Int J Thyroidol.
2024 May;17(1):30-52. 10.11106/ijt.2024.17.1.30.
Korean Thyroid Association Guidelines on the Management of Differentiated Thyroid Cancers; Part I. Initial Management of Differentiated Thyroid Cancers - Chapter 2. Surgical Management of Thyroid Cancer 2024
- Affiliations
-
- 1Department of Internal Medicine, Soonchunhyang University Bucheon Hospital, Bucheon, Korea
- 2Department of Surgery, Yongin Severance Hospital, Yongin, Korea
- 3Department of Internal Medicine, Chonnam National University Hwasun Hospital, Hwasun, Korea
- 4Department of Otolaryngology-Head and Neck Surgery, Chungnam National University Hospital, Daejeon, Korea
- 5Department of Surgery, Ewha Womans University Mokdong Hospital, Seoul, Korea
- 6Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 7Department of Surgery, Asan Medical Center, Seoul, Korea
- 8Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 9Department of Radiology, Gangneung Asan Hospital, Gangneung, Korea
- 10Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 11Department of Surgery, Chung-Ang University Gwangmyeong Hospital, Gwangmyeong, Korea
- 12Department of Internal Medicine, Seoul National University Boramae Medical Center, Seoul, Korea
- 13Department of Otolaryngology-Head and Neck Surgery, Dankook University Hospital, Cheonan, Korea
- 14Department of Otolaryngology-Head and Neck Surgery, Chungnam National University Sejong Hospital, Sejong, Korea
- 15Department of Otolaryngology-Head and Neck Surgery, National Cancer Center, Goyang, Korea
- 16Department of Radiology, Yeouido St. Mary’s Hospital, Seoul, Korea
- 17Department of Internal Medicine, National Cancer Center, Goyang, Korea
- 18Department of Radiology, Seoul National University Hospital, Seoul, Korea
- 19Department of Internal Medicine, Seoul St. Mary’s Hospital, Seoul, Korea
- 20Department of Otolaryngology-Head and Neck Surgery, Gangnam Severance Hospital, Seoul, Korea
- 21Department of Internal Medicine, Chung-Ang University Hospital, Seoul, Korea
- 22Department of Pathology, Seoul St. Mary’s Hospital, Seoul, Korea
- 23Department of Otolaryngology-Head and Neck Surgery, Eunpyeong St. Mary’s Hospital, Seoul, Korea
- KMID: 2556504
- DOI: http://doi.org/10.11106/ijt.2024.17.1.30
Abstract
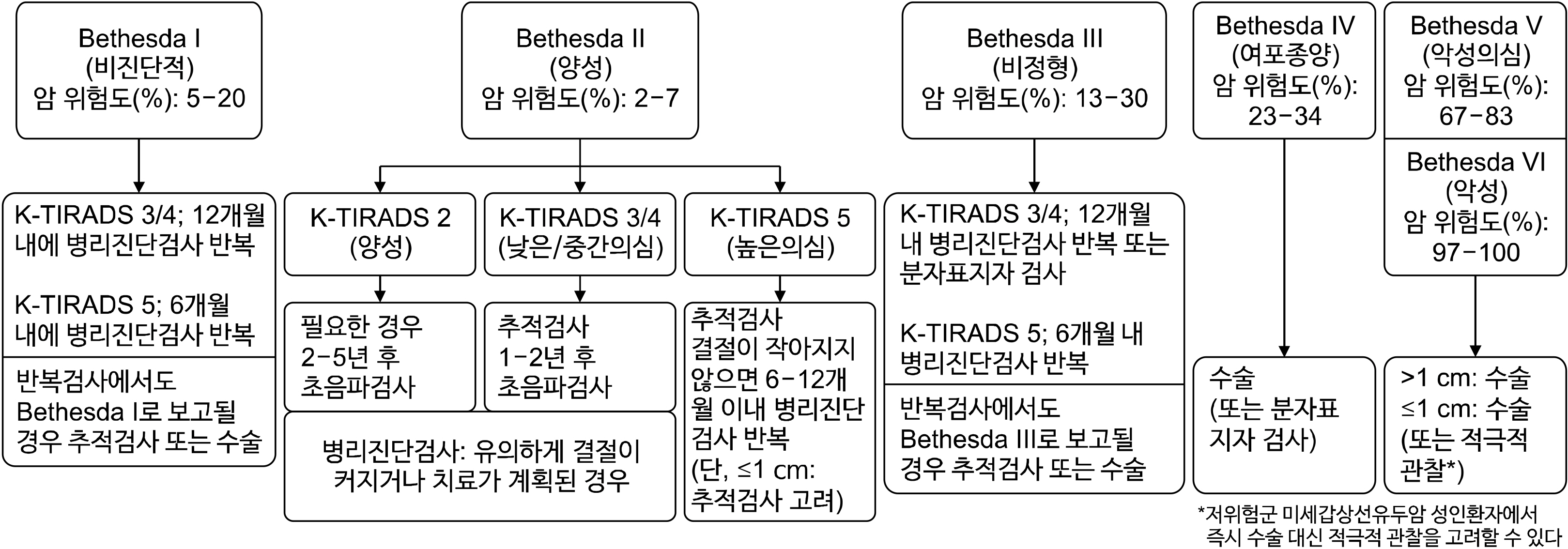
- The primary objective of initial treatment for thyroid cancer is minimizing treatment-related side effects and unnecessary interventions while improving patients’ overall and disease-specific survival rates, reducing the risk of disease persistence or recurrence, and conducting accurate staging and recurrence risk analysis. Appropriate surgical treatment is the most important requirement for this purpose, and additional treatments including radioactive iodine therapy and thyroid-stimulating hormone suppression therapy are performed depending on the patients’ staging and recurrence risk. Diagnostic surgery may be considered when repeated pathologic tests yield nondiagnostic results (Bethesda category 1) or atypia of unknown significance (Bethesda category 3), depending on clinical risk factors, nodule size, ultrasound findings, and patient preference. If a follicular neoplasm (Bethesda category 4) is diagnosed pathologically, surgery is the preferred option. For suspicious papillary carcinoma (suspicious for malignancy, Bethesda category 5), surgery is considered similar to a diagnosis of malignancy (Bethesda category 6). As for the extent of surgery, if the cancer is ≤1 cm in size and clinically free of extrathyroidal extension (ETE) (cT1a), without evidence of cervical lymph node (LN) metastasis (cN0), and without obvious reason to resect the contralateral lobe, a lobectomy can be performed. If the cancer is 1-2 cm in size, clinically free of ETE (cT1b), and without evidence of cervical LN metastasis (cN0), lobectomy is the preferred option. For patients with clinically evident ETE to major organs (cT4) or with cervical LN metastasis (cN1) or distant metastasis (M1), regardless of the cancer size, total thyroidectomy and complete cancer removal should be performed at the time of initial surgery. Active surveillance may be considered for adult patients diagnosed with low-risk thyroid papillary microcarcinoma. Endoscopic and robotic thyroidectomy may be performed for low-risk differentiated thyroid cancer when indicated, based on patient preference.
Figure
Reference
-
References
1. Huang H, Yan D, Liu W, Liu S, Xu Z, Wang X. 2022; Isthmectomy is effective and sufficient for selected patients with the isthmus-confined solitary papillary thyroid carcinoma. Asian J Surg. 45(9):1678–81. DOI: 10.1016/j.asjsur.2021.08.074. PMID: 35181211.
Article2. Park H, Harries V, McGill MR, Ganly I, Shah JP. 2020; Isthmusectomy in selected patients with well-differentiated thyroid carcinoma. Head Neck. 42(1):43–9. DOI: 10.1002/hed.25968. PMID: 31589005. PMCID: PMC7485011.
Article3. Ali SZ, Baloch ZW, Cochand-Priollet B, Schmitt FC, Vielh P, VanderLaan PA. 2023; The 2023 Bethesda system for reporting thyroid cytopathology. Thyroid. 33(9):1039–44. DOI: 10.1089/thy.2023.0141. PMID: 37427847.
