J Korean Med Sci.
2024 Jun;39(21):e172. 10.3346/jkms.2024.39.e172.
The Impact of an Antimicrobial Stewardship Program on Days of Therapy in the Pediatric Center: An Interrupted Time-Series Analysis of a 19-Year Study
- Affiliations
-
- 1Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Pharmacy, Samsung Medical Center, Seoul, Korea
- 3Sungkyunkwan University School of Pharmacy, Suwon, Korea
- 4Research Institute for Future Medicine, Samsung Medical Center, Seoul, Korea
- 5Department of Pediatrics, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea
- 6Department of Pediatrics, Seoulsan Boram Hospital, Ulsan, Korea
- 7Samsung Dream Pediatric Clinic, Suwon, Korea
- 8Department of Pediatrics, Myongji Hospital, Goyang, Korea
- 9Department of Pediatrics, Severance Children’s Hospital, Yonsei University College of Medicine, Seoul, Korea
- 10Samsung Dream Pediatric Clinic, Jeju, Korea
- 11Wonju Citizen Clinic, Wonju, Korea
- 12Department of Pediatrics, Kyungpook National University Hospital, Kyungpook National University School of Medicine, Daegu, Korea
- 13Department of Pediatrics, Gangnam Severance Hospital, Seoul, Korea
- 14Department of Pediatrics, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea
- 15Department of Pediatrics, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea
- 16Academic Research Service Headquarter, LSK Global PS, Seoul, Korea
- 17Department of Health Sciences and Technology, Samsung Advanced Institute for Health Sciences and Technology, Seoul, Korea
- KMID: 2556289
- DOI: http://doi.org/10.3346/jkms.2024.39.e172
Abstract
- Background
We aimed to analyze the effects of an antimicrobial stewardship program (ASP) on the proportion of antimicrobial-resistant pathogens in bacteremia, antimicrobial use, and mortality in pediatric patients.
Methods
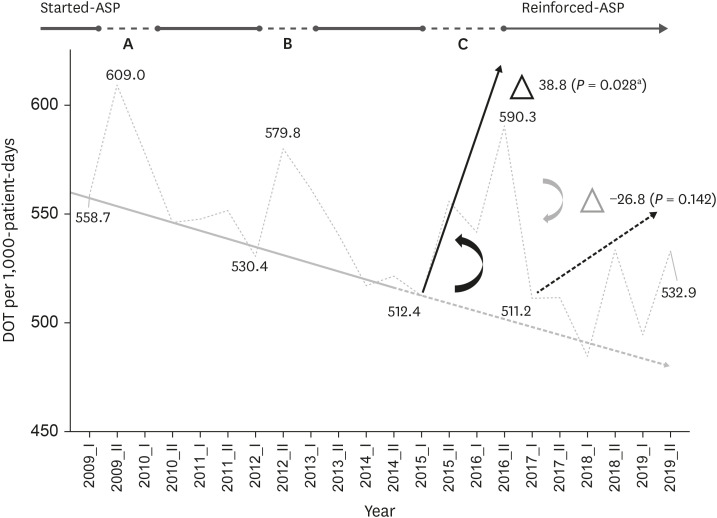
A retrospective single-center study was performed on pediatric inpatients under 19 years old who received systemic antimicrobial treatment from 2001 to 2019. A pediatric infectious disease attending physician started ASP in January 2008. The study period was divided into the pre-intervention (2001–2008) and the post-intervention (2009–2019) periods. The amount of antimicrobial use was defined as days of therapy per 1,000 patientdays, and the differences were compared using delta slope (= changes in slopes) between the two study periods by an interrupted time-series analysis. The proportion of resistant pathogens and the 30-day overall mortality rate were analyzed by the χ2 .
