Arch Hand Microsurg.
2024 Jun;29(2):75-81. 10.12790/ahm.23.0043.
Effects of distal ulnar morphology on symptomatic extensor carpi ulnaris (ECU) subluxation and the clinical outcomes of anatomic ECU subsheath reconstruction: a retrospective observational study
- Affiliations
-
- 1Department of Orthopaedic Surgery, Center for Hand and Elbow Surgery, Konkuk University School of Medicine, Seoul, Korea
- KMID: 2556356
- DOI: http://doi.org/10.12790/ahm.23.0043
Abstract
- Purpose
This study aimed to evaluate the association between distal ulnar morphology and symptomatic extensor carpi ulnaris (ECU) subluxation and assess the results of anatomic ECU subsheath reconstruction.
Methods
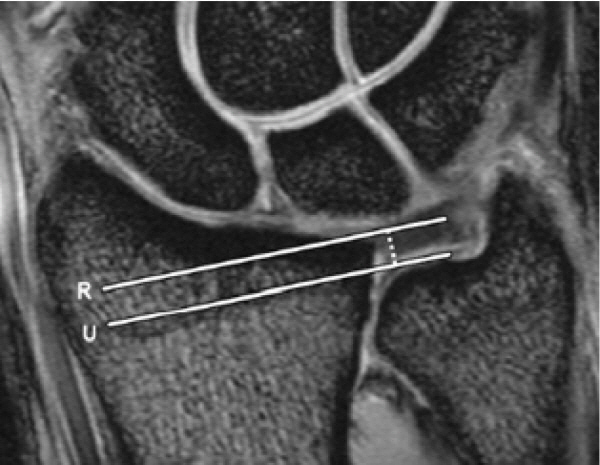
