Ewha Med J.
2024 Apr;47(2):e15. 10.12771/emj.2024.e15.
Sex differences in coronary atherogenesis: a narrative review
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2556304
- DOI: http://doi.org/10.12771/emj.2024.e15
Abstract
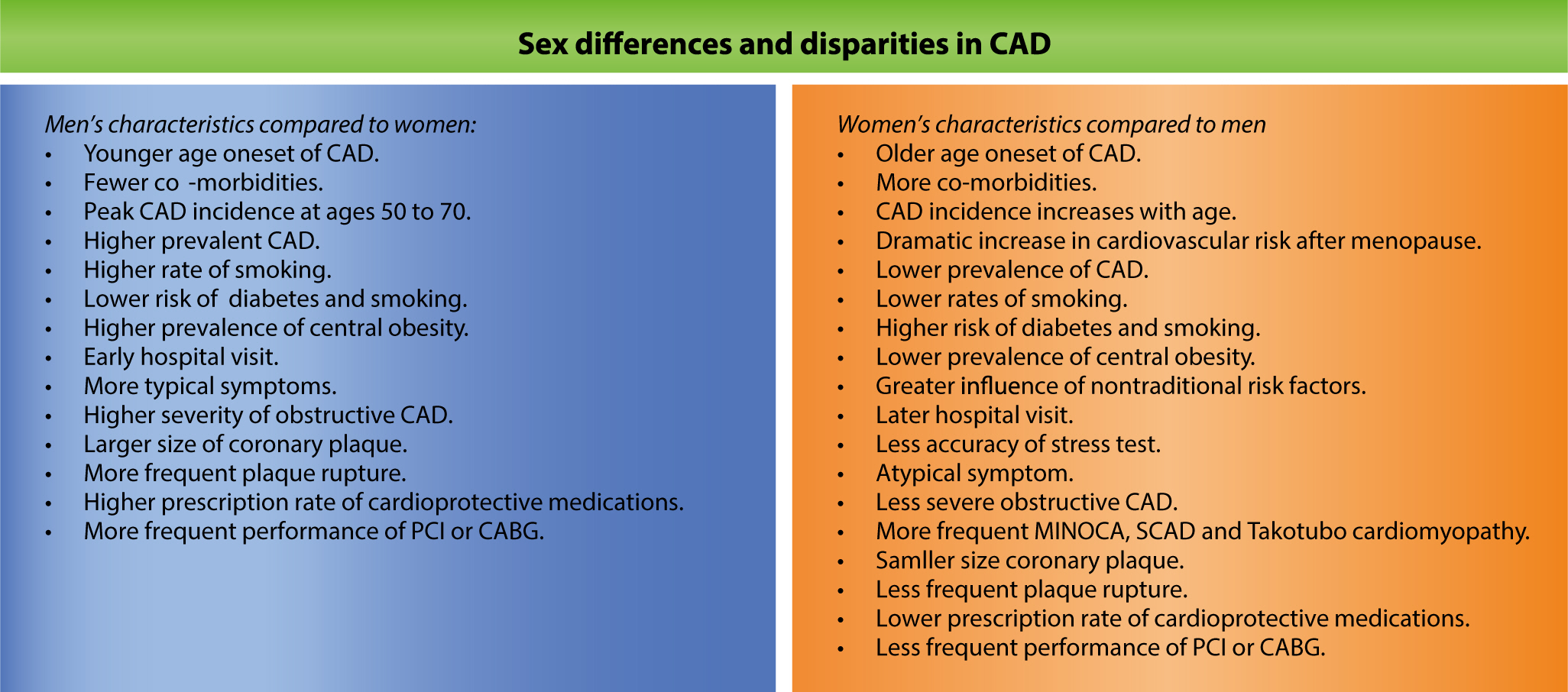
- Coronary artery disease (CAD) remains the leading cause of mortality worldwide, driven primarily by atherogenesis. Recent efforts to understand sex differences in CAD have revealed distinct patterns in disease burden, risk factors, and clinical presentations. This review examines these sex differences in CAD, underscoring the importance of customized diagnostic and management strategies. Although men typically have higher rates of CAD prevalence and incidence, women face unique challenges, such as delayed diagnosis, atypical symptoms, and lower rates of medication prescription. Hormonal, genetic, and lifestyle factors all play a role in these disparities, with estrogen notably reducing CAD risk in women. Nontraditional risk factors, including chronic inflammation, psychological stress, socioeconomic status, and reproductive history, also contribute to CAD development and are often neglected in clinical settings. Addressing these differences requires increased awareness, more accurate diagnosis, and equitable healthcare access for both sexes. Furthermore, greater inclusion of women in CAD research is essential to better understand sex-specific mechanisms and optimize treatment outcomes. Personalizing CAD management based on sex-specific knowledge has the potential to improve prognosis and decrease disease incidence for both men and women.
