, Sorrenti S, Di Gioia C, De Vito C, Antonelli A, Gnessi L, et al. 2013; Cervical lymph node metastases from thyroid cancer: does thyroglobulin and calcitonin measurement in fine needle aspirates improve the diagnostic value of cytology? BMC Clin Pathol. 13:7. DOI: 10.1186/1472-6890-13-7. PMID: 23421519. PMCID: PMC3583740.
Article172. Park JY, Choi W, Hong AR, Yoon JH, Kim HK, Kang HC. 2023; A comprehensive assessment of the harms of fine-needle aspiration biopsy for thyroid nodules: a systematic review. Endocrinol Metab (Seoul). 38(1):104–16. DOI: 10.3803/EnM.2023.1669. PMID: 36891657. PMCID: PMC10008658.
Article173. Schleder S, Jung EM, Schicho A, Schreyer AG, Habicher W, Grassinger J, et al. 2023; Efficacy and safety of ultrasound-guided core needle biopsies (US-CNBs) in cervical lymphadenopathy in patients with suspected head and neck cancer during the COVID-19 pandemic. Clin Hemorheol Microcirc. 83(4):397–408. DOI: 10.3233/CH-221680. PMID: 36683499.
Article174. Assaf N, Nassif S, Tamim H, Bazarbachi A, Zaatari G, Chakhachiro Z. 2020; Diagnosing lymphoproliferative disorders using core needle biopsy versus surgical excisional biopsy: three-year experience of a reference center in Lebanon. Clin Lymphoma Myeloma Leuk. 20(8):e455–e60. DOI: 10.1016/j.clml.2019.11.013. PMID: 32461041.
Article175. Allin D, David S, Jacob A, Mir N, Giles A, Gibbins N. 2017; Use of core biopsy in diagnosing cervical lymphadenopathy: a viable alternative to surgical excisional biopsy of lymph nodes? Ann R Coll Surg Engl. 99(3):242–4. DOI: 10.1308/rcsann.2016.0353. PMID: 27917669. PMCID: PMC5450284.
Article176. Teng D, Dong C, Sun D, Liu Z, Wang H. 2021; Comparison of ultrasound-guided core needle biopsy under the assistance of hydrodissection with fine needle aspiration in the diagnosis of high-risk cervical lymph nodes: a randomized controlled trial. Front Oncol. 11:799956. DOI: 10.3389/fonc.2021.799956. PMID: 35096601. PMCID: PMC8793772.
Article177. Jeong SY, Baek JH, Chung SR, Choi YJ, Song DE, Chung KW, et al. 2022; Diagnostic performance of core needle biopsy for characterizing thyroidectomy bed lesions. Korean J Radiol. 23(10):1019–27. DOI: 10.3348/kjr.2021.0772. PMID: 36098339. PMCID: PMC9523230.
Article178. Lee MK, Baek JH, Chung SR, Choi YJ, Lee JH, Jung SL. 2022; Radiofrequency ablation of recurrent thyroid cancers: anatomy- based management. Ultrasonography. 41(3):434–43. DOI: 10.14366/usg.21221. PMID: 35189056. PMCID: PMC9262676.
Article179. Lee JY, Kim JH, Yeon EK, Hwang I, Yoo RE, Kang KM, et al. 2022; Computed tomography complements ultrasound for the differential diagnosis of traumatic neuroma from recurrent tumor in patients with postoperative thyroid cancer. Eur Radiol. 32(4):2760–8. DOI: 10.1007/s00330-021-08321-x. PMID: 34665316.
Article180. Wang JC, Takashima S, Takayama F, Kawakami S, Saito A, Matsushita T, et al. 2001; Tracheal invasion by thyroid carcinoma: prediction using MR imaging. AJR Am J Roentgenol. 177(4):929–36. DOI: 10.2214/ajr.177.4.1770929. PMID: 11566708.181. Pacini F, Capezzone M, Elisei R, Ceccarelli C, Taddei D, Pinchera A. 2002; Diagnostic 131-iodine whole-body scan may be avoided in thyroid cancer patients who have undetectable stimulated serum Tg levels after initial treatment. J Clin Endocrinol Metab. 87(4):1499–501. DOI: 10.1210/jcem.87.4.8274. PMID: 11932271.
