J Korean Med Sci.
2024 May;39(20):e169. 10.3346/jkms.2024.39.e169.
Exploring Disparities for Obesity in Korea Using Hierarchical Age-PeriodCohort Analysis With Cross-Classified Random Effect Models
- Affiliations
-
- 1Division of Cancer Early Detection, National Cancer Control Institute, National Cancer Center, Goyang, Korea
- 2Cardio-Cerebrovascular Center, Chonnam National University Hospital, Gwangju, Korea
- 3Department of Preventive Medicine, Chonnam National University Medical School, Hwasun, Korea
- KMID: 2556286
- DOI: http://doi.org/10.3346/jkms.2024.39.e169
Abstract
- Background
This research article investigates the age, period, and birth cohort effects on prevalence of obesity in the Korean population, with the goal of identifying key factors to inform effective public health strategies.
Methods
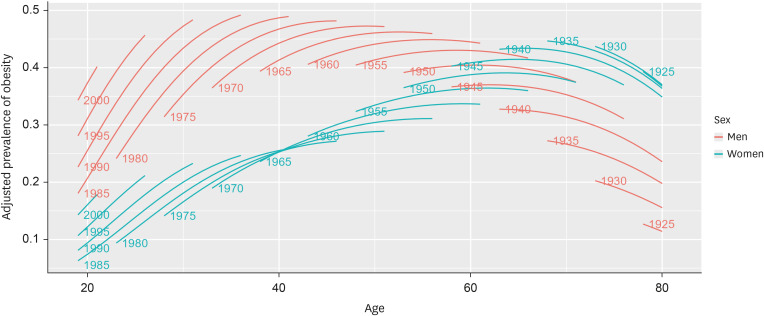
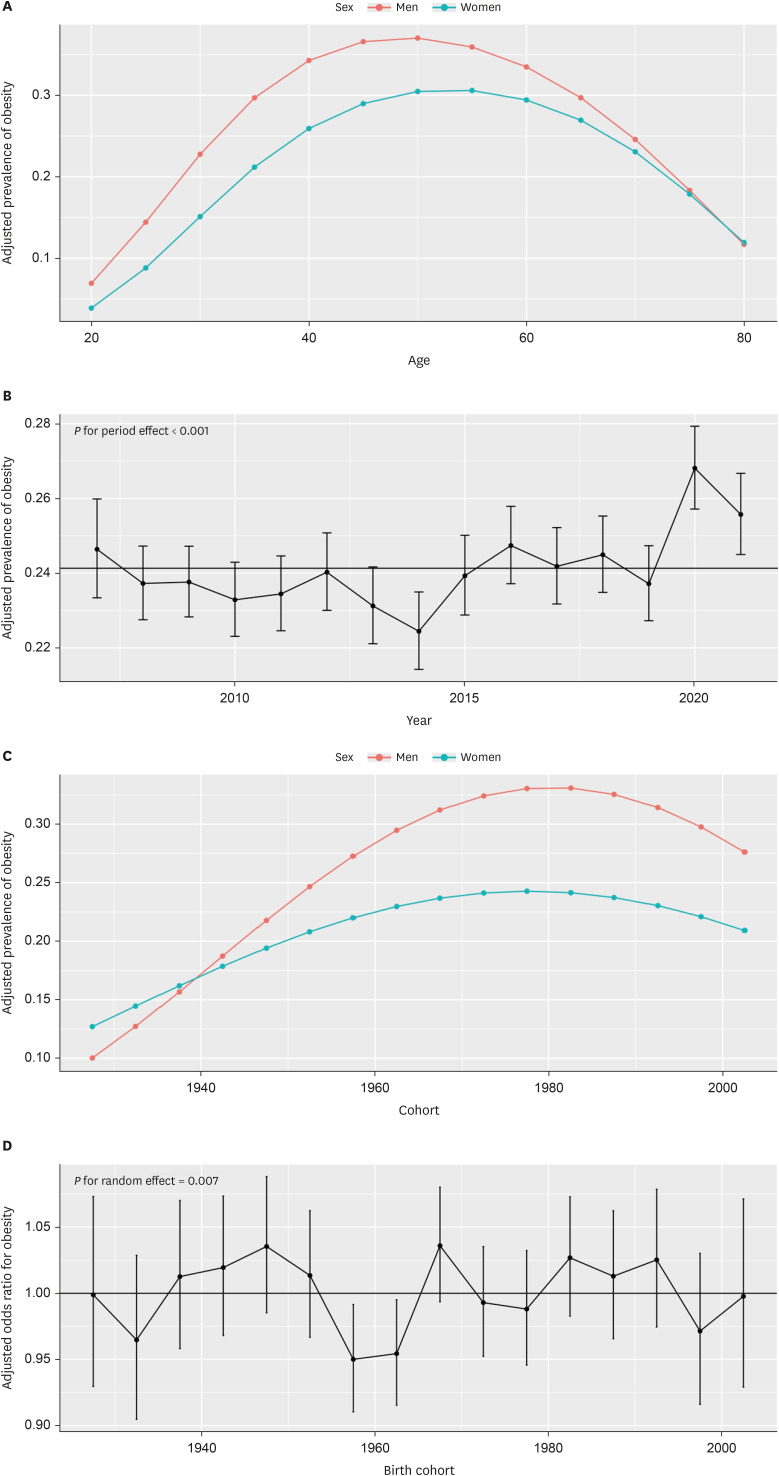
We analyzed data from the Korea National Health and Nutrition Examination Survey, spanning 2007–2021, including 35,736 men and 46,756 women. Using the hierarchical