Results
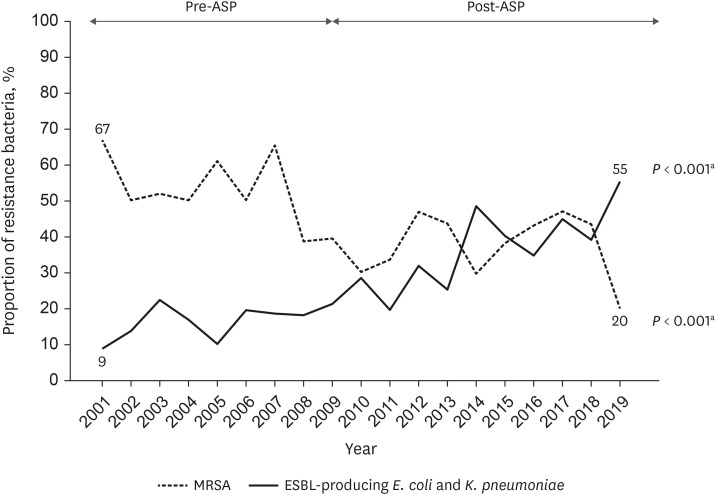
The proportion of extended-spectrum beta-lactamase (ESBL)-producing Escherichia coli and Klebsiella pneumoniae bacteremia increased from 17% (39 of 235) in the pre-intervention period to 35% (189 of 533) in the post-intervention period (P < 0.001). The total amount of antimicrobial use significantly decreased after the introduction of ASP (delta slope value = −16.5; 95% confidence interval [CI], −30.6 to −2.3; P = 0.049). The 30-day overall mortality rate in patients with bacteremia did not increase, being 10% (55 of 564) in the pre-intervention and 10% (94 of 941) in the post-intervention period (P = 0.881).
Conclusion
The introduction of ASP for pediatric patients reduced the delta slope of the total antimicrobial use without increasing the mortality rate despite an increased incidence of ESBL-producing gram-negative bacteremia.
Keyword
Figure
Reference
-
1. Fishman N. Society for Healthcare Epidemiology of America. Infectious Diseases Society of America. Pediatric Infectious Diseases Society. Policy statement on antimicrobial stewardship by the Society for Healthcare Epidemiology of America (SHEA), the Infectious Diseases Society of America (IDSA), and the Pediatric Infectious Diseases Society (PIDS). Infect Control Hosp Epidemiol. 2012; 33(4):322–327. PMID: 22418625.2. Llor C, Bjerrum L. Antimicrobial resistance: risk associated with antibiotic overuse and initiatives to reduce the problem. Ther Adv Drug Saf. 2014; 5(6):229–241. PMID: 25436105.3. Kolár M, Urbánek K, Látal T. Antibiotic selective pressure and development of bacterial resistance. Int J Antimicrob Agents. 2001; 17(5):357–363. PMID: 11337221.4. Friedman ND, Temkin E, Carmeli Y. The negative impact of antibiotic resistance. Clin Microbiol Infect. 2016; 22(5):416–422. PMID: 26706614.5. Naylor NR, Pouwels KB, Hope R, Green N, Henderson KL, Knight GM, et al. The health and cost burden of antibiotic resistant and susceptible Escherichia coli bacteraemia in the English hospital setting: a national retrospective cohort study. PLoS One. 2019; 14(9):e0221944. PMID: 31504046.6. Thorpe KE, Joski P, Johnston KJ. Antibiotic-resistant infection treatment costs have doubled since 2002, now exceeding $2 billion annually. Health Aff (Millwood). 2018; 37(4):662–669. PMID: 29561692.7. Cosgrove SE. The relationship between antimicrobial resistance and patient outcomes: mortality, length of hospital stay, and health care costs. Clin Infect Dis. 2006; 42(Suppl 2):S82–S89. PMID: 16355321.8. Barlam TF, Cosgrove SE, Abbo LM, MacDougall C, Schuetz AN, Septimus EJ, et al. Implementing an antibiotic stewardship program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis. 2016; 62(10):e51–e77. PMID: 27080992.9. Yoon YK, Kwon KT, Jeong SJ, Moon C, Kim B, Kiem S, et al. Guidelines on implementing antimicrobial stewardship programs in Korea. Infect Chemother. 2021; 53(3):617–659. PMID: 34623784.10. Cheong HS, Park KH, Kim HB, Kim SW, Kim B, Moon C, et al. Core elements for implementing antimicrobial stewardship programs in Korean general hospitals. Infect Chemother. 2022; 54(4):637–673. PMID: 36596679.11. Shin SM, Shin JY, Kim MH, Lee SH, Choi S, Park BJ. Prevalence of antibiotic use for pediatric acute upper respiratory tract infections in Korea. J Korean Med Sci. 2015; 30(5):617–624. PMID: 25931794.12. Choe YJ, Shin JY. Trends in the use of antibiotics among Korean children. Korean J Pediatr. 