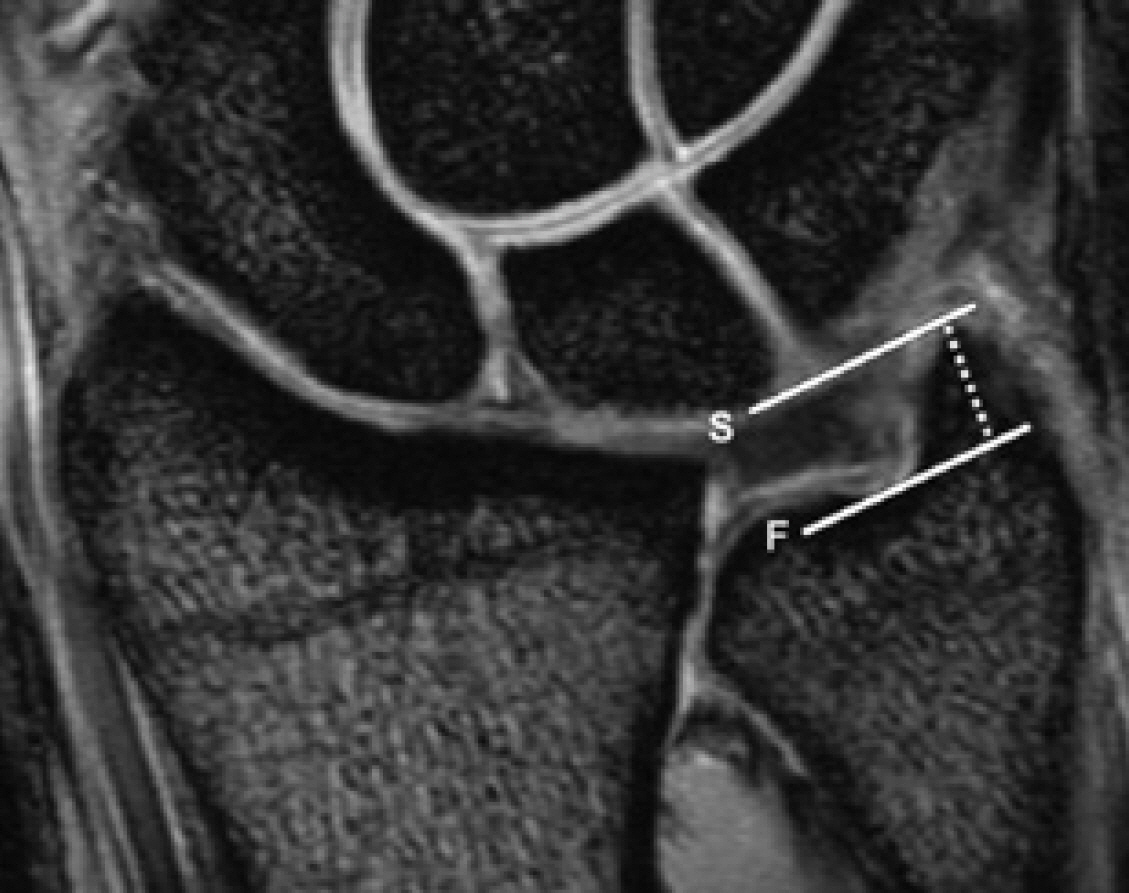
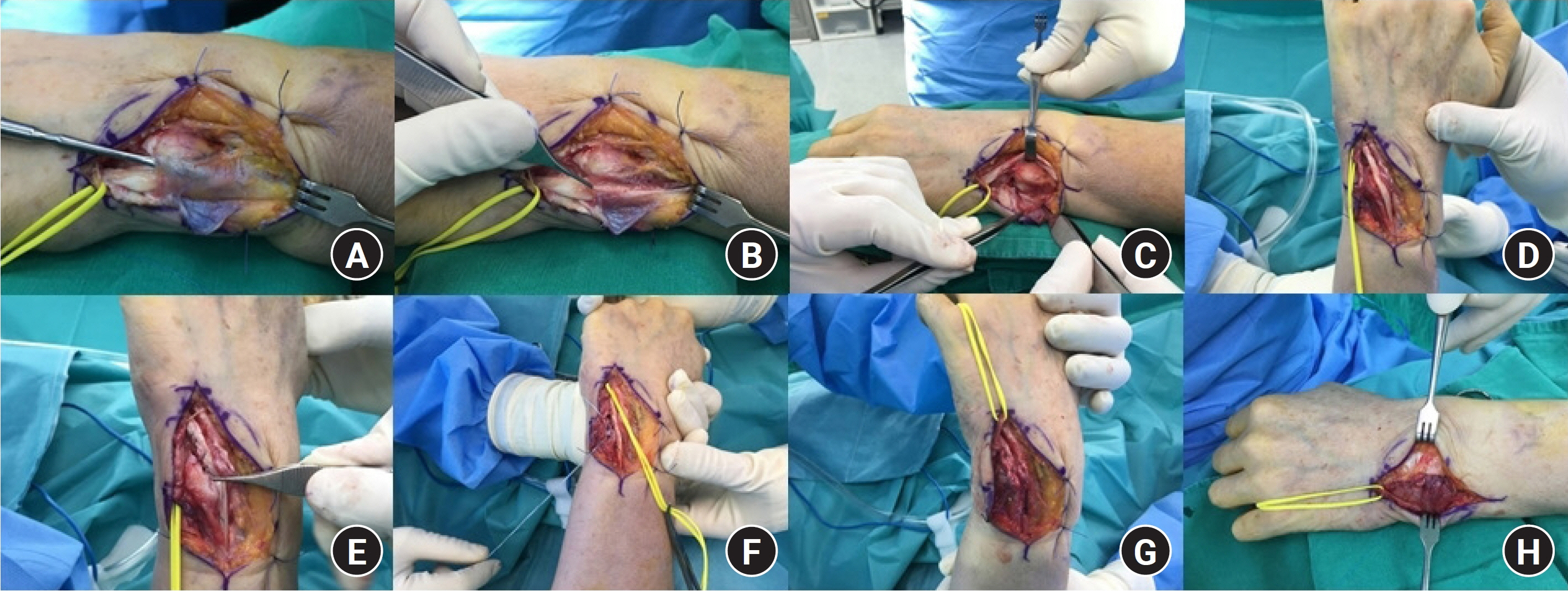
To investigate the effects of distal ulnar morphology on symptomatic ECU subluxation, we compared distal ulnar morphology using magnetic resonance imaging among three groups: group 1 (symptomatic ECU subluxation, 12 cases), group 2 (non-symptomatic ECU subluxation, 24 cases), and group 3 (no ECU subluxation, 24 cases). Distal ulnar morphology was evaluated using ulnar variance, ulnar styloid length, and ECU groove depth. Clinical outcomes were evaluated using the Patient-Related Wrist Evaluation (PRWE) score, the Disabilities of the Arm, Shoulder, Hand (DASH) score, grip strength, and the range of motion of the wrist joint.