Article4. Kim K, Bae JS, Kim JS, Jung SL, Jung CK. 2022; Diagnostic performance of thyroid core needle biopsy using the revised reporting system: comparison with fine needle aspiration cytology. Endocrinol Metab (Seoul). 37(1):159–69. DOI: 10.3803/EnM.2021.1299. PMID: 35255608. PMCID: PMC8901962.
Article5. Chung SR, Baek JH, Lee JH, Lee YM, Sung TY, Chung KW, et al. 2019; Risk of malignancy according to the sub- classification of atypia of undetermined significance and suspicious follicular neoplasm categories in thyroid core needle biopsies. Endocr Pathol. 30(2):146–54. DOI: 10.1007/s12022-019-9577-4. PMID: 31044350.
Article6. Na HY, Woo JW, Moon JH, Choi JY, Jeong WJ, Kim YK, et al. 2019; Preoperative diagnostic categories of noninvasive follicular thyroid neoplasm with papillary-like nuclear features in thyroid core needle biopsy and its impact on risk of malignancy. Endocr Pathol. 30(4):329–39. DOI: 10.1007/s12022-019-09590-5. PMID: 31605276.
Article7. Ali SZ, Baloch ZW, Cochand-Priollet B, Schmitt FC, Vielh P, VanderLaan PA. 2023; The 2023 Bethesda system for reporting thyroid cytopathology. J Am Soc Cytopathol. 12(5):319–25. DOI: 10.1016/j.jasc.2023.05.005. PMID: 37438235.
Article8. Jung CK, Baek JH, Na DG, Oh YL, Yi KH, Kang HC. 2020; 2019 practice guidelines for thyroid core needle biopsy: a report of the Clinical Practice Guidelines Development Committee of the Korean Thyroid Association. J Pathol Transl Med. 54(1):64–86. DOI: 10.4132/jptm.2019.12.04. PMID: 31964112. PMCID: PMC6986975.
Article9. Park JY, Yi SY, Baek SH, Lee YH, Kwon HJ, Park HJ. 2022; Diagnostic efficacy, performance and safety of side-cut core needle biopsy for thyroid nodules: comparison of automated and semi-automated biopsy needles. Endocrine. 76(2):341–8. DOI: 10.1007/s12020-022-02980-6. PMID: 35032314.
Article10. Ahn HS, Youn I, Na DG, Kim SJ, Lee MY. 2021; Diagnostic performance of core needle biopsy as a first-line diagnostic tool for thyroid nodules according to ultrasound patterns: comparison with fine needle aspiration using propensity score matching analysis. Clin Endocrinol (Oxf). 94(3):494–503. DOI: 10.1111/cen.14321. PMID: 32869866.
Article11. Xiong Y, Yan L, Nong L, Zheng Y, Li T. 2019; Pathological diagnosis of thyroid nodules based on core needle biopsies: comparative study between core needle biopsies and resected specimens in 578 cases. Diagn Pathol. 14(1):10. DOI: 10.1186/s13000-019-0786-4. PMID: 30711008. PMCID: PMC6359785.
Article12. Ahn HS, Seo M, Ha SM, Kim HS. 2018; Comparison of the diagnostic efficacy of ultrasound-guided core needle biopsy with 18- versus 20-gauge needles for thyroid nodules. J Ultrasound Med. 37(11):2565–74. DOI: 10.1002/jum.14614. PMID: 29575135.
Article13. Choe J, Baek JH, Park HS, Choi YJ, Lee JH. 2018; Core needle biopsy of thyroid nodules: outcomes and safety from a large single-center single-operator study. Acta Radiol. 59(8):924–31. DOI: 10.1177/0284185117741916. PMID: 29137498.
Article14. Hong MJ, Na DG, Kim SJ, Kim DS. 2018; Role of core needle biopsy as a first-line diagnostic tool for thyroid nodules: a retrospective cohort study. Ultrasonography. 37(3):244–53. DOI: 10.14366/usg.17041. PMID: 29113031. PMCID: PMC6044216.
Article15. Kim HC, Kim YJ, Han HY, Yi JM, Baek JH, Park SY, et al. 2017; First-line use of core needle biopsy for high-yield preliminary diagnosis of thyroid nodules. AJNR Am J Neuroradiol. 38(2):357–63. DOI: 10.3174/ajnr.A5007. PMID: 27932508. PMCID: PMC7963827.
Article16. Suh CH, Baek JH, Choi YJ, Kim TY, Sung TY, Song DE, et al. 2017; Efficacy and safety of core-needle biopsy in initially detected thyroid nodules via propensity score analysis. Sci Rep. 7(1):8242. DOI: 10.1038/s41598-017-07924-z. PMID: 28811482. PMCID: PMC5557918.
Article17. Suh CH, Baek JH, Lee JH, Choi YJ, Kim JK, Sung TY, et al. 2016; The role of core-needle biopsy as a first-line diagnostic tool for initially detected thyroid nodules. Thyroid. 26(3):395–403. DOI: 10.1089/thy.2015.0404. PMID: 26651390.
Article18. Kim YH, Kwon HJ, Kim EK, Kwak JY, Moon HJ, Yoon JH. 2015; Applying ultrasound-guided core needle biopsy for diagnosis of thyroid masses: preliminary results from a single institution. J Ultrasound Med. 34(10):1801–8. DOI: 10.7863/ultra.15.14.12028. PMID: 26324755.19. Ha EJ, Baek JH, Lee JH, Kim JK, Kim JK, Lim HK, et al. 2014; Core needle biopsy can minimise the non-diagnostic results and need for diagnostic surgery in patients with calcified thyroid nodules. Eur Radiol. 24(6):1403–9. DOI: 10.1007/s00330-014-3123-z. PMID: 24604217.
Article20. Ha EJ, Baek JH, Lee JH, Song DE, Kim JK, Shong YK, et al. 2013; Sonographically suspicious thyroid nodules with initially benign cytologic results: the role of a core needle biopsy. Thyroid. 23(6):703–8. DOI: 10.1089/thy.2012.0426. PMID: 23544697.
Article21. Sung JY, Na DG, Kim KS, Yoo H, Lee H, Kim JH, et al. 2012; Diagnostic accuracy of fine-needle aspiration versus core-needle biopsy for the diagnosis of thyroid malignancy in a clinical cohort. Eur Radiol. 22(7):1564–72. DOI: 10.1007/s00330-012-2405-6. PMID: 22415411.
Article22. Joo L, Na DG, Kim JH, Seo H. 2022; Comparison of core needle biopsy and repeat fine-needle aspiration in avoiding diagnostic surgery for thyroid nodules initially diagnosed as atypia/follicular lesion of undetermined significance. Korean J Radiol. 23(2):280–8. DOI: 10.3348/kjr.2021.0619. PMID: 35029081. PMCID: PMC8814697.
Article23. Choe JY, Kwak Y, Kim M, Chung YR, Kim HJ, Kim YK, et al. 2018; Utility of a formatted pathologic reporting system in thyroid core needle biopsy: a validation study of 1998 consecutive cases. Clin Endocrinol (Oxf). 88(1):96–104. DOI: 10.1111/cen.13397. PMID: 28618022.
Article24. Hauch A, Al-Qurayshi Z, Randolph G, Kandil E. 2014; Total thyroidectomy is associated with increased risk of complications for low- and high-volume surgeons. Ann Surg Oncol. 21(12):3844–52. DOI: 10.1245/s10434-014-3846-8. PMID: 24943236.
Article25. Park I, Rhu J, Woo JW, Choi JH, Kim JS, Kim JH. 2016; Preserving parathyroid gland vasculature to reduce post- thyroidectomy hypocalcemia. World J Surg. 40(6):1382–9. DOI: 10.1007/s00268-016-3423-3. PMID: 27028753.26. Park S, Jeon MJ, Song E, Oh HS, Kim M, Kwon H, et al. 2017; Clinical features of early and late postoperative hypothyroidism after lobectomy. J Clin Endocrinol Metab. 102(4):1317–24. DOI: 10.1210/jc.2016-3597. PMID: 28324106.
