Arch Hand Microsurg.
2024 Jun;29(2):127-131. 10.12790/ahm.24.0005.
Improved flap perfusion and hemostasis after postoperative embolization in free flap surgery: a case report
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Chungnam National University Hospital, Daejeon, Korea
- 2Department of Plastic and Reconstructive Surgery, Chungnam National University College of Medicine, Daejeon, Korea
- KMID: 2556364
- DOI: http://doi.org/10.12790/ahm.24.0005
Abstract
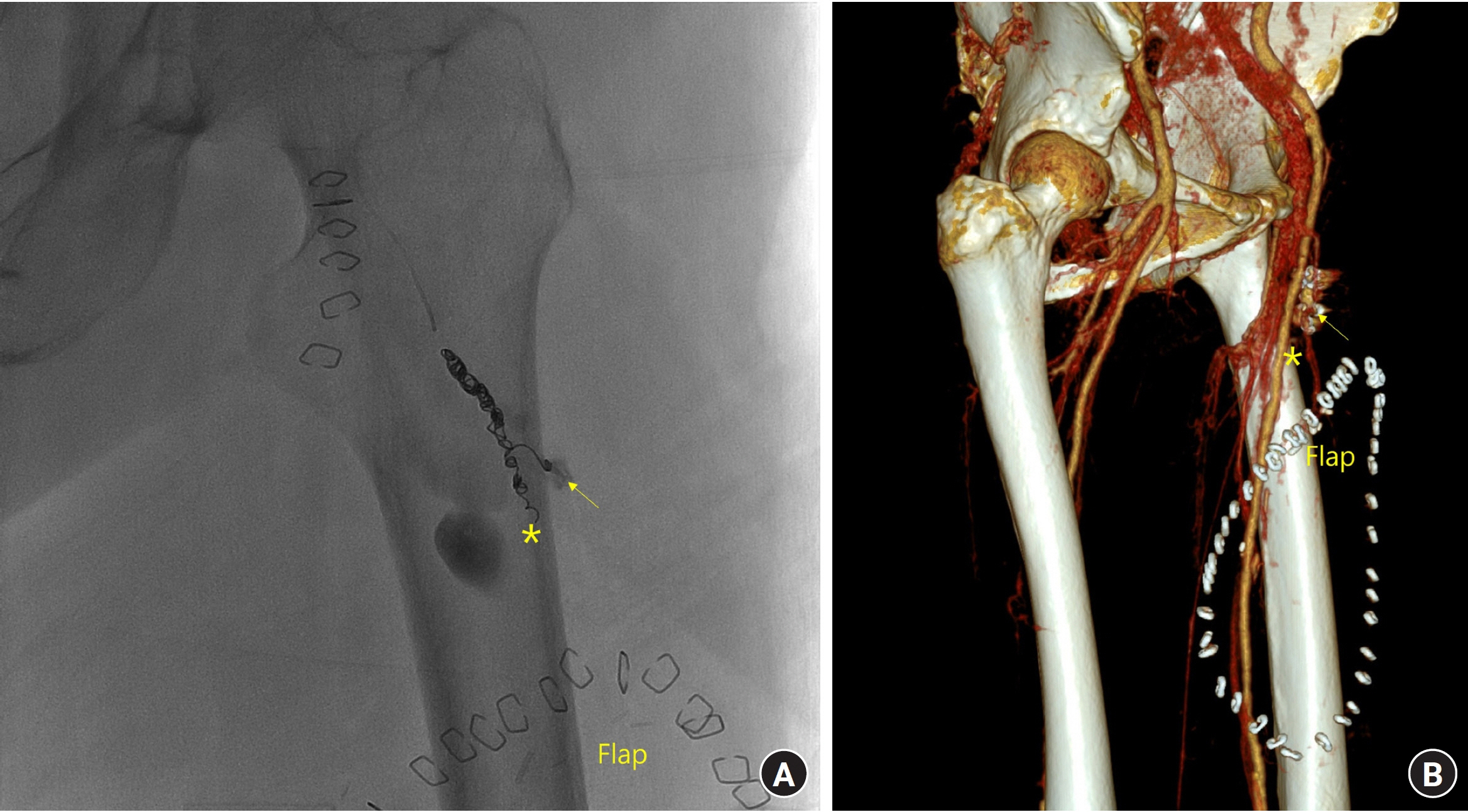
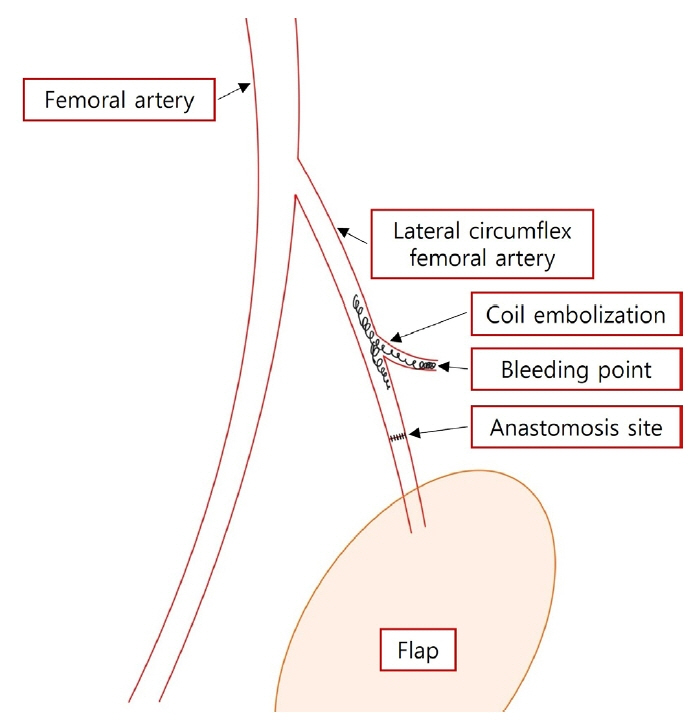
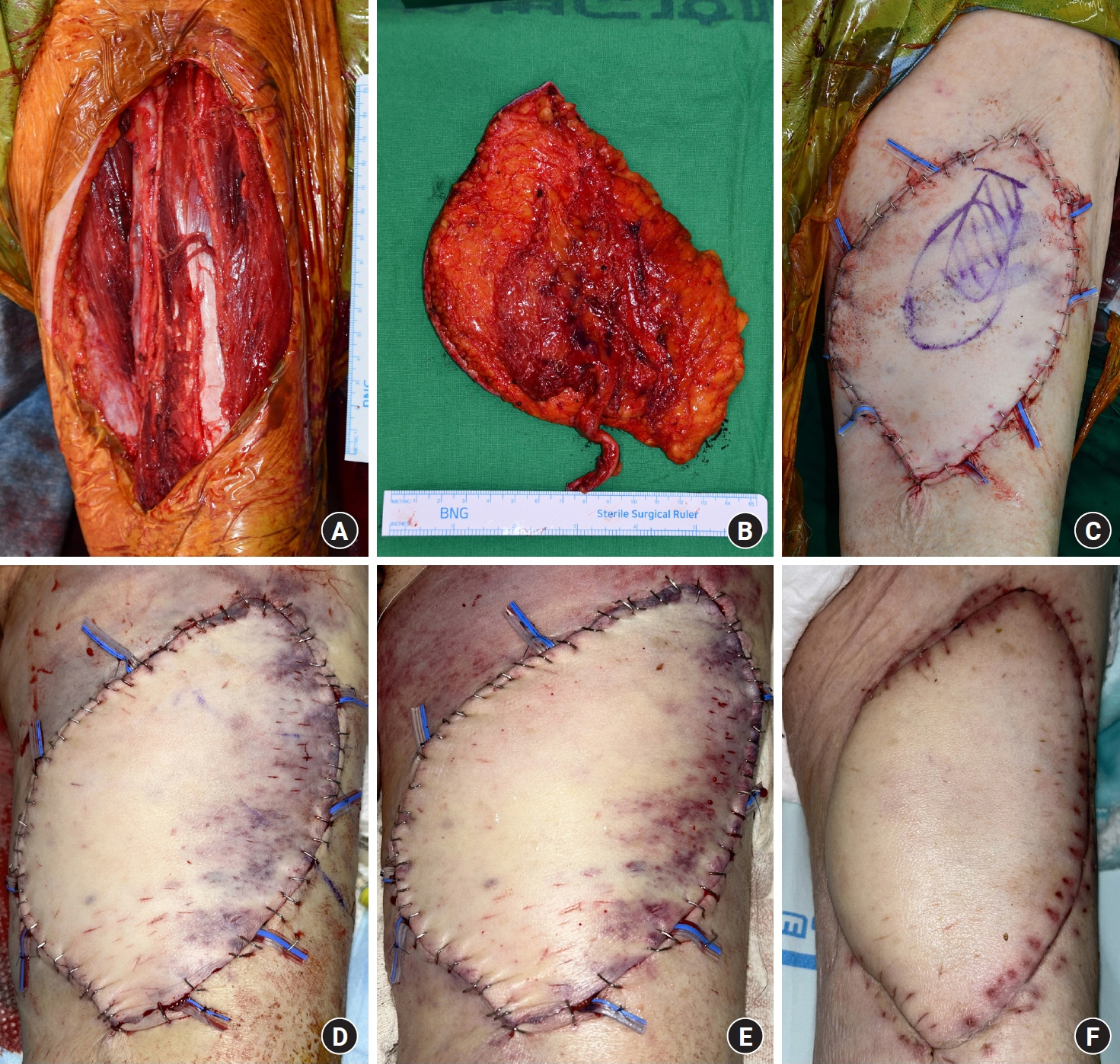
- This study aims to present a novel use of coil embolization in managing postoperative bleeding after free flap surgery, a technique typically reserved for other medical complications. We report the case of a 77-year-old female patient who underwent muscle-sparing latissimus dorsi free flap surgery for recurrent myxofibrosarcoma on her left thigh. Although hemostasis was achieved hemostasis during surgery, the patient experienced postoperative bleeding, which was initially managed with compression and blood transfusions. Upon a critical drop in the hemoglobin level, coil embolization was performed at the proximal segment of the descending branch of the lateral circumflex femoral artery. Coil embolization successfully controlled bleeding, while preserving