Article182. Torlontano M, Crocetti U, D'Aloiso L, Bonfitto N, Di Giorgio A, Modoni S, et al. 2003; Serum thyroglobulin and 131I whole body scan after recombinant human TSH stimulation in the follow-up of low-risk patients with differentiated thyroid cancer. Eur J Endocrinol. 148(1):19–24. DOI: 10.1530/eje.0.1480019. PMID: 12534353.
Article183. Xue YL, Qiu ZL, Song HJ, Luo QY. 2013; Value of 131I SPECT/CT for the evaluation of differentiated thyroid cancer: a systematic review of the literature. Eur J Nucl Med Mol Imaging. 40(5):768–78. DOI: 10.1007/s00259-012-2310-x. PMID: 23242250.
Article184. Chong A, Seo Y, Bang JI, Park S, Kim K, Hong CM, et al. 2024; Clinical implications of adding SPECT/CT to radioiodine whole-body scan in patients with differentiated thyroid cancer: a systematic review and meta-analysis. Clin Nucl Med. 49(3):215–25. DOI: 10.1097/RLU.0000000000004953. PMID: 38048517.
Article185. Sahin M, Aydogan BI, Ozkan E, Emral R, Gullu S, Erdogan MF, et al. 2021; Recombinant human thyrotropin versus thyroid hormone withdrawal in differentiated thyroid carcinoma follow-up: a single center experience. Acta Endocrinol (Buchar). 17(3):337–45. DOI: 10.4183/aeb.2021.337. PMID: 35342477. PMCID: PMC8919477.
Article186. Liepe K. 2015; Sensitivity of preparation with rhTSH or thyroid hormone withdrawal using 131I-whole body scans to identify metastases of differentiated thyroid cancer. Int J Surg. 16(Pt A):107–12. DOI: 10.1016/j.ijsu.2015.02.016. PMID: 25771100.187. Qichang W, Lin B, Gege Z, Youjia Z, Qingjie M, Renjie W, et al. 2019; Diagnostic performance of 18F-FDG-PET/CT in DTC patients with thyroglobulin elevation and negative iodine scintigraphy: a meta-analysis. Eur J Endocrinol. 181(2):93–102. DOI: 10.1530/EJE-19-0261. PMID: 31117054.
Article188. Dong MJ, Liu ZF, Zhao K, Ruan LX, Wang GL, Yang SY, et al. 2009; Value of 18F-FDG-PET/PET-CT in differentiated thyroid carcinoma with radioiodine-negative whole-body scan: a meta-analysis. Nucl Med Commun. 30(8):639–50. DOI: 10.1097/MNM.0b013e32832dcfa7. PMID: 19512954.
Article189. Caetano R, Bastos CR, de Oliveira IA, da Silva RM, Fortes CP, Pepe VL, et al. 2016; Accuracy of positron emission tomography and positron emission tomography-CT in the detection of differentiated thyroid cancer recurrence with negative (131) I whole-body scan results: a meta-analysis. Head Neck. 38(2):316–27. DOI: 10.1002/hed.23881. PMID: 25251544.
Article190. Treglia G, Annunziata S, Muoio B, Salvatori M, Ceriani L, Giovanella L. 2013; The role of fluorine-18-fluorodeoxyglucose positron emission tomography in aggressive histological subtypes of thyroid cancer: an overview. Int J Endocrinol. 2013:856189. DOI: 10.1155/2013/856189. PMID: 23653645. PMCID: PMC3638656.