Article27. Vuong HG, Chung DGB, Ngo LM, Bui TQ, Hassell L, Jung CK, et al. 2021; The use of the Bethesda system for reporting thyroid cytopathology in pediatric thyroid nodules: a meta- analysis. Thyroid. 31(8):1203–11. DOI: 10.1089/thy.2020.0702. PMID: 33504264.28. Lee YB, Oh YL, Shin JH, Kim SW, Chung JH, Min YK, et al. 2021; Comparison of four ultrasonography-based risk stratification systems in thyroid nodules with nondiagnostic/unsatisfactory cytology: a real-world study. Cancers (Basel). 13(8):1948. DOI: 10.3390/cancers13081948. PMID: 33919595. PMCID: PMC8073392.
Article29. Hong MJ, Na DG, Baek JH, Sung JY, Kim JH. 2017; Cytology-ultrasonography risk-stratification scoring system based on fine-needle aspiration cytology and the Korean-Thyroid Imaging Reporting and Data System. Thyroid. 27(7):953–9. DOI: 10.1089/thy.2016.0603. PMID: 28463597.
Article30. Vuong HG, Ngo HTT, Bychkov A, Jung CK, Vu TH, Lu KB, et al. 2020; Differences in surgical resection rate and risk of malignancy in thyroid cytopathology practice between Western and Asian countries: a systematic review and meta-analysis. Cancer Cytopathol. 128(4):238–49. DOI: 10.1002/cncy.22228. PMID: 31883438.
Article31. Ngo HTT, Nguyen TPX, Vu TH, Jung CK, Hassell L, Kakudo K, et al. 2021; Impact of molecular testing on the management of indeterminate thyroid nodules among Western and Asian countries: a systematic review and meta-analysis. Endocr Pathol. 32(2):269–79. DOI: 10.1007/s12022-020-09643-0. PMID: 32767256.
Article32. Słowińska-Klencka D, Wysocka-Konieczna K, Klencki M, Popowicz B. 2020; Diagnostic value of six Thyroid Imaging Reporting and Data Systems (TIRADS) in cytologically equivocal thyroid nodules. J Clin Med. 9(7):2281. DOI: 10.3390/jcm9072281. PMID: 32709122. PMCID: PMC7408998.
Article33. Hong HS, Lee JY. 2019; Diagnostic performance of ultrasound patterns by K-TIRADS and 2015 ATA guidelines in risk stratification of thyroid nodules and follicular lesions of undetermined significance. AJR Am J Roentgenol. 213(2):444–50. DOI: 10.2214/AJR.18.20961. PMID: 31039023.
Article34. Nikiforov YE, Seethala RR, Tallini G, Baloch ZW, Basolo F, Thompson LD, et al. 2016; Nomenclature revision for encapsulated follicular variant of papillary thyroid carcinoma: a paradigm shift to reduce overtreatment of indolent tumors. JAMA Oncol. 2(8):1023–9. DOI: 10.1001/jamaoncol.2016.0386. PMID: 27078145. PMCID: PMC5539411.
Article35. Cho YY, Ahn SH, Lee EK, Park YJ, Choi D, Kim BY, et al. 2024; Malignancy risk of follicular neoplasm (Bethesda IV) with variable cutoffs of tumor size: a systemic review and meta-analysis. J Clin Endocrinol Metab. 109(5):1383–92. DOI: 10.1210/clinem/dgad684. PMID: 38113188.
Article36. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2016; 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 26(1):1–133. DOI: 10.1089/thy.2015.0020. PMID: 26462967. PMCID: PMC4739132.
Article37. Durante C, Hegedus L, Czarniecka A, Paschke R, Russ G, Schmitt F, et al. 2023; 2023 European Thyroid Association clinical practice guidelines for thyroid nodule management. Eur Thyroid J. 12(5):e230067. DOI: 10.1530/ETJ-23-0067.
Article38. Agarwal S, Bychkov A, Jung CK. 2021; Emerging biomarkers in thyroid practice and research. Cancers (Basel). 14(1):204. DOI: 10.3390/cancers14010204. PMID: 35008368. PMCID: PMC8744846.
Article39. Lasolle H, Lopez J, Pattou F, Borson-Chazot F, Bardet S, Groussin L, et al. 2022; SFE-AFCE-SFMN 2022 consensus on the management of thyroid nodules : role of molecular tests for cytologically indeterminate thyroid nodules. Ann Endocrinol (Paris). 83(6):395–400. DOI: 10.1016/j.ando.2022.10.006. PMID: 36283464.
Article40. Trimboli P, Ferrarazzo G, Piccardo A, Lucchini B, Durante C. 2022; Operation rate and cancer prevalence among thyroid nodules with FNAC report of suspicious for malignancy (TIR4) or malignant (TIR5) according to Italian classification system: a systematic review and meta-analysis. Endocrine. 78(1):24–31. DOI: 10.1007/s12020-022-03165-x. PMID: 35986840. PMCID: PMC9474526.
Article41. Chen B, Shi Y, Xu Y, Zhang J. 2021; The predictive value of coexisting BRAFV600E and TERT promoter mutations on poor outcomes and high tumour aggressiveness in papillary thyroid carcinoma: a systematic review and meta-analysis. Clin Endocrinol (Oxf). 94(5):731–42. DOI: 10.1111/cen.14316. PMID: 32816325.
Article42. Moon S, Song YS, Kim YA, Lim JA, Cho SW, Moon JH, et al. 2017; Effects of coexistent BRAF(V600E) and TERT promoter mutations on poor clinical outcomes in papillary thyroid cancer: a meta-analysis. Thyroid. 27(5):651–60. DOI: 10.1089/thy.2016.0350. PMID: 28181854.
Article43. Zhang C, Li Y, Li J, Chen X. 2020; Total thyroidectomy versus lobectomy for papillary thyroid cancer: a systematic review and meta-analysis. Medicine (Baltimore). 99(6):e19073. DOI: 10.1097/MD.0000000000019073. PMID: 32028431. PMCID: PMC7015547.44. Macedo FI, Mittal VK. 2015; Total thyroidectomy versus lobectomy as initial operation for small unilateral papillary thyroid carcinoma: a meta-analysis. Surg Oncol. 24(2):117–22. DOI: 10.1016/j.suronc.2015.04.005. PMID: 25956302.
Article45. Bilimoria KY, Bentrem DJ, Ko CY, Stewart AK, Winchester DP, Talamonti MS, et al. 2007; Extent of surgery affects survival for papillary thyroid cancer. Ann Surg. 246(3):375–81. discussion 81–4. DOI: 10.1097/SLA.0b013e31814697d9. PMID: 17717441. PMCID: PMC1959355.
Article46. Rajjoub SR, Yan H, Calcatera NA, Kuchta K, Wang CE, Lutfi W, et al. 2018; Thyroid lobectomy is not sufficient for T2 papillary thyroid cancers. Surgery. 163(5):1134–43. DOI: 10.1016/j.surg.2017.12.026. PMID: 29426618.
Article47. Suman P, Razdan SN, Wang CE, Tulchinsky M, Ahmed L, Prinz RA, et al. 2020; Thyroid lobectomy for T1b-T2 papillary thyroid cancer with high-risk features. J Am Coll Surg. 230(1):136–44. DOI: 10.1016/j.jamcollsurg.2019.09.021. PMID: 31672668.
Article48. Nixon IJ, Wang LY, Migliacci JC, Eskander A, Campbell MJ, Aniss A, et al. 2016; An international multi-institutional validation of age 55 years as a cutoff for risk stratification in the AJCC/UICC staging system for well-differentiated thyroid cancer. Thyroid. 26(3):373–80. DOI: 10.1089/thy.2015.0315. PMID: 26914539. PMCID: PMC4790212.
Article49. Capezzone M, Robenshtok E, Cantara S, Castagna MG. 2021; Familial non-medullary thyroid cancer: a critical review. J Endocrinol Invest. 44(5):943–50. DOI: 10.1007/s40618-020-01435-x. PMID: 33025555. PMCID: PMC8049908.
Article50. Saenko V, Mitsutake N. 2024; Radiation-related thyroid cancer. Endocr Rev. 45(1):1–29. DOI: 10.1210/endrev/bnad022. PMID: 37450579. PMCID: PMC10765163.