Figure
Reference
-
References
1. Tsao CW, Aday AW, Almarzooq ZI, Anderson CAM, Arora P, Avery CL, et al. Heart disease and stroke statistics—2023 update: a report from the American Heart Association. Circulation. 2023; 147(8):e93–e621. DOI: 10.1161/CIR.0000000000001123. PMID: 36695182.2. Libby P, Buring JE, Badimon L, Hansson GK, Deanfield J, Bittencourt MS, et al. Atherosclerosis. Nat Rev Dis Primers. 2019; 5(1):56. DOI: 10.1038/s41572-019-0106-z. PMID: 31420554.3. Vogel B, Acevedo M, Appelman Y, Noel Bairey Merz C, Chieffo A, Figtree GA, et al. The Lancet women and cardiovascular disease commission: reducing the global burden by 2030. Lancet. 2021; 397(10292):2385–2438. DOI: 10.1016/S0140-6736(21)00684-X. PMID: 34010613.4. Mosca L, Barrett-Connor E, Wenger NK. Sex/gender differences in cardiovascular disease prevention: what a difference a decade makes. Circulation. 2011; 124(19):2145–2154. DOI: 10.1161/CIRCULATIONAHA.110.968792. PMID: 22064958. PMCID: PMC3362050.5. Chen SQ, Liu J, Zhou Y, Huang ZD, Xie Y, Huang HZ, et al. Sex differences in characteristics, treatments, and in-hospital outcomes of patients undergoing coronary angiography or intervention. Front Cardiovasc Med. 2022; 9:878566. DOI: 10.3389/fcvm.2022.878566. PMID: 35571216. PMCID: PMC9106109.6. Kim SR, Bae SA, Lee JY, Kim MS, Kim MN, Chung WJ, et al. Gender disparities in prevalence by diagnostic criteria, treatment and mortality of newly diagnosed acute myocardial infarction in Korean adults. Sci Rep. 2023; 13(1):4120. DOI: 10.1038/s41598-023-31014-y. PMID: 36914709. PMCID: PMC10011387.7. Kim HL, Kim HJ, Kim M, Park SM, Yoon HJ, Byun YS, et al. Sex differences in coronary angiographic findings in patients with stable chest pain: analysis of data from the KoRean wOmen'S chest pain rEgistry (KoROSE). Biol Sex Differ. 2022; 13(1):2. DOI: 10.1186/s13293-021-00411-1. PMID: 34980251. PMCID: PMC8722299.8. Okunrintemi V, Tibuakuu M, Virani SS, Sperling LS, Volgman AS, Gulati M, et al. Sex differences in the age of diagnosis for cardiovascular disease and its risk factors among US adults: trends from 2008 to 2017, the medical expenditure panel survey. J Am Heart Assoc. 2020; 9(24):e018764. DOI: 10.1161/JAHA.120.018764. PMID: 33161825. PMCID: PMC7955360.9. Kim HL, Jang JS, Kim MA, Seo JB, Chung WY, Kim SH, et al. Gender differences of in-hospital outcomes in patients undergoing percutaneous coronary intervention in the drug-eluting stent era. Medicine. 2019; 98(20):e15557. DOI: 10.1097/MD.0000000000015557. PMID: 31096458. PMCID: PMC6531253.10. Madhavan MV, Gersh BJ, Alexander KP, Granger CB, Stone GW. Coronary artery disease in patients ≥80 years of age. J Am Coll Cardiol. 2018; 71(18):2015–2040. DOI: 10.1016/j.jacc.2017.12.068. PMID: 29724356.11. Wenger NK. Coronary heart disease: an older woman's major health risk. BMJ. 1997; 315(7115):1085–1090. DOI: 10.1136/bmj.315.7115.1085. PMID: 9366743. PMCID: PMC2127693.12. Kannel WB, Vasan RS. Is age really a non-modifiable cardiovascular risk factor? Am J Cardiol. 2009; 104(9):1307–1310. DOI: 10.1016/j.amjcard.2009.06.051. PMID: 19840582. PMCID: PMC3760670.13. Saltiki K, Doukas C, Kanakakis J, Anastasiou E, Mantzou E, Alevizaki M. Severity of cardiovascular disease in women: relation with exposure to endogenous estrogen. Maturitas. 2006; 55(1):51–57. DOI: 10.1016/j.maturitas.2005.12.008. PMID: 16464546.14. Ossewaarde ME, Bots ML, Verbeek AL, Peeters PH, van der Graaf Y, Grobbee DE, et al. Age at menopause, cause-specific mortality and total life expectancy. Epidemiology. 