Article191. Zampella E, Klain M, Pace L, Cuocolo A. 2021; PET/CT in the management of differentiated thyroid cancer. Diagn Interv Imaging. 102(9):515–23. DOI: 10.1016/j.diii.2021.04.004. PMID: 33926848.
Article192. Cracolici V. 2023; No longer well-differentiated: diagnostic criteria and clinical importance of poorly differentiated/high-grade thyroid carcinoma. Surg Pathol Clin. 16(1):45–56. DOI: 10.1016/j.path.2022.09.006. PMID: 36739166.193. Ma C, Xie J, Lou Y, Gao Y, Zuo S, Wang X. 2010; The role of TSH for 18F-FDG-PET in the diagnosis of recurrence and metastases of differentiated thyroid carcinoma with elevated thyroglobulin and negative scan: a meta-analysis. Eur J Endocrinol. 163(2):177–83. DOI: 10.1530/EJE-10-0256. PMID: 20484385.
Article194. Bang JI, Park S, Kim K, Seo Y, Chong A, Hong CM, et al. 2023; The diagnostic value of (18)F-fluorodeoxyglucose positron emission tomography/computed tomography in differentiated thyroid cancer patients with elevated thyroglobulin/thyroglobulin antibody levels and negative iodine scintigraphy: a systematic review and meta-analysis. Thyroid. 33(10):1224–36. DOI: 10.1089/thy.2023.0264. PMID: 37597200.195. Bannas P, Derlin T, Groth M, Apostolova I, Adam G, Mester J, et al. 2012; Can (18)F-FDG-PET/CT be generally recommended in patients with differentiated thyroid carcinoma and elevated thyroglobulin levels but negative I-131 whole body scan? Ann Nucl Med. 26(1):77–85. DOI: 10.1007/s12149-011-0545-4. PMID: 22006540.
Article196. Choi SJ, Jung KP, Lee SS, Park YS, Lee SM, Bae SK. 2016; Clinical usefulness of F-18 FDG PET/CT in papillary thyroid cancer with negative radioiodine scan and elevated thyroglobulin level or positive anti-thyroglobulin antibody. Nucl Med Mol Imaging. 50(2):130–6. DOI: 10.1007/s13139-015-0378-5. PMID: 27275361. PMCID: PMC4870461.
Article197. Ozdemir E, Yildirim Poyraz N, Polat SB, Turkolmez S, Ersoy R, Cakir B. 2014; Diagnostic value of 18F-FDG PET/CT in patients with TENIS syndrome: correlation with thyroglobulin levels. Ann Nucl Med. 28(3):241–7. DOI: 10.1007/s12149-013-0801-x. PMID: 24379008.
Article198. Filippi L, Frantellizzi V, Monari F, Lodi Rizzini E, Tabacchi E, Pirisino R, et al. 2021; Usefulness of PET/CT with (18)F-FDG in patients with differentiated thyroid carcinoma after radioiodine therapy: an Italian multicenter study. Diagnostics (Basel). 11(7):1264. DOI: 10.3390/diagnostics11071264. PMID: 34359347. PMCID: PMC8306511.
Article199. Wang H, Fu HL, Li JN, Zhou RJ, Hui Gu Z, Wu JC, et al. 2008; Comparison of whole-body 18F-FDG SPECT and posttherapeutic 131I scintigraphy in the detection of metastatic thyroid cancer. Clin Imaging. 32(1):32–7. DOI: 10.1016/j.clinimag.2007.07.010. PMID: 18164392.
Article200. Kang SY, Bang JI, Kang KW, Lee HY, Chung JK. 2019; FDG PET/CT for the early prediction of RAI therapy response in patients with metastatic differentiated thyroid carcinoma. PLoS One. 14(6):e0218416. DOI: 10.1371/journal.pone.0218416. PMID: 31237886. PMCID: PMC6592523.