Article51. Adam MA, Pura J, Gu L, Dinan MA, Tyler DS, Reed SD, et al. 2014; Extent of surgery for papillary thyroid cancer is not associated with survival: an analysis of 61,775 patients. Ann Surg. 260(4):601–5. discussion 5–7. DOI: 10.1097/SLA.0000000000000925. PMID: 25203876. PMCID: PMC4532384.52. Tuttle RM, Haugen B, Perrier ND. 2017; Updated American Joint Committee on cancer/tumor-node-metastasis staging system for differentiated and anaplastic thyroid cancer (eighth edition): what changed and why? Thyroid. 27(6):751–6. DOI: 10.1089/thy.2017.0102. PMID: 28463585. PMCID: PMC5467103.
Article53. Kim TH, Kim YN, Kim HI, Park SY, Choe JH, Kim JH, et al. 2017; Prognostic value of the eighth edition AJCC TNM classification for differentiated thyroid carcinoma. Oral Oncol. 71:81–6. DOI: 10.1016/j.oraloncology.2017.06.004. PMID: 28688696.
Article54. Tam S, Boonsripitayanon M, Amit M, Fellman BM, Li Y, Busaidy NL, et al. 2018; Survival in differentiated thyroid cancer: comparing the AJCC cancer staging seventh and eighth editions. Thyroid. 28(10):1301–10. DOI: 10.1089/thy.2017.0572. PMID: 30141373.
Article55. Xiang J, Wang Z, Sun W, Zhang H. 2021; The new T3b category has clinical significance? SEER-based study. Clin Endocrinol (Oxf). 94(3):449–59. DOI: 10.1111/cen.14305. PMID: 32745252.
Article56. Park SY, Kim HI, Kim JH, Kim JS, Oh YL, Kim SW, et al. 2018; Prognostic significance of gross extrathyroidal extension invading only strap muscles in differentiated thyroid carcinoma. Br J Surg. 105(9):1155–62. DOI: 10.1002/bjs.10830. PMID: 29663333.
Article57. Song E, Lee YM, Oh HS, Jeon MJ, Song DE, Kim TY, et al. 2019; A relook at the T stage of differentiated thyroid carcinoma with a focus on gross extrathyroidal extension. Thyroid. 29(2):202–8. DOI: 10.1089/thy.2018.0300. PMID: 30358515.
Article58. Park JO, Kim JH, Joo YH, Kim SY, Kim GJ, Kim HB, et al. 2023; Guideline for the surgical management of locally invasive differentiated thyroid cancer from the Korean Society of Head and Neck Surgery. Clin Exp Otorhinolaryngol. 16(1):1–19. DOI: 10.21053/ceo.2022.01732. PMID: 36634669. PMCID: PMC9985989.
Article59. Lee DY, Oh DJ, Kang KR, Kim MS, Oh KH, Baek SK, et al. 2016; Comparison of learning curves for retroauricular and transaxillary endoscopic hemithyroidectomy. Ann Surg Oncol. 23(12):4023–8. DOI: 10.1245/s10434-016-5433-7. PMID: 27421697.
Article60. Lee J, Yun JH, Nam KH, Soh EY, Chung WY. 2011; The learning curve for robotic thyroidectomy: a multicenter study. Ann Surg Oncol. 18(1):226–32. DOI: 10.1245/s10434-010-1220-z. PMID: 20680695.
Article61. Adam MA, Thomas S, Youngwirth L, Hyslop T, Reed SD, Scheri RP, et al. 2017; Is there a minimum number of thyroidectomies a surgeon should perform to optimize patient outcomes? Ann Surg. 265(2):402–7. DOI: 10.1097/SLA.0000000000001688. PMID: 28059969.
Article62. Ito Y, Miyauchi A, Inoue H, Fukushima M, Kihara M, Higashiyama T, et al. 2010; An observational trial for papillary thyroid microcarcinoma in Japanese patients. World J Surg. 34(1):28–35. DOI: 10.1007/s00268-009-0303-0. PMID: 20020290.
Article63. Molinaro E, Campopiano MC, Pieruzzi L, Matrone A, Agate L, Bottici V, et al. 2020; Active surveillance in papillary thyroid microcarcinomas is feasible and safe: experience at a single Italian center. J Clin Endocrinol Metab. 105(3):e172–80. DOI: 10.1210/clinem/dgz113. PMID: 31652318. PMCID: PMC8105780.
Article64. Sanabria A. 2020; Experience with active surveillance of thyroid low-risk carcinoma in a developing country. Thyroid. 30(7):985–91. DOI: 10.1089/thy.2019.0522. PMID: 31950887.
Article65. Jin M, Kim HI, Ha J, Jeon MJ, Kim WG, Lim DJ, et al. 2021; Tumor volume doubling time in active surveillance of papillary thyroid microcarcinoma: a multicenter cohort study in Korea. Thyroid. 31(10):1494–501. DOI: 10.1089/thy.2021.0094. PMID: 34225475.
Article66. Nagaoka R, Ebina A, Toda K, Jikuzono T, Saitou M, Sen M, et al. 2021; Multifocality and progression of papillary thyroid microcarcinoma during active surveillance. World J Surg. 45(9):2769–76. DOI: 10.1007/s00268-021-06185-2. PMID: 34100116.
Article67. Ho AS, Kim S, Zalt C, Melany ML, Chen IE, Vasquez J, et al. 2022; Expanded parameters in active surveillance for low-risk papillary thyroid carcinoma: a nonrandomized controlled trial. JAMA Oncol. 8(11):1588–96. DOI: 10.1001/jamaoncol.2022.3875. PMID: 36107411. PMCID: PMC9478884.
Article68. Lee EK, Moon JH, Hwangbo Y, Ryu CH, Cho SW, Choi JY, et al. 2022; Progression of low-risk papillary thyroid microcarcinoma during active surveillance: interim analysis of a multicenter prospective cohort study of active surveillance on papillary thyroid microcarcinoma in Korea. Thyroid. 32(11):1328–36. DOI: 10.1089/thy.2021.0614. PMID: 36205563. PMCID: PMC9700369.
Article69. Ito Y, Miyauchi A, Fujishima M, Noda T, Sano T, Sasaki T, et al. 2023; Thyroid-stimulating hormone, age, and tumor size are risk factors for progression during active surveillance of low-risk papillary thyroid microcarcinoma in adults. World J Surg. 47(2):392–401. DOI: 10.1007/s00268-022-06770-z. PMID: 36182976. PMCID: PMC9803751.
Article70. Miyauchi A, Ito Y, Fujishima M, Miya A, Onoda N, Kihara M, et al. 2023; Long-term outcomes of active surveillance and immediate surgery for adult patients with low-risk papillary thyroid microcarcinoma: 30-year experience. Thyroid. 33(7):817–25. DOI: 10.1089/thy.2023.0076. PMID: 37166389. PMCID: PMC10354707.
Article71. Tuttle RM, Fagin J, Minkowitz G, Wong R, Roman B, Patel S, et al. 2022; Active surveillance of papillary thyroid cancer: frequency and time course of the six most common tumor volume kinetic patterns. Thyroid. 32(11):1337–45. DOI: 10.1089/thy.2022.0325. PMID: 36178355. PMCID: PMC9700377.
Article72. Oh HS, Kwon H, Song E, Jeon MJ, Kim TY, Lee JH, et al. 2019; Tumor volume doubling time in active surveillance of papillary thyroid carcinoma. Thyroid. 29(5):642–9. DOI: 10.1089/thy.2018.0609. PMID: 30864894.
Article73. Lee JY, Kim JH, Kim YK, Lee CY, Lee EK, Moon JH, et al. 2023; US predictors of papillary thyroid microcarcinoma progression at active surveillance. Radiology. 309(1):e230006. DOI: 10.1148/radiol.230006. PMID: 37906009.
Article74. Ito Y, Miyauchi A, Kihara M, Higashiyama T, Kobayashi K, Miya A. 2014; Patient age is significantly related to the progression of papillary microcarcinoma of the thyroid under observation. Thyroid. 24(1):27–34. DOI: 10.1089/thy.2013.0367. PMID: 24001104. PMCID: PMC3887422.
Article75. Mazzaferri EL. 2011; Approach to the pregnant patient with thyroid cancer. J Clin Endocrinol Metab. 96(2):265–72. DOI: 10.1210/jc.2010-1624. PMID: 21296990.