2005; 16(4):556–562. DOI: 10.1097/01.ede.0000165392.35273.d4. PMID: 15951675.15. Somani YB, Pawelczyk JA, De Souza MJ, Kris-Etherton PM, Proctor DN. Aging women and their endothelium: probing the relative role of estrogen on vasodilator function. Am J Physiol Heart Circ Physiol. 2019; 317(2):H395–H404. DOI: 10.1152/ajpheart.00430.2018. PMID: 31173499. PMCID: PMC6732482.16. Straub RH. The complex role of estrogens in inflammation. Endocr Rev. 2007; 28(5):521–574. DOI: 10.1210/er.2007-0001. PMID: 17640948.17. Niranjan MK, Koiri RK, Srivastava R. Expression of estrogen receptor alpha in response to stress and estrogen antagonist tamoxifen in the shell gland of Gallus gallus domesticus: involvement of anti-oxidant system and estrogen. Stress. 2021; 24(3):261–272. DOI: 10.1080/10253890.2019.1710127. PMID: 31885314.18. Janssen I, Powell LH, Kazlauskaite R, Dugan SA. Testosterone and visceral fat in midlife women: the Study of Women's Health Across the Nation (SWAN) fat patterning study. Obesity. 2010; 18(3):604–610. DOI: 10.1038/oby.2009.251. PMID: 19696765. PMCID: PMC2866448.19. Barton M. Cholesterol and atherosclerosis: modulation by oestrogen. Curr Opin Lipidol. 2013; 24(3):214–220. DOI: 10.1097/MOL.0b013e3283613a94. PMID: 23594711.20. Burke AP, Farb A, Malcom G, Virmani R. Effect of menopause on plaque morphologic characteristics in coronary atherosclerosis. Am Heart J. 2001; 141(2):S58–S62. DOI: 10.1067/mhj.2001.109946. PMID: 11174360.21. Taddei S, Virdis A, Ghiadoni L, Mattei P, Sudano I, Bernini G, et al. Menopause is associated with endothelial dysfunction in women. Hypertension. 1996; 28(4):576–582. DOI: 10.1161/01.HYP.28.4.576. PMID: 8843881.22. Kim HL. Differences in risk factors for coronary atherosclerosis according to sex. J Lipid Atheroscler. 2024; 13:e12. DOI: 10.12997/jla.2024.13.2.97.23. Iorga A, Cunningham CM, Moazeni S, Ruffenach G, Umar S, Eghbali M. The protective role of estrogen and estrogen receptors in cardiovascular disease and the controversial use of estrogen therapy. Biol Sex Differ. 2017; 8(1):33. DOI: 10.1186/s13293-017-0152-8. PMID: 29065927. PMCID: PMC5655818.24. Brahmbhatt Y, Gupta M, Hamrahian S. Hypertension in premenopausal and postmenopausal women. Curr Hypertens Rep. 2019; 21(10):74. DOI: 10.1007/s11906-019-0979-y. PMID: 31451980.25. Appelman Y, van Rijn BB, ten Haaf ME, Boersma E, Peters SAE. Sex differences in cardiovascular risk factors and disease prevention. Atherosclerosis. 2015; 241(1):211–218. DOI: 10.1016/j.atherosclerosis.2015.01.027. PMID: 25670232.26. Juutilainen A, Kortelainen S, Lehto S, Rönnemaa T, Pyörälä K, Laakso M. Gender difference in the impact of type 2 diabetes on coronary heart disease risk. Diabetes Care. 2004; 27(12):2898–2904. DOI: 10.2337/diacare.27.12.2898. PMID: 15562204.27. Huxley R, Barzi F, Woodward M. Excess risk of fatal coronary heart disease associated with diabetes in men and women: meta-analysis of 37 prospective cohort studies. BMJ. 2006; 332(7533):73–78. DOI: 10.1136/bmj.38678.389583.7C. PMID: 16371403. PMCID: PMC1326926.28. Gnatiuc L, Herrington WG, Halsey J, Tuomilehto J, Fang X, Kim HC, et al. Sex-specific relevance of diabetes to occlusive vascular and other mortality: a collaborative meta-analysis of individual data from 980 793 adults from 68 prospective studies. Lancet Diabetes Endocrinol. 2018; 6(7):538–546. DOI: 10.1016/S2213-8587(18)30079-2. PMID: 29752194.29. Abbey M, Owen A, Suzakawa M, Roach P, Nestel PJ. Effects of menopause and hormone replacement therapy on plasma lipids, lipoproteins and LDL-receptor activity. Maturitas. 