Article201. Wang H, Dai H, Li Q, Shen G, Shi L, Tian R. 2021; Investigating (18)F-FDG PET/CT parameters as prognostic markers for differentiated thyroid cancer: a systematic review. Front Oncol. 11:648658. DOI: 10.3389/fonc.2021.648658. PMID: 34055616. PMCID: PMC8158293.
Article202. Leboulleux S, El Bez I, Borget I, Elleuch M, Deandreis D, Al Ghuzlan A, et al. 2012; Postradioiodine treatment whole-body scan in the era of 18-fluorodeoxyglucose positron emission tomography for differentiated thyroid carcinoma with elevated serum thyroglobulin levels. Thyroid. 22(8):832–8. DOI: 10.1089/thy.2012.0081. PMID: 22853728.
Article203. Valerio L, Guidoccio F, Giani C, Tardelli E, Puccini G, Puleo L, et al. 2021; [18F]-FDG-PET/CT correlates with the response of radiorefractory thyroid cancer to lenvatinib and patient survival. J Clin Endocrinol Metab. 106(8):2355–66. DOI: 10.1210/clinem/dgab278. PMID: 33901285.
Article204. Grani G, Ramundo V, Falcone R, Lamartina L, Montesano T, Biffoni M, et al. 2019; Thyroid cancer patients with no evidence of disease: the need for repeat neck ultrasound. J Clin Endocrinol Metab. 104(11):4981–9. DOI: 10.1210/jc.2019-00962. PMID: 31206157.
Article205. Torlontano M, Attard M, Crocetti U, Tumino S, Bruno R, Costante G, et al. 2004; Follow-up of low risk patients with papillary thyroid cancer: role of neck ultrasonography in detecting lymph node metastases. J Clin Endocrinol Metab. 89(7):3402–7. DOI: 10.1210/jc.2003-031521. PMID: 15240622.
Article206. Matrone A, Gambale C, Piaggi P, Viola D, Giani C, Agate L, et al. 2017; Postoperative thyroglobulin and neck ultrasound in the risk restratification and decision to perform 131I ablation. J Clin Endocrinol Metab. 102(3):893–902. DOI: 10.1210/jc.2017-00617. PMID: 28482084.207. Malandrino P, Tumino D, Russo M, Marescalco S, Fulco RA, Frasca F. 2019; Surveillance of patients with differentiated thyroid cancer and indeterminate response: a longitudinal study on basal thyroglobulin trend. J Endocrinol Invest. 42(10):1223–30. DOI: 10.1007/s40618-019-01044-3. PMID: 30963467.
Article208. Tramontin MY, Nobre GM, Lopes M, Carneiro MP, Alves PAG, de Andrade FA, et al. 2021; High thyroglobulin and negative whole-body scan: no long-term benefit of empiric radioiodine therapy. Endocrine. 73(2):398–406. DOI: 10.1007/s12020-021-02647-8. PMID: 33570724.
Article209. Yuan L, Wang J, Pan L, Feng H, Chen P, Luo J, et al. 2023; Outcome of patients with differentiated thyroid cancer treated with empirical radioiodine therapy on the basis of Thyroglobulin Elevation Negative Iodine Scintigraphy (TENIS) syndrome without structural disease: a retrospective cohort study. Ann Nucl Med. 37(1):18–25. DOI: 10.1007/s12149-022-01799-5. PMID: 36318362.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- ATA Guideline in a View Point of Nuclear Medicine
- The Revised 2016 Korean Thyroid Association Guidelines for Thyroid Nodules and Cancers: Differences from the 2015 American Thyroid Association Guidelines
- Korean Thyroid Association Guidelines on the Management of Differentiated Thyroid Cancers; Part I. Initial Management of Differentiated Thyroid Cancers - Chapter 5. Evaluation of Recurrence Risk Postoperatively and Initial Risk Stratification in Differentiated Thyroid Cancer 2024
- Differentiated Thyroid Cancer and Radioactive Iodine: Past, Present and Future
- Postoperative Surveillance of Thyroid Cancer: in View of US