Article76. Oh HS, Kim WG, Park S, Kim M, Kwon H, Jeon MJ, et al. 2017; Serial neck ultrasonographic evaluation of changes in papillary thyroid carcinoma during pregnancy. Thyroid. 27(6):773–7. DOI: 10.1089/thy.2016.0618. PMID: 28446078.
Article77. Ito Y, Miyauchi A, Kudo T, Ota H, Yoshioka K, Oda H, et al. 2016; Effects of pregnancy on papillary microcarcinomas of the thyroid re-evaluated in the entire patient series at Kuma Hospital. Thyroid. 26(1):156–60. DOI: 10.1089/thy.2015.0393. PMID: 26670937. PMCID: PMC4739387.
Article78. Horiguchi K, Yoshida Y, Iwaku K, Emoto N, Kasahara T, Sato J, et al. 2021; Position paper from the Japan Thyroid Association task force on the management of low-risk papillary thyroid microcarcinoma (T1aN0M0) in adults. Endocr J. 68(7):763–80. DOI: 10.1507/endocrj.EJ20-0692. PMID: 33762511.
Article79. Hwang H, Choi JY, Yu HW, Moon JH, Kim JH, Lee EK, et al. 2023; Surgical outcomes in patients with low-risk papillary thyroid microcarcinoma from MAeSTro study: immediate operation versus delayed operation after active surveillance. A multicenter prospective cohort study. Ann Surg. 278(5):e1087–e95. DOI: 10.1097/SLA.0000000000005841. PMID: 36912439.80. Kim K, Choi JY, Kim SJ, Lee EK, Lee YK, Ryu JS, et al. 2022; Active surveillance versus immediate surgery for low-risk papillary thyroid microcarcinoma patients in South Korea: a cost-minimization analysis from the MAeSTro study. Thyroid. 32(6):648–56. DOI: 10.1089/thy.2021.0679. PMID: 35570657.
Article81. Baek HS, Ha J, Kim K, Bae J, Kim JS, Kim S, et al. 2023; Cost-effectiveness of active surveillance compared to early surgery of small papillary thyroid cancer: a retrospective study on a Korean population. J Korean Med Sci. 38(34):e264. DOI: 10.3346/jkms.2023.38.e264. PMID: 37644680. PMCID: PMC10462480.
Article82. Kong SH, Ryu J, Kim MJ, Cho SW, Song YS, Yi KH, et al. 2019; Longitudinal assessment of quality of life according to treatment options in low-risk papillary thyroid microcarcinoma patients: active surveillance or immediate surgery (interim analysis of MAeSTro). Thyroid. 29(8):1089–96. DOI: 10.1089/thy.2018.0624. PMID: 31161898.
Article83. Moon JH, Ryu CH, Cho SW, Choi JY, Chung EJ, Hah JH, et al. 2021; Effect of initial treatment choice on 2-year quality of life in patients with low-risk papillary thyroid microcarcinoma. J Clin Endocrinol Metab. 106(3):724–35. DOI: 10.1210/clinem/dgaa889. PMID: 33248442.
Article84. Hwangbo Y, Choi JY, Lee EK, Ryu CH, Cho SW, Chung EJ, et al. 2022; A cross-sectional survey of patient treatment choice in a multicenter prospective cohort study on active surveillance of papillary thyroid microcarcinoma (MAeSTro). Thyroid. 32(7):772–80. DOI: 10.1089/thy.2021.0619. PMID: 35698288.
Article85. Brito JP, Moon JH, Zeuren R, Kong SH, Kim YG, Iniguez-Ariza NM, et al. 2018; Thyroid cancer treatment choice: a pilot study of a tool to facilitate conversations with patients with papillary microcarcinomas considering treatment options. Thyroid. 28(10):1325–31. DOI: 10.1089/thy.2018.0105. PMID: 29905089.
Article86. Issa PP, Mueller L, Hussein M, Albuck A, Shama M, Toraih E, et al. 2022; Radiologist versus non-radiologist detection of lymph node metastasis in papillary thyroid carcinoma by ultrasound: a meta-analysis. Biomedicines. 10(10):2575. DOI: 10.3390/biomedicines10102575. PMID: 36289838. PMCID: PMC9599420.
Article87. Suh CH, Baek JH, Choi YJ, Lee JH. 2017; Performance of CT in the preoperative diagnosis of cervical lymph node metastasis in patients with papillary thyroid cancer: a systematic review and meta-analysis. AJNR Am J Neuroradiol. 38(1):154–61. DOI: 10.3174/ajnr.A4967. PMID: 27789450. PMCID: PMC7963646.
Article88. Lee DH, Kim YK, Yu HW, Choi JY, Park SY, Moon JH. 2019; Computed tomography for detecting cervical lymph node metastasis in patients who have papillary thyroid microcarcinoma with tumor characteristics appropriate for active surveillance. Thyroid. 29(11):1653–9. DOI: 10.1089/thy.2019.0100. PMID: 31436140.
Article89. Xing Z, Qiu Y, Yang Q, Yu Y, Liu J, Fei Y, et al. 2020; Thyroid cancer neck lymph nodes metastasis: meta-analysis of US and CT diagnosis. Eur J Radiol. 129:109103. DOI: 10.1016/j.ejrad.2020.109103. PMID: 32574937.
Article90. Gronlund MP, Jensen JS, Hahn CH, Gronhoj C, Buchwald CV. 2021; Risk factors for recurrence of follicular thyroid cancer: a systematic review. Thyroid. 31(10):1523–30. DOI: 10.1089/thy.2020.0921. PMID: 34102860.
Article91. Kim BY, Choi N, Kim SW, Jeong HS, Chung MK, Son YI. 2020; Randomized trial of prophylactic ipsilateral central lymph node dissection in patients with clinically node negative papillary thyroid microcarcinoma. Eur Arch Otorhinolaryngol. 277(2):569–76. DOI: 10.1007/s00405-019-05702-3. PMID: 31664515.
Article92. Ito Y, Miyauchi A, Masuoka H, Fukushima M, Kihara M, Miya A. 2018; Excellent prognosis of central lymph node recurrence-free survival for cN0M0 papillary thyroid carcinoma patients who underwent routine prophylactic central node dissection. World J Surg. 42(8):2462–8. DOI: 10.1007/s00268-018-4497-x. PMID: 29372373. PMCID: PMC6060821.93. Kim M, Kim HI, Jeon MJ, Kim HK, Kim EH, Yi HS, et al. 2018; Eighth edition of tumor-node-metastasis staging system improve survival predictability for papillary, but not follicular thyroid carcinoma: a multicenter cohort study. Oral Oncol. 87:97–103. DOI: 10.1016/j.oraloncology.2018.10.029. PMID: 30527251.
Article94. Ito Y, Onoda N, Okamoto T. 2020; The revised clinical practice guidelines on the management of thyroid tumors by the Japan Associations of Endocrine Surgeons: core questions and recommendations for treatments of thyroid cancer. Endocr J. 67(7):669–717. DOI: 10.1507/endocrj.EJ20-0025. PMID: 32269182.
Article95. Song E, Kim WW, Jeon MJ, Sung TY, Song DE, Kim TY, et al. 2019; Clinical significance of gross invasion of strap muscles in patients with 1- to 4-cm-sized papillary thyroid carcinoma undergoing lobectomy. Ann Surg Oncol. 26(13):4466–71. DOI: 10.1245/s10434-019-07778-x. PMID: 31471840.
Article96. Jang SW, Park JH, Kim HR, Kwon HJ, Lee YM, Hong SJ, et al. 2023; Recurrence risk evaluation in patients with papillary thyroid carcinoma: multicenter machine learning evaluation of lymph node variables. Cancers (Basel). 15(2):550. DOI: 10.3390/cancers15020550. PMID: 36672498. PMCID: PMC9856505.
Article97. Alsubaie KM, Alsubaie HM, Alzahrani FR, Alessa MA, Abdulmonem SK, Merdad MA, et al. 2022; Prophylactic central neck dissection for clinically node-negative papillary thyroid carcinoma. Laryngoscope. 132(6):1320–8. DOI: 10.1002/lary.29912. PMID: 34708877.