Results
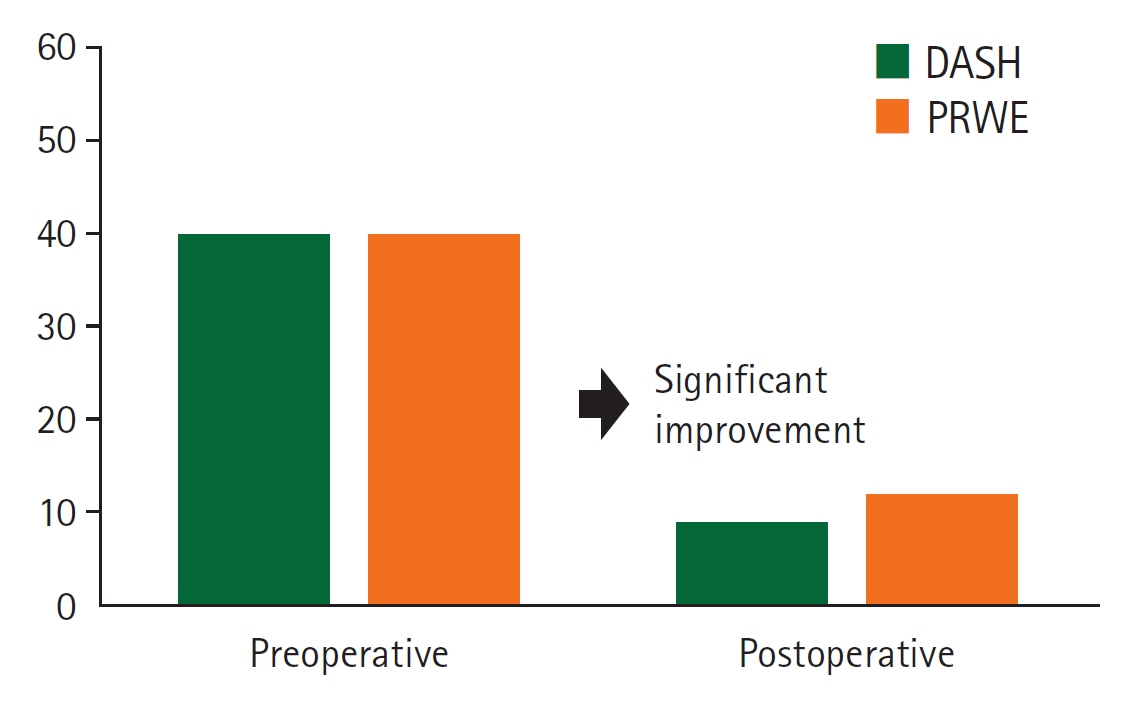
Ulnar variance showed a statistically significant difference between groups 1 and 2, and ECU groove depth showed statistically significant differences between groups 1 and 2 and between groups 2 and 3. Ulnar styloid length showed no statistically significant between-group differences. In patients with symptomatic ECU subluxation, there was a significant increase in the range of motion in supination and grip strength, and a significant decrease in the DASH score (from 40 to 9) and PRWE score (from 48 to 12).
Conclusion
Negative ulnar variance was associated with symptomatic ECU subluxation, and shallow ECU groove depth was correlated to asymptomatic ECU subluxation, but unrelated to symptoms. Anatomic ECU tendon sheath reconstruction was identified as an effective surgical method.