age-period-cohort (APC) analysis with cross-classified random effects modeling, we applied multivariable mixed logistic regression to estimate the marginal prevalence of obesity across age, period, and birth cohort, while assessing the interaction between APC and lifestyle and socioeconomic factors.
Results
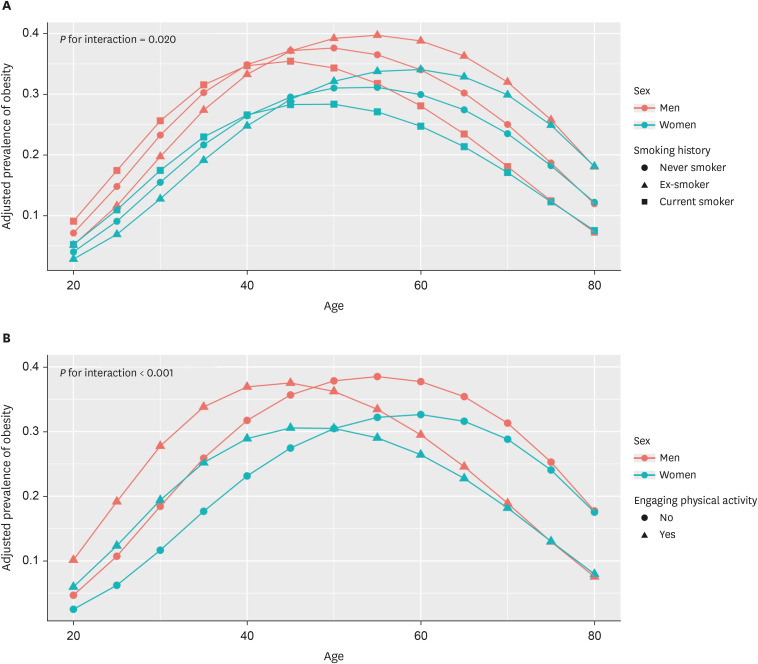
Our findings reveal an inverted U-shaped age effect on obesity, influenced by smoking history (P for interaction = 0.020) and physical activity (I for interaction < 0.001). The period effect was positive in 2020 and 2021, while negative in 2014 (P for period effect < 0.001). A declining trend in obesity prevalence was observed in birth cohorts from 1980s onward. Notably, disparities in obesity rates among recent birth cohorts have increased in relation to smoking history (P for interaction = 0.020), physical activity (P for interaction < 0.001), and residence (P for interaction = 0.005). Particularly, those born after 1960 were more likely to be obese if they were ex-smokers, physical inactive, or lived in rural areas.