2019; 62(4):113–118. PMID: 30852884.13. Song SY, Shin JH, Hyeon SY, Kim D, Kang WK, Choi SH, et al. Pediatric fluoroquinolone prescription in South Korea before and after a regulatory intervention: a nationwide study, 2007-2015. PLoS One. 2017; 12(5):e0176420. PMID: 28520738.14. Huh K, Chung DR, Park HJ, Kim MJ, Lee NY, Ha YE, et al. Impact of monitoring surgical prophylactic antibiotics and a computerized decision support system on antimicrobial use and antimicrobial resistance. Am J Infect Control. 2016; 44(9):e145–e152. PMID: 26975714.15. Hwang H, Kim B. Impact of an infectious diseases specialist-led antimicrobial stewardship programmes on antibiotic use and antimicrobial resistance in a large Korean hospital. Sci Rep. 2018; 8(1):14757. PMID: 30283084.16. Jang W, Hwang H, Jo HU, Cha YH, Kim B. Effect of discontinuation of an antimicrobial stewardship programme on the antibiotic usage pattern. Clin Microbiol Infect. 2021; 27(12):1860.e1–1860.e5.17. Kim SH, Yoon JG, Park HJ, Won H, Ryoo SS, Choi E, et al. Effects of a comprehensive antimicrobial stewardship program in a surgical intensive care unit. Int J Infect Dis. 2021; 108:237–243. PMID: 33639294.18. Araujo da Silva AR, Albernaz de Almeida Dias DC, Marques AF, Biscaia di Biase C, Murni IK, Dramowski A, et al. Role of antimicrobial stewardship programmes in children: a systematic review. J Hosp Infect. 2018; 99(2):117–123. PMID: 28807835.19. Turner RB, Valcarlos E, Loeffler AM, Gilbert M, Chan D. Impact of an antimicrobial stewardship program on antibiotic use at a nonfreestanding children’s hospital. J Pediatric Infect Dis Soc. 2017; 6(3):e36–e40. PMID: 28903514.20. Hersh AL, De Lurgio SA, Thurm C, Lee BR, Weissman SJ, Courter JD, et al. Antimicrobial stewardship programs in freestanding children’s hospitals. Pediatrics. 2015; 135(1):33–39. PMID: 25489018.21. Nzegwu NI, Rychalsky MR, Nallu LA, Song X, Deng Y, Natusch AM, et al. Implementation of an antimicrobial stewardship program in a neonatal intensive care unit. Infect Control Hosp Epidemiol. 2017; 38(10):1137–1143. PMID: 28745260.22. Aizawa Y, Suwa J, Higuchi H, Fukuoka K, Furuichi M, Kaneko T, et al. Antimicrobial stewardship program in a pediatric intensive care unit. J Pediatric Infect Dis Soc. 2018; 7(3):e156–e159. PMID: 29688433.23. Klatte JM, Kopcza K, Knee A, Horton ER, Housman E, Fisher DJ. Implementation and impact of an antimicrobial stewardship program at a non-freestanding children’s hospital. J Pediatr Pharmacol Ther. 2018; 23(2):84–91. PMID: 29720908.24. Velasco-Arnaiz E, Simó-Nebot S, Ríos-Barnés M, López Ramos MG, Monsonís M, Urrea-Ayala M, et al. Benefits of a pediatric antimicrobial stewardship program in antimicrobial use and quality of prescriptions in a referral children’s hospital. J Pediatr. 2020; 225:222–230.e1. PMID: 32522527.25. Shishido A, Otake S, Kimura M, Tsuzuki S, Fukuda A, Ishida A, et al. Effects of a nudge-based antimicrobial stewardship program in a pediatric primary emergency medical center. Eur J Pediatr. 2021; 180(6):1933–1940. PMID: 33558964.26. Wattier RL, Levy ER, Sabnis AJ, Dvorak CC, Auerbach AD. Reducing second gram-negative antibiotic therapy on pediatric oncology and hematopoietic stem cell transplantation services. Infect Control Hosp Epidemiol. 