Article98. Back K, Choe JH, Kim JS, Kim JH. 2021; Occult contralateral central neck metastasis in papillary thyroid carcinoma with preoperatively documented ipsilateral lateral neck metastasis. Eur J Surg Oncol. 47(6):1339–45. DOI: 10.1016/j.ejso.2021.01.008. PMID: 33744024.
Article99. Viola D, Materazzi G, Valerio L, Molinaro E, Agate L, Faviana P, et al. 2015; Prophylactic central compartment lymph node dissection in papillary thyroid carcinoma: clinical implications derived from the first prospective randomized controlled single institution study. J Clin Endocrinol Metab. 100(4):1316–24. DOI: 10.1210/jc.2014-3825. PMID: 25590215.
Article100. Ahn JH, Kwak JH, Yoon SG, Yi JW, Yu HW, Kwon H, et al. 2022; A prospective randomized controlled trial to assess the efficacy and safety of prophylactic central compartment lymph node dissection in papillary thyroid carcinoma. Surgery. 171(1):182–9. DOI: 10.1016/j.surg.2021.03.071. PMID: 34391573.
Article101. Wang Y, Xiao Y, Pan Y, Yang S, Li K, Zhao W, et al. 2022; The effectiveness and safety of prophylactic central neck dissection in clinically node-negative papillary thyroid carcinoma patients: a meta-analysis. Front Endocrinol (Lausanne). 13:1094012. DOI: 10.3389/fendo.2022.1094012. PMID: 36733809. PMCID: PMC9886572.102. Sanabria A, Betancourt-Aguero C, Sanchez-Delgado JG, Garcia-Lozano C. 2022; Prophylactic central neck lymph node dissection in low-risk thyroid carcinoma patients does not decrease the incidence of locoregional recurrence: a meta- analysis of randomized trials. Ann Surg. 276(1):66–73. DOI: 10.1097/SLA.0000000000005388. PMID: 35129470.
Article103. Chen L, Wu YH, Lee CH, Chen HA, Loh EW, Tam KW. 2018; Prophylactic central neck dissection for papillary thyroid carcinoma with clinically uninvolved central neck lymph nodes: a systematic review and meta-analysis. World J Surg. 42(9):2846–57. DOI: 10.1007/s00268-018-4547-4. PMID: 29488066.
Article104. Zhao WJ, Luo H, Zhou YM, Dai WY, Zhu JQ. 2017; Evaluating the effectiveness of prophylactic central neck dissection with total thyroidectomy for cN0 papillary thyroid carcinoma: an updated meta-analysis. Eur J Surg Oncol. 43(11):1989–2000. DOI: 10.1016/j.ejso.2017.07.008. PMID: 28807633.
Article105. Hartl DM, Mamelle E, Borget I, Leboulleux S, Mirghani H, Schlumberger M. 2013; Influence of prophylactic neck dissection on rate of retreatment for papillary thyroid carcinoma. World J Surg. 37(8):1951–8. DOI: 10.1007/s00268-013-2089-3. PMID: 23677562.
Article106. Conzo G, Calò PG, Sinisi AA, De Bellis A, Pasquali D, Iorio S, et al. 2014; Impact of prophylactic central compartment neck dissection on locoregional recurrence of differentiated thyroid cancer in clinically node-negative patients: a retrospective study of a large clinical series. Surgery. 155(6):998–1005. DOI: 10.1016/j.surg.2014.02.010. PMID: 24856120.
Article107. Perros P, Boelaert K, Colley S, Evans C, Evans RM, Gerrard Ba G, et al. 2014; Guidelines for the management of thyroid cancer. Clin Endocrinol (Oxf). 81 Suppl 1:1–122. DOI: 10.1111/cen.12515. PMID: 24989897.
Article108. Filetti S, Durante C, Hartl D, Leboulleux S, Locati LD, Newbold K, et al. 2019; Thyroid cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 30(12):1856–83. DOI: 10.1093/annonc/mdz400. PMID: 31549998.
Article109. Haddad RI, Bischoff L, Ball D, Bernet V, Blomain E, Busaidy NL, et al. 2022; Thyroid carcinoma, version 2.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 20(8):925–51. DOI: 10.6004/jnccn.2022.0040. PMID: 35948029.110. Yan S, Yu J, Zhao W, Wang B, Zhang L. 2022; Prophylactic bilateral central neck dissection should be evaluated based on prospective randomized study of 581 PTC patients. BMC Endocr Disord. 22(1):5. DOI: 10.1186/s12902-021-00909-0. PMID: 34983475. PMCID: PMC8725302.
Article111. Tao Y, Wang F, Shen X, Zhu G, Liu R, Viola D, et al. 2021; BRAF V600E status sharply differentiates lymph node metastasis-associated mortality risk in papillary thyroid cancer. J Clin Endocrinol Metab. 106(11):3228–38. DOI: 10.1210/clinem/dgab286. PMID: 34273152. PMCID: PMC8530728.112. Zhang Z, Zhang X, Yin Y, Zhao S, Wang K, Shang M, et al. 2022; Integrating BRAF(V600E) mutation, ultrasonic and clinicopathologic characteristics for predicting the risk of cervical central lymph node metastasis in papillary thyroid carcinoma. BMC Cancer. 22(1):461. DOI: 10.1186/s12885-022-09550-z. PMID: 35473554. PMCID: PMC9044661.
Article113. Erdem E, Gulcelik MA, Kuru B, Alagol H. 2003; Comparison of completion thyroidectomy and primary surgery for differentiated thyroid carcinoma. Eur J Surg Oncol. 29(9):747–9. DOI: 10.1016/j.ejso.2003.08.006. PMID: 14602494.
Article114. Tan MP, Agarwal G, Reeve TS, Barraclough BH, Delbridge LW. 2002; Impact of timing on completion thyroidectomy for thyroid cancer. Br J Surg. 89(6):802–4. DOI: 10.1046/j.1365-2168.2002.02068.x. PMID: 12027996.
Article115. Untch BR, Palmer FL, Ganly I, Patel SG, Michael Tuttle R, Shah JP, et al. 2014; Oncologic outcomes after completion thyroidectomy for patients with well-differentiated thyroid carcinoma. Ann Surg Oncol. 21(4):1374–8. DOI: 10.1245/s10434-013-3428-1. PMID: 24366419.
Article116. Li G, Li R, Song L, Chen W, Jiang K, Tang H, et al. 2020; Implications of extrathyroidal extension invading only the strap muscles in papillary thyroid carcinomas. Thyroid. 30(1):57–64. DOI: 10.1089/thy.2018.0801. PMID: 31830859.
Article117. Amit M, Boonsripitayanon M, Goepfert RP, Tam S, Busaidy NL, Cabanillas ME, et al. 2018; Extrathyroidal extension: does strap muscle invasion alone influence recurrence and survival in patients with differentiated thyroid cancer? Ann Surg Oncol. 25(11):3380–8. DOI: 10.1245/s10434-018-6563-x. PMID: 30022274.
Article118. Danilovic DLS, Castroneves LA, Suemoto CK, Elias LO, Soares IC, Camargo RY, et al. 2020; Is there a difference between minimal and gross extension into the strap muscles for the risk of recurrence in papillary thyroid carcinomas? Thyroid. 30(7):1008–16. DOI: 10.1089/thy.2019.0753. PMID: 32059626.
Article119. Kang IK, Kim K, Bae JS, Kim JS. 2021; Is completion thyroidectomy necessary in patients with papillary thyroid carcinoma who underwent lobectomy? Korean J Head Neck Oncol. 37(2):25–31. DOI: 10.21593/kjhno/2021.37.2.25.
Article120. Baloch ZW, Asa SL, Barletta JA, Ghossein RA, Juhlin CC, Jung CK, et al. 2022; Overview of the 2022 WHO classification of thyroid neoplasms. Endocr Pathol. 33(1):27–63. DOI: 10.1007/s12022-022-09707-3. PMID: 35288841.
Article121. Wreesmann VB, Nixon IJ, Rivera M, Katabi N, Palmer F, Ganly I, et al. 2015; Prognostic value of vascular invasion in well- differentiated papillary thyroid carcinoma. Thyroid. 25(5):503–8. DOI: 10.1089/thy.2015.0052. PMID: 25748079. PMCID: PMC4968276.