blood flow to the flap. The patient’s hemoglobin levels stabilized, and the flap’s perfusion improved post-procedure. This approach proved effective in managing bleeding in areas other than the anastomosis site, with the patient showing a satisfactory recovery and no significant complications in the 30-day postoperative period. Coil embolization, a method commonly used for gastrointestinal bleeding and other vascular issues, can be a viable and effective option for controlling postoperative bleeding after free flap surgery. This case demonstrates its potential as a lifesaving intervention while preserving flap viability. However, further research with more cases is needed to evaluate the generalizability and long-term outcomes of this technique in similar surgical contexts.
Figure
Reference
-
References
1. Selber JC, Bergey M, Sonnad SS, Kovach S, Wu L, Serletti JM. Free flap breast reconstruction in advanced age: is it safe? Plast Reconstr Surg. 2009; 124:1015–22.
Article2. Hirche C, Kneser U, Xiong L, et al. Microvascular free flaps are a safe and suitable training procedure during structured plastic surgery residency: a comparative cohort study with 391 patients. J Plast Reconstr Aesthet Surg. 2016; 69:715–21.3. Koul AR, Patil RK, Nahar S. Unfavourable results in free tissue transfer. Indian J Plast Surg. 2013; 46:247–55.
Article4. Gal TJ, Cooperman LH. Hypertension in the immediate postoperative period. Br J Anaesth. 1975; 47:70–4.
Article5. Kim MJ, Woo KJ, Park BY, Kang SR. Effects of transfusion on free flap survival: searching for an optimal hemoglobin threshold for transfusion. J Reconstr Microsurg. 2018; 34:610–5.
Article6. Koshima I, Nanba Y, Tsutsui T, Takahashi Y, Watanabe A, Ishii R. Free perforator flap for the treatment of defects after resection of huge arteriovenous malformations in the head and neck regions. Ann Plast Surg. 2003; 51:194–9.
Article7. Islam S, Ali M, Avery C, Hayter JP. External carotid artery pseudoaneurysm following microvascular free flap reconstruction. The role of endovascular thrombin injection in embolization: a case report and review. Int J Oral Maxillofac Surg. 2014; 43:1069–72.
Article8. Yuen JC, Gray DJ. Endovascular treatment of a pseudoaneurysm of a recipient external carotid artery following radiation and free tissue transfer. Ann Plast Surg. 2000; 44:656–9.
Article9. Wolford H, Peterson SL, Ray C, Morgan SJ. Delayed arteriovenous fistula and pseudoaneurysm after an open tibial fracture successfully managed with selective angiographic embolization. J Trauma. 2001; 51:781–3.
Article10. Nikfarjam J, Taub PJ, Patel A, Rose E. Arteriovenous fistula following radial forearm free flap. J Reconstr Microsurg. 2011; 27:295–8.
Article