Figure
Reference
-
References
1. Allende C, Le Viet D. Extensor carpi ulnaris problems at the wrist: classification, surgical treatment and results. J Hand Surg Br. 2005; 30:265–72.2. Lee KS, Ablove RH, Singh S, et al. Ultrasound imaging of normal displacement of the extensor carpi ulnaris tendon within the ulnar groove in 12 forearm-wrist positions. AJR Am J Roentgenol. 2009; 193:651–5.
Article3. Vulpius J. Habitual dislocation of the extensor carpi ulnaris tendon. Acta Orthop Scand. 1964; 34:105–8.
Article4. Eckhardt WA, Palmer AK. Recurrent dislocation of extensor carpi ulnaris tendon. J Hand Surg Am. 1981; 6:629–31.
Article5. Inoue G, Tamura Y. Recurrent dislocation of the extensor carpi ulnaris tendon. Br J Sports Med. 1998; 32:172–4.
Article6. Rayan GM. Recurrent dislocation of the extensor carpi ulnaris in athletes. Am J Sports Med. 1983; 11:183–4.
Article7. Rowland SA. Acute traumatic subluxation of the extensor carpi ulnaris tendon at the wrist. J Hand Surg Am. 1986; 11:809–11.
Article8. MacLennan AJ, Nemechek NM, Waitayawinyu T, Trumble TE. Diagnosis and anatomic reconstruction of extensor carpi ulnaris subluxation. J Hand Surg Am. 2008; 33:59–64.
Article9. Montalvan B, Parier J, Brasseur JL, Le Viet D, Drape JL. Extensor carpi ulnaris injuries in tennis players: a study of 28 cases. Br J Sports Med. 2006; 40:424–9.
Article10. Burkhart SS, Wood MB, Linscheid RL. Posttraumatic recurrent subluxation of the extensor carpi ulnaris tendon. J Hand Surg Am. 1982; 7:1–3.
Article11. Iorio ML, Bayomy AF, Huang JI. Morphology of the extensor carpi ulnaris groove and tendon. J Hand Surg Am. 2014; 39:2412–6.12. Jeantroux J, Becce F, Guerini H, Montalvan B, Le Viet D, Drapé JL. Athletic injuries of the extensor carpi ulnaris subsheath: MRI findings and utility of gadolinium-enhanced fat-saturated T1-weighted sequences with wrist pronation and supination. Eur Radiol. 2011; 21:160–6.
Article13. Luijkx T, Buckens CF, van Seeters T, Pegge SA, Maas M. ECU tendon subluxation: a nonspecific MRI finding occurring in all wrist positions irrespective of ulnar-sided symptoms? Eur J Radiol. 2019; 116:192–7.
Article14. Petchprapa CN, Meraj S, Jain N. ECU tendon “dislocation” in asymptomatic volunteers. Skeletal Radiol. 2016; 45:805–12.
Article15. Chang CY, Huang AJ, Bredella MA, Kattapuram SV, Torriani M. Association between distal ulnar morphology and extensor carpi ulnaris tendon pathology. Skeletal Radiol. 2014; 43:793–800.
Article16. Graham TJ. Pathologies of the extensor carpi ulnaris (ECU) tendon and its investments in the athlete. Hand Clin. 2012; 28:345–56.
Article17. Bateni CP, Bartolotta RJ, Richardson ML, Mulcahy H, Allan CH. Imaging key wrist ligaments: what the surgeon needs the radiologist to know. AJR Am J Roentgenol. 2013; 200:1089–95.
Article18. Puri SK, Morse KW, Hearns KA, Carlson MG. A biomechanical comparison of extensor carpi ulnaris subsheath reconstruction techniques. J Hand Surg Am. 2017; 42:837.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Subluxation of the Extensor Carpi Ulnaris Tendon Associated with the Extensor Digitorum Tendon Subluxation of the Long Finger
- Operative Treatment for Extensor Carpi Ulnaris Tendon Dislocation
- Tendon Problems of the Ulnar Wrist
- Ulnar nerve Compression Syndrome due to anomalous Branch of the Ulnar Nerve Piercing the Flexor Carpi Ulnaris: Report of one case
- Management of the Comminuted Fractures of the Ulnar Head and Neck Combined with Distal Radius Fractures by Darrach Procedure and Tenodesis of Extensor Carpi Ulnaris