1999; 33(3):259–269. DOI: 10.1016/S0378-5122(99)00054-7. PMID: 10656504.30. Prescott E, Hippe M, Schnohr P, Hein HO, Vestbo J. Smoking and risk of myocardial infarction in women and men: longitudinal population study. BMJ. 1998; 316(7137):1043–1047. DOI: 10.1136/bmj.316.7137.1043. PMID: 9552903. PMCID: PMC28505.31. Grundtvig M, Hagen TP, German M, Reikvam A. Sex-based differences in premature first myocardial infarction caused by smoking: twice as many years lost by women as by men. Eur J Cardiovasc Prev Rehabil. 2009; 16(2):174–179. DOI: 10.1097/HJR.0b013e328325d7f0. PMID: 19247184.32. Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009; 373(9669):1083–1096. DOI: 10.1016/S0140-6736(09)60318-4. PMID: 19299006.33. Després JP. Body fat distribution and risk of cardiovascular disease: an update. Circulation. 2012; 126(10):1301–1313. DOI: 10.1161/CIRCULATIONAHA.111.067264. PMID: 22949540.34. Kim HL, Kim MA. Sex differences in coronary artery disease: insights from the KoRean wOmen'S chest pain rEgistry (KoROSE). Korean Circ J. 2023; 53(10):655–676. DOI: 10.4070/kcj.2023.0205. PMID: 37880830. PMCID: PMC10625849.35. Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005; 352(16):1685–1695. DOI: 10.1056/NEJMra043430. PMID: 15843671.36. Mason JC, Libby P. Cardiovascular disease in patients with chronic inflammation: mechanisms underlying premature cardiovascular events in rheumatologic conditions. Eur Heart J. 2015; 36(8):482–489. DOI: 10.1093/eurheartj/ehu403. PMID: 25433021. PMCID: PMC4340364.37. Steptoe A, Kivimäki M. Stress and cardiovascular disease. Nat Rev Cardiol. 2012; 9(6):360–370. DOI: 10.1038/nrcardio.2012.45. PMID: 22473079.38. Vaccarino V, Sullivan S, Hammadah M, Wilmot K, Al Mheid I, Ramadan R, et al. Mental stress–induced-myocardial ischemia in young patients with recent myocardial infarction: sex differences and mechanisms. Circulation. 2018; 137(8):794–805. DOI: 10.1161/CIRCULATIONAHA.117.030849. PMID: 29459465. PMCID: PMC5822741.39. Backholer K, Peters SAE, Bots SH, Peeters A, Huxley RR, Woodward M. Sex differences in the relationship between socioeconomic status and cardiovascular disease: a systematic review and meta-analysis. J Epidemiol Community Health. 2017; 71(6):550–557. DOI: 10.1136/jech-2016-207890. PMID: 27974445.40. Kelly AC, Michos ED, Shufelt CL, Vermunt JV, Minissian MB, Quesada O, et al. Pregnancy and reproductive risk factors for cardiovascular disease in women. Circ Res. 2022; 130(4):652–672. DOI: 10.1161/CIRCRESAHA.121.319895. PMID: 35175837. PMCID: PMC8870397.41. Søndergaard MM, Hlatky MA, Stefanick ML, Vittinghoff E, Nah G, Allison M, et al. Association of adverse pregnancy outcomes with risk of atherosclerotic cardiovascular disease in postmenopausal women. JAMA Cardiol. 2020; 5(12):1390–1398. DOI: 10.1001/jamacardio.2020.4097. PMID: 32936228. PMCID: PMC7495331.42. Yerly A, van der Vorst EPC, Baumgartner I, Bernhard SM, Schindewolf M, Döring Y. Sex-specific and hormone-related differences in vascular remodelling in atherosclerosis. Eur J Clin Invest. 2023; 53(1):e13885. DOI: 10.1111/eci.13885. PMID: 36219492.43. Yahagi K, Davis HR, Arbustini E, Virmani R. Sex differences in coronary artery disease: pathological observations. Atherosclerosis. 2015; 239(1):260–267. DOI: 10.1016/j.atherosclerosis.2015.01.017. PMID: 25634157.44. Arbustini E, Dal Bello B, Morbini P, Burke AP, Bocciarelli M, Specchia G, et al. Plaque erosion is a major substrate for coronary thrombosis in acute myocardial infarction. Heart. 