Article122. Suh YJ, Kwon H, Kim SJ, Choi JY, Lee KE, Park YJ, et al. 2015; Factors affecting the locoregional recurrence of conventional papillary thyroid carcinoma after surgery: a retrospective analysis of 3381 patients. Ann Surg Oncol. 22(11):3543–9. DOI: 10.1245/s10434-015-4448-9. PMID: 25743326.
Article123. de Castro TP, Waissmann W, Simoes TC, de Mello RC, Carvalho DP. 2016; Predictors for papillary thyroid cancer persistence and recurrence: a retrospective analysis with a 10-year follow-up cohort study. Clin Endocrinol (Oxf). 85(3):466–74. DOI: 10.1111/cen.13032. PMID: 26834009.
Article124. Sorrenti S, Carbotta G, Di Matteo FM, Catania A, Pironi D, Tartaglia F, et al. 2020; Evaluation of clinicopathological and molecular parameters on disease recurrence of papillary thyroid cancer patient: a retrospective observational study. Cancers (Basel). 12(12):3637. DOI: 10.3390/cancers12123637. PMID: 33291668. PMCID: PMC7761952.
Article125. Falvo L, Catania A, D'Andrea V, Marzullo A, Giustiniani MC, De Antoni E. 2005; Prognostic importance of histologic vascular invasion in papillary thyroid carcinoma. Ann Surg. 241(4):640–6. DOI: 10.1097/01.sla.0000157317.60536.08. PMID: 15798466. PMCID: PMC1357068.
Article126. Furlan JC, Bedard YC, Rosen IB. 2004; Clinicopathologic significance of histologic vascular invasion in papillary and follicular thyroid carcinomas. J Am Coll Surg. 198(3):341–8. DOI: 10.1016/j.jamcollsurg.2003.11.012. PMID: 14992733.127. Cao J, Hu JL, Chen C, Wang QL, Fang XH, Zhang Y, et al. 2016; Vascular invasion is an independent prognostic factor for distant recurrence-free survival in papillary thyroid carcinoma: a matched-case comparative study. J Clin Pathol. 69(10):872–7. DOI: 10.1136/jclinpath-2015-203547. PMID: 27010434.
Article128. Chereau N, Trésallet C, Noullet S, Godiris-Petit G, Tissier F, Leenhardt L, et al. 2016; Does the T1 subdivision correlate with the risk of recurrence of papillary thyroid cancer? Langenbecks Arch Surg. 401(2):223–30. DOI: 10.1007/s00423-016-1399-y. PMID: 26957089.
Article129. Gardner RE, Tuttle RM, Burman KD, Haddady S, Truman C, Sparling YH, et al. 2000; Prognostic importance of vascular invasion in papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg. 126(3):309–12. DOI: 10.1001/archotol.126.3.309. PMID: 10722002.
Article130. Akslen LA, Myking AO, Salvesen H, Varhaug JE. 1992; Prognostic importance of various clinicopathological features in papillary thyroid carcinoma. Eur J Cancer. 29A(1):44–51. DOI: 10.1016/0959-8049(93)90574-Y. PMID: 1445745.
Article131. Kang SW, Jeong JJ, Yun JS, Sung TY, Lee SC, Lee YS, et al. 2009; Robot-assisted endoscopic surgery for thyroid cancer: experience with the first 100 patients. Surg Endosc. 23(11):2399–406. DOI: 10.1007/s00464-009-0366-x. PMID: 19263137.
Article132. Lee KE, Rao J, Youn YK. 2009; Endoscopic thyroidectomy with the da Vinci robot system using the bilateral axillary breast approach (BABA) technique: our initial experience. Surg Laparosc Endosc Percutan Tech. 19(3):e71–5. DOI: 10.1097/SLE.0b013e3181a4ccae. PMID: 19542833.133. Singer MC, Seybt MW, Terris DJ. 2011; Robotic facelift thyroidectomy: I. Preclinical simulation and morphometric assessment. Laryngoscope. 121(8):1631–5. DOI: 10.1002/lary.21831. PMID: 21692075.
Article134. Richmon JD, Holsinger FC, Kandil E, Moore MW, Garcia JA, Tufano RP. 2011; Transoral robotic-assisted thyroidectomy with central neck dissection: preclinical cadaver feasibility study and proposed surgical technique. J Robot Surg. 5(4):279–82. DOI: 10.1007/s11701-011-0287-2. PMID: 22162981. PMCID: PMC3214254.
Article135. Lang BH, Wong CK, Tsang JS, Wong KP, Wan KY. 2015; A systematic review and meta-analysis evaluating completeness and outcomes of robotic thyroidectomy. Laryngoscope. 125(2):509–18. DOI: 10.1002/lary.24946. PMID: 25236330.
Article136. Martino B, Nitro L, De Pasquale L, Lozza P, Maccari A, Castellani L, et al. 2022; Conversion rates in robotic thyroid surgery: a systematic review and meta-analysis. Int J Med Robot. 18(5):e2427. DOI: 10.1002/rcs.2427. PMID: 35644881. PMCID: PMC9539493.
Article137. Sun GH, Peress L, Pynnonen MA. 2014; Systematic review and meta-analysis of robotic vs conventional thyroidectomy approaches for thyroid disease. Otolaryngol Head Neck Surg. 150(4):520–32. DOI: 10.1177/0194599814521779. PMID: 24500878.
Article138. Pan JH, Zhou H, Zhao XX, Ding H, Wei L, Qin L, et al. 2017; Robotic thyroidectomy versus conventional open thyroidectomy for thyroid cancer: a systematic review and meta-analysis. Surg Endosc. 31(10):3985–4001. DOI: 10.1007/s00464-017-5433-0. PMID: 28337546.
Article139. Wang YC, Liu K, Xiong JJ, Zhu JQ. 2015; Robotic thyroidectomy versus conventional open thyroidectomy for differentiated thyroid cancer: meta-analysis. J Laryngol Otol. 129(6):558–67. DOI: 10.1017/S002221511500122X. PMID: 26004423.
Article140. Kihara M, Miyauchi A, Yabuta T, Higashiyama T, Fukushima M, Ito Y, et al. 2014; Outcome of vocal cord function after partial layer resection of the recurrent laryngeal nerve in patients with invasive papillary thyroid cancer. Surgery. 155(1):184–9. DOI: 10.1016/j.surg.2013.06.052. PMID: 24646959.
Article141. Moritani S, Takenobu M, Yoshioka K, Kawamoto K, Fujii T, Yasunaga M, et al. 2021; Novel surgical methods for reconstruction of the recurrent laryngeal nerve: microscope- guided partial layer resection and intralaryngeal reconstruction of the recurrent laryngeal nerve. Surgery. 169(5):1124–30. DOI: 10.1016/j.surg.2020.09.017. PMID: 33092811.
Article142. Nishida T, Nakao K, Hamaji M, Kamiike W, Kurozumi K, Matsuda H. 1997; Preservation of recurrent laryngeal nerve invaded by differentiated thyroid cancer. Ann Surg. 226(1):85–91. DOI: 10.1097/00000658-199707000-00012. PMID: 9242342. PMCID: PMC1190911.
Article143. Kamani D, Darr EA, Randolph GW. 2013; Electrophysiologic monitoring characteristics of the recurrent laryngeal nerve preoperatively paralyzed or invaded with malignancy. Otolaryngol Head Neck Surg. 149(5):682–8. DOI: 10.1177/0194599813504735. PMID: 24046274.
Article144. Kim KH, Sung MW, Chang KH, Kang BS. 2000; Therapeutic dilemmas in the management of thyroid cancer with laryngotracheal involvement. Otolaryngol Head Neck Surg. 122(5):763–7. DOI: 10.1016/S0194-5998(00)70212-9. PMID: 10793362.
Article145. Iwaki S, Maeda T, Saito M, Otsuki N, Takahashi M, Wakui E, et al. 2017; Role of immediate recurrent laryngeal nerve reconstruction in surgery for thyroid cancers with fixed vocal cords. Head Neck. 39(3):427–31. DOI: 10.1002/hed.24627. PMID: 27997055.