2017; 38(9):1039–1047. PMID: 28758610.27. Horikoshi Y, Suwa J, Higuchi H, Kaneko T, Furuichi M, Aizawa Y, et al. Sustained pediatric antimicrobial stewardship program with consultation to infectious diseases reduced carbapenem resistance and infection-related mortality. Int J Infect Dis. 2017; 64:69–73. PMID: 28941633.28. Donà D, Barbieri E, Daverio M, Lundin R, Giaquinto C, Zaoutis T, et al. Correction to: implementation and impact of pediatric antimicrobial stewardship programs: a systematic scoping review. Antimicrob Resist Infect Control. 2020; 9(1):59. PMID: 32381059.29. Stultz JS, Arnold SR, Shelton CM, Bagga B, Lee KR. Antimicrobial stewardship impact on Pseudomonas aeruginosa susceptibility to meropenem at a tertiary pediatric institution. Am J Infect Control. 2019; 47(12):1513–1515. PMID: 31253550.30. Polk RE, Fox C, Mahoney A, Letcavage J, MacDougall C. Measurement of adult antibacterial drug use in 130 US hospitals: comparison of defined daily dose and days of therapy. Clin Infect Dis. 2007; 44(5):664–670. PMID: 17278056.31. Ramsay C, Brown E, Hartman G, Davey P. Room for improvement: a systematic review of the quality of evaluations of interventions to improve hospital antibiotic prescribing. J Antimicrob Chemother. 2003; 52(5):764–771. PMID: 14563901.32. Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017; 46(1):348–355. PMID: 27283160.33. Turner SL, Karahalios A, Forbes AB, Taljaard M, Grimshaw JM, McKenzie JE. Comparison of six statistical methods for interrupted time series studies: empirical evaluation of 190 published series. BMC Med Res Methodol. 2021; 21(1):134. PMID: 34174809.34. Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002; 27(4):299–309. PMID: 12174032.35. Centers for Disease Control and Prevention, National Center for Immunization and Respiratory Diseases (NCIRD). 2009 H1N1 Pandemic (H1N1pdm09 virus). Updated 2019. Accessed March 1, 2023. https://archive.cdc.gov/#/details?url=https://www.cdc.gov/flu/pandemic-resources/2009-h1n1-pandemic.html .36. Cho SY, Kang JM, Ha YE, Park GE, Lee JY, Ko JH, et al. MERS-CoV outbreak following a single patient exposure in an emergency room in South Korea: an epidemiological outbreak study. Lancet. 2016; 388(10048):994–1001. PMID: 27402381.37. Lee J, Pai H, Kim YK, Kim NH, Eun BW, Kang HJ, et al. Control of extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae in a children’s hospital by changing antimicrobial agent usage policy. J Antimicrob Chemother. 2007; 60(3):629–637. PMID: 17599919.38. Viale P, Tumietto F, Giannella M, Bartoletti M, Tedeschi S, Ambretti S, et al. Impact of a hospital-wide multifaceted programme for reducing carbapenem-resistant Enterobacteriaceae infections in a large teaching hospital in northern Italy. Clin Microbiol Infect. 2015; 21(3):242–247. PMID: 25658534.39. Horikoshi Y, Higuchi H, Suwa J, Isogai M, Shoji T, Ito K. Impact of computerized pre-authorization of broad spectrum antibiotics in Pseudomonas aeruginosa at a children’s hospital in Japan. J Infect Chemother. 