1999; 82(3):269–272. DOI: 10.1136/hrt.82.3.269. PMID: 10455073. PMCID: PMC1729173.45. Cho DH, Choi J, Kim MN, Kim HL, Kim YH, Na JO, et al. Gender differences in the presentation of chest pain in obstructive coronary artery disease: results from the Korean Women's Chest Pain Registry. Korean J Intern Med. 2020; 35(3):582–592. DOI: 10.3904/kjim.2018.320. PMID: 30879289. PMCID: PMC7214370.46. La S, Beltrame J, Tavella R. Sex-specific and ethnicity-specific differences in MINOCA. Nat Rev Cardiol. 2024; 21(3):192–202. DOI: 10.1038/s41569-023-00927-6. PMID: 37775559.47. Kaul P, Armstrong PW, Sookram S, Leung BK, Brass N, Welsh RC. Temporal trends in patient and treatment delay among men and women presenting with ST-elevation myocardial infarction. Am Heart J. 2011; 161(1):91–97. DOI: 10.1016/j.ahj.2010.09.016. PMID: 21167339.48. Daly C, Clemens F, Lopez Sendon JL, Tavazzi L, Boersma E, Danchin N, et al. Gender differences in the management and clinical outcome of stable angina. Circulation. 2006; 113(4):490–498. DOI: 10.1161/CIRCULATIONAHA.105.561647. PMID: 16449728.49. Zhao M, Woodward M, Vaartjes I, Millett ERC, Klipstein‐Grobusch K, Hyun K, et al. Sex differences in cardiovascular medication prescription in primary care: a systematic review and meta‐analysis. J Am Heart Assoc. 2020; 9(11):e014742. DOI: 10.1161/JAHA.119.014742. PMID: 32431190. PMCID: PMC7429003.50. Agarwala A, Goldberg A. Special considerations for lipid-lowering therapy in women reflecting recent randomized trials. Curr Atheroscler Rep. 2021; 23(8):42. DOI: 10.1007/s11883-021-00942-3. PMID: 34146167.51. Whitelaw S, Sullivan K, Eliya Y, Alruwayeh M, Thabane L, Yancy CW, et al. Trial characteristics associated with under-enrolment of females in randomized controlled trials of heart failure with reduced ejection fraction: a systematic review. Eur J Heart Fail. 2021; 23(1):15–24. DOI: 10.1002/ejhf.2034. PMID: 33118664.52. Kim HJ, Kim HY, Kim HL, Park SM, Cho DH, Kim M, et al. Awareness of cardiovascular disease among Korean women: results from a nationwide survey. Prev Med Rep. 2022; 26:101698. DOI: 10.1016/j.pmedr.2022.101698. PMID: 35111568. PMCID: PMC8789602.53. Mosca L, Hammond G, Mochari-Greenberger H, Towfighi A, Albert MA. Fifteen-year trends in awareness of heart disease in women: results of a 2012 American Heart Association national survey. Circulation. 2013; 127(11):1254–1263. DOI: 10.1161/CIR.0b013e318287cf2f. PMID: 23429926. PMCID: PMC3684065.54. Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation. 2018; 137(12):e67–e492. DOI: 10.1161/CIR.0000000000000558. PMCID: PMC6085757.55. Smith GN, Louis JM, Saade GR. Pregnancy and the postpartum period as an opportunity for cardiovascular risk identification and management. Obstet Gynecol. 2019; 134(4):851–862. DOI: 10.1097/AOG.0000000000003363. PMID: 31503139.56. Tannenbaum C, Norris CM, Sean McMurtry M. Sex-specific considerations in guidelines generation and application. Can J Cardiol. 2019; 35(5):598–605. DOI: 10.1016/j.cjca.2018.11.011. PMID: 30910247.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Considerations for Chronic Pain Management Based on Sex Differences: A Narrative Review
- Sex differences in metabolic dysfunction-associated steatotic liver disease: a narrative review
- Sex differences in the prevalence of common comorbidities in autism: a narrative review
- Current status and significance of research on sex differences in neuroscience: a narrative review and bibliometric analysis
- Sex Differences in Coronary Artery Disease: Insights From the KoRean wOmen’S chest pain rEgistry (KoROSE)