Article146. Yuan Q, Hou J, Liao Y, Zheng L, Wang K, Wu G. 2020; Selective vagus-recurrent laryngeal nerve anastomosis in thyroidectomy with cancer invasion or iatrogenic transection. Langenbecks Arch Surg. 405(4):461–8. DOI: 10.1007/s00423-020-01906-y. PMID: 32504208.
Article147. Cody HS 3rd, Shah JP. 1981; Locally invasive, well-differentiated thyroid cancer. 22 years' experience at Memorial Sloan-Kettering Cancer Center. Am J Surg. 142(4):480–3. DOI: 10.1016/0002-9610(81)90379-2. PMID: 7283051.148. Wada N, Nakayama H, Masudo Y, Suganuma N, Rino Y. 2006; Clinical outcome of different modes of resection in papillary thyroid carcinomas with laryngotracheal invasion. Langenbecks Arch Surg. 391(6):545–9. DOI: 10.1007/s00423-006-0106-9. PMID: 17043903.
Article149. Shin DH, Mark EJ, Suen HC, Grillo HC. 1993; Pathologic staging of papillary carcinoma of the thyroid with airway invasion based on the anatomic manner of extension to the trachea: a clinicopathologic study based on 22 patients who underwent thyroidectomy and airway resection. Hum Pathol. 24(8):866–70. DOI: 10.1016/0046-8177(93)90136-5. PMID: 8375857.
Article150. McCarty TM, Kuhn JA, Williams WL Jr, Ellenhorn JD, O'Brien JC, Preskitt JT, et al. 1997; Surgical management of thyroid cancer invading the airway. Ann Surg Oncol. 4(5):403–8. DOI: 10.1007/BF02305553. PMID: 9259967.
Article151. McCaffrey JC. 2006; Aerodigestive tract invasion by well-differentiated thyroid carcinoma: diagnosis, management, prognosis, and biology. Laryngoscope. 116(1):1–11. DOI: 10.1097/01.MLG.0000200428.26975.86. PMID: 16481800.
Article152. Ito Y, Fukushima M, Yabuta T, Tomoda C, Inoue H, Kihara M, et al. 2009; Local prognosis of patients with papillary thyroid carcinoma who were intra-operatively diagnosed as having minimal invasion of the trachea: a 17-year experience in a single institute. Asian J Surg. 32(2):102–8. DOI: 10.1016/S1015-9584(09)60019-1. PMID: 19423457.
Article153. Su SY, Milas ZL, Bhatt N, Roberts D, Clayman GL. 2016; Well-differentiated thyroid cancer with aerodigestive tract invasion: long-term control and functional outcomes. Head Neck. 38(1):72–8. DOI: 10.1002/hed.23851. PMID: 25204531.
Article154. Wang LY, Nixon IJ, Patel SG, Palmer FL, Tuttle RM, Shaha A, et al. 2016; Operative management of locally advanced, differentiated thyroid cancer. Surgery. 160(3):738–46. DOI: 10.1016/j.surg.2016.04.027. PMID: 27302105. PMCID: PMC5126966.
Article155. Matsumoto F, Ikeda K. 2021; Surgical management of tracheal invasion by well-differentiated thyroid cancer. Cancers (Basel). 13(4):797. DOI: 10.3390/cancers13040797. PMID: 33672929. PMCID: PMC7918429.
Article156. Allen M, Spillinger A, Arianpour K, Johnson J, Johnson AP, Folbe AJ, et al. 2021; Tracheal resection in the management of thyroid cancer: an evidence-based approach. Laryngoscope. 131(4):932–46. DOI: 10.1002/lary.29112. PMID: 32985692.157. Ji YB, Tae K, Lee YS, Jeong JH, Lee SH, Kim KR, et al. 2009; Surgical management of tracheal invasion by differentiated thyroid cancer: how we do it. Clin Otolaryngol. 34(6):565–7. DOI: 10.1111/j.1749-4486.2009.02026.x. PMID: 20070768.
Article158. Musholt TJ, Musholt PB, Behrend M, Raab R, Scheumann GF, Klempnauer J. 1999; Invasive differentiated thyroid carcinoma: tracheal resection and reconstruction procedures in the hands of the endocrine surgeon. Surgery. 126(6):1078–87. discussion 87–8. DOI: 10.1067/msy.2099.102267. PMID: 10598191.
Article159. Shadmehr MB, Farzanegan R, Zangi M, Mohammadzadeh A, Sheikhy K, Pejhan S, et al. 2012; Thyroid cancers with laryngotracheal invasion. Eur J Cardiothorac Surg. 41(3):635–40. DOI: 10.1093/ejcts/ezr131. PMID: 22219428.
Article160. Park CS, Suh KW, Min JS. 1993; Cartilage-shaving procedure for the control of tracheal cartilage invasion by thyroid carcinoma. Head Neck. 15(4):289–91. DOI: 10.1002/hed.2880150403. PMID: 8360048.
Article161. Ozaki O, Sugino K, Mimura T, Ito K. 1995; Surgery for patients with thyroid carcinoma invading the trachea: circumferential sleeve resection followed by end-to-end anastomosis. Surgery. 117(3):268–71. DOI: 10.1016/S0039-6060(05)80200-4. PMID: 7878531.
Article162. Tsai YF, Tseng YL, Wu MH, Hung CJ, Lai WW, Lin MY. 2005; Aggressive resection of the airway invaded by thyroid carcinoma. Br J Surg. 92(11):1382–7. DOI: 10.1002/bjs.5124. PMID: 16044411.
Article163. Tsukahara K, Sugitani I, Kawabata K. 2009; Surgical management of tracheal shaving for papillary thyroid carcinoma with tracheal invasion. Acta Otolaryngol. 129(12):1498–502. DOI: 10.3109/00016480902725239. PMID: 19922104.
Article164. Warshavsky A, Rosen R, Nard-Carmel N, Muhanna N, Ungar O, Abergel A, et al. 2021; Outcomes of tracheal resections in well-differentiated thyroid cancer-a case series and meta-analysis. World J Surg. 45(9):2752–8. DOI: 10.1007/s00268-021-06172-7. PMID: 34023920.
Article165. Moritani S. 2017; Window resection for intraluminal cricotracheal invasion by papillary thyroid carcinoma. World J Surg. 41(7):1812–9. DOI: 10.1007/s00268-017-3927-5. PMID: 28243696.
Article166. Ebihara M, Kishimoto S, Hayashi R, Miyazaki M, Shinozaki T, Daiko H, et al. 2011; Window resection of the trachea and secondary reconstruction for invasion by differentiated thyroid carcinoma. Auris Nasus Larynx. 38(2):271–5. DOI: 10.1016/j.anl.2010.09.003. PMID: 21093183.
Article167. Brauckhoff M. 2014; Classification of aerodigestive tract invasion from thyroid cancer. Langenbecks Arch Surg. 399(2):209–16. DOI: 10.1007/s00423-013-1142-x. PMID: 24271275.
Article168. McCaffrey TV, Bergstralh EJ, Hay ID. 1994; Locally invasive papillary thyroid carcinoma: 1940-1990. Head Neck. 16(2):165–72. DOI: 10.1002/hed.2880160211. PMID: 8021137.
Article169. Nixon IJ, Simo R, Newbold K, Rinaldo A, Suarez C, Kowalski LP, et al. 2016; Management of invasive differentiated thyroid cancer. Thyroid. 26(9):1156–66. DOI: 10.1089/thy.2016.0064. PMID: 27480110. PMCID: PMC5118958.
Article170. Ballantyne AJ. 1994; Resections of the upper aerodigestive tract for locally invasive thyroid cancer. Am J Surg. 168(6):636–9. DOI: 10.1016/S0002-9610(05)80136-9. PMID: 7978010.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- ATA Guideline in a View Point of Nuclear Medicine
- Preoperative Staging of Well Differentiated Thyroid Cancer: US Is Enough?
- Evaluation and Management of Bone Health in Patients with Thyroid Diseases: A Position Statement of the Korean Thyroid Association
- Second Primary Malignancy after Radioiodine Treatment of Thyroid Disease: Current Status
- Management of Thyroid Nodules and Cancers Arising in the Elderly