2016; 22(8):532–535. PMID: 27263807.40. Chang MS, Sung KW, Kim YJ. Clinical characteristics of bacteremia in children with cancer. Korean J Pediatr Infect Dis. 2011; 18(2):201–206.41. Lee NH, Kang JM, Lee JW, Huh HJ, Lee NY, Yoo KH, et al. Cefepime versus cefepime plus amikacin as an initial antibiotic choice for pediatric cancer patients with febrile neutropenia in an era of increasing cefepime resistance. Pediatr Infect Dis J. 2020; 39(10):931–936. PMID: 32453199.42. Lee MJ, Moon SM, Kim B, Park SY, Park JY, Koo H, et al. Status of antimicrobial stewardship programmes in Korean hospitals including small to medium-sized hospitals and the awareness and demands of physicians: a nationwide survey in 2020. J Glob Antimicrob Resist. 2021; 26:180–187. PMID: 34153526.43. Kim B, Eun BW, Lee E, Kim TH, Park S, Park SY. Professional status of infectious disease specialists in Korea: a nationwide survey. J Korean Med Sci. 2022; 37(47):e320. PMID: 36472083.44. Ashiru-Oredope D, Kerr F, Hughes S, Urch J, Lanzman M, Yau T, et al. Assessing the impact of COVID-19 on antimicrobial stewardship activities/programs in the United Kingdom. Antibiotics (Basel). 2021; 10(2):110. PMID: 33498716.45. Comelli A, Genovese C, Lombardi A, Bobbio C, Scudeller L, Restelli U, et al. What is the impact of SARS-CoV-2 pandemic on antimicrobial stewardship programs (ASPs)? The results of a survey among a regional network of infectious disease centres. Antimicrob Resist Infect Control. 2022; 11(1):108. PMID: 36038903.46. Langford BJ, So M, Raybardhan S, Leung V, Westwood D, MacFadden DR, et al. Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Clin Microbiol Infect. 2020; 26(12):1622–1629. PMID: 32711058.47. Alshaikh FS, Godman B, Sindi ON, Seaton RA, Kurdi A. Prevalence of bacterial coinfection and patterns of antibiotics prescribing in patients with COVID-19: a systematic review and meta-analysis. PLoS One. 2022; 17(8):e0272375. PMID: 35913964.48. Abelenda-Alonso G, Padullés A, Rombauts A, Gudiol C, Pujol M, Alvarez-Pouso C, et al. Antibiotic prescription during the COVID-19 pandemic: a biphasic pattern. Infect Control Hosp Epidemiol. 2020; 41(11):1371–1372. PMID: 32729437.49. CDC. Core Elements of Hospital Antibiotic Stewardship Programs. Atlanta, GA, USA: US Department of Health and Human Services, CDC;2019.50. Liu C, Yoon EJ, Kim D, Shin JH, Shin JH, Shin KS, et al. Antimicrobial resistance in South Korea: a report from the Korean global antimicrobial resistance surveillance system (Kor-GLASS) for 2017. J Infect Chemother. 2019; 25(11):845–859. PMID: 31311694.51. Kaier K, Meyer E, Dettenkofer M, Frank U. Epidemiology meets econometrics: using time-series analysis to observe the impact of bed occupancy rates on the spread of multidrug-resistant bacteria. J Hosp Infect. 2010; 76(2):108–113. PMID: 20599296.52. Kim D, Lee H, Choi JS, Croney CM, Park KS, Park HJ, et al. The changes in epidemiology of imipenem-resistant Acinetobacter baumannii bacteremia in a pediatric intensive care unit for 17 years. J Korean Med Sci. 2022; 37(24):e196. PMID: 35726147.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antimicrobial Therapy and Antimicrobial Stewardship in Sepsis
- Improving Causal Inference in Observational Studies: Interrupted Time Series Design
- Optimal antimicrobial therapy and antimicrobial stewardship in sepsis and septic shock
- Antimicrobial Therapy and Antimicrobial Stewardship in Urosepsis
- Antimicrobial Consumption as a Key Component of Antimicrobial Stewardship Programs: a Meaningful Movement toward Evidence-based Antimicrobial Stewardship of Validated Outcome Measures