Conclusion
These findings highlight growing disparities in obesity within birth cohorts, underscoring the need for targeted health policies that promote smoking cessation and physical activity, especially in rural areas.
Keyword
Figure
Reference
-
1. Chong B, Jayabaskaran J, Kong G, Chan YH, Chin YH, Goh R, et al. Trends and predictions of malnutrition and obesity in 204 countries and territories: an analysis of the Global Burden of Disease Study 2019. EClinicalMedicine. 2023; 57:101850. PMID: 36864983.2. Yang YS, Han BD, Han K, Jung JH, Son JW. Taskforce Team of the Obesity Fact Sheet of the Korean Society for the Study of Obesity. Obesity fact sheet in Korea, 2021: trends in obesity prevalence and obesity-related comorbidity incidence stratified by age from 2009 to 2019. J Obes Metab Syndr. 2022; 31(2):169–177. PMID: 35770450.3. Bell A. Life-course and cohort trajectories of mental health in the UK, 1991-2008--a multilevel age-period-cohort analysis. Soc Sci Med. 2014; 120(120):21–30. PMID: 25215933.4. Keyes KM, Utz RL, Robinson W, Li G. What is a cohort effect? Comparison of three statistical methods for modeling cohort effects in obesity prevalence in the United States, 1971-2006. Soc Sci Med. 2010; 70(7):1100–1108. PMID: 20122771.5. Kwon JW, Song YM, Park H, Sung J, Kim H, Cho SI. Effects of age, time period, and birth cohort on the prevalence of diabetes and obesity in Korean men. Diabetes Care. 2008; 31(2):255–260. PMID: 17977938.6. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004; 363(9403):157–163. PMID: 14726171.7. Yang Y, Kelifa MO, Yu B, Herbert C, Wang Y, Jiang J. Gender-specific temporal trends in overweight prevalence among Chinese adults: a hierarchical age-period-cohort analysis from 2008 to 2015. Glob Health Res Policy. 2020; 5(1):42. PMID: 32944654.8. Okui T. An age-period-cohort analysis of biomarkers of lifestyle-related diseases using the National Health and Nutrition Survey in Japan, 1973-2018. Int J Environ Res Public Health. 2020; 17(21):8159. PMID: 33158284.9. Oh K, Kim Y, Kweon S, Kim S, Yun S, Park S, et al. Korea National Health and Nutrition Examination Survey, 20th anniversary: accomplishments and future directions. Epidemiol Health. 2021; 43:e2021025. PMID: 33872484.10. Bell A, Jones K. Explaining fixed effects: random effects modeling of time-series cross-sectional and panel data. Polit Sci Res Methods. 2015; 3(1):133–153.11. Bates D, Mächler M, Bolker BM, Walker SC. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015; 67(1):1–48.12. Befort CA, Nazir N, Perri MG. Prevalence of obesity among adults from rural and urban areas of the United States: findings from NHANES (2005-2008). J Rural Health. 2012; 28(4):392–397. PMID: 23083085.13. Peytremann-Bridevaux I, Faeh D, Santos-Eggimann B. Prevalence of overweight and obesity in rural and urban settings of 10 European countries. Prev Med. 2007; 44(5):442–446. PMID: 17258803.14. Angkurawaranon C, Jiraporncharoen W, Chenthanakij B, Doyle P, Nitsch D. Urban environments and obesity in southeast Asia: a systematic review, meta-analysis and meta-regression. PLoS One. 2014; 9(11):e113547. PMID: 25426942.15. NCD Risk Factor Collaboration (NCD-RisC). Rising rural body-mass index is the main driver of the global obesity epidemic in adults. Nature. 2019; 569(7755):260–264. PMID: 31068725.16. Cho S, Shin JY, Kim HJ, Eun SJ, Kang S, Jang WM, et al. Chasms in achievement of recommended diabetes care among geographic regions in Korea. J Korean Med Sci. 2019; 34(31):e190. PMID: 31392852.17. Lim SM, Seo SH, Park KS, Hwangbo Y, Suh Y, Ji S, et al. Performance of a community-based noncommunicable disease control program in Korea: patients 65 years of age or older. J Korean Med Sci. 2020; 35(31):e268. PMID: 32776722.18. Kim HS, Suh Y, Kim MS, Yoo BN, Lee EJ, Lee EW, et al. Effects of community-based primary care management on patients with hypertension and diabetes. Asia Pac J Public Health. 2019; 31(6):522–535. PMID: 31523988.19. Beverly EA. Obesity management solutions in rural communities. Curr Cardiovasc Risk Rep. 2024; 18(1):13–23.20. Diouf I, Charles MA, Ducimetière P, Basdevant A, Eschwege E, Heude B. Evolution of obesity prevalence in France: an age-period-cohort analysis. Epidemiology. 2010; 21(3):360–365. PMID: 20375843.21. Ge W, Hu J, Xiao Y, Liang F, Yi L, Zhu R, et al. COVID-19–related childhood BMI increases in China: a health surveillance–based ambispective cohort analysis. Am J Prev Med. 2022; 63(4):647–655. PMID: 35688722.22. Lange SJ, Kompaniyets L, Freedman DS, Kraus EM, Porter R, Blanck HM, et al. Longitudinal trends in body mass index before and during the COVID-19 pandemic among persons aged 2-19 years - United States, 2018-2020. MMWR Morb Mortal Wkly Rep. 2021; 70(37):1278–1283. PMID: 34529635.23. Yamamura E. Impact of the Fukushima nuclear accident on obesity of children in Japan (2008-2014). Econ Hum Biol. 2016; 21:110–121. PMID: 26849534.24. Dor-Haim H, Katzburg S, Revach P, Levine H, Barak S. The impact of COVID-19 lockdown on physical activity and weight gain among active adult population in Israel: a cross-sectional study. BMC Public Health. 2021; 21(1):1521. PMID: 34362319.25. Oh CM, Kim Y, Yang J, Choi S, Oh K. Changes in health behaviors and obesity of Korean adolescents before and during the COVID-19 pandemic: a special report using the Korea Youth Risk Behavior Survey. Epidemiol Health. 2023; 45:e2023018. PMID: 36791796.26. Puccinelli PJ, da Costa TS, Seffrin A, de Lira CA, Vancini RL, Nikolaidis PT, et al. Reduced level of physical activity during COVID-19 pandemic is associated with depression and anxiety levels: an internet-based survey. BMC Public Health. 2021; 21(1):425. PMID: 33648487.27. Kyle TK, Dhurandhar EJ, Allison DB. Regarding obesity as a disease: evolving policies and their implications. Endocrinol Metab Clin North Am. 2016; 45(3):511–520. PMID: 27519127.28. Aubin HJ, Farley A, Lycett D, Lahmek P, Aveyard P. Weight gain in smokers after quitting cigarettes: meta-analysis. BMJ. 2012; 345:e4439. PMID: 22782848.29. Tian J, Venn A, Otahal P, Gall S. The association between quitting smoking and weight gain: a systemic review and meta-analysis of prospective cohort studies: Smoking cessation and weight gain. Obes Rev. 2015; 16(10):883–901. PMID: 26114839.30. Sahle BW, Chen W, Rawal LB, Renzaho AM. Weight gain after smoking cessation and risk of major chronic diseases and mortality. JAMA Netw Open. 2021; 4(4):e217044. PMID: 33904915.31. Veldheer S, Yingst J, Zhu J, Foulds J. Ten-year weight gain in smokers who quit, smokers who continued smoking and never smokers in the United States, NHANES 2003-2012. Int J Obes. 2015; 39(12):1727–1732.32. Bush T, Levine MD, Beebe LA, Cerutti B, Deprey M, McAfee T, et al. Addressing weight gain in smoking cessation treatment: a randomized controlled trial. Am J Health Promot. 2012; 27(2):94–102. PMID: 23113779.33. García-Fernández G, Krotter A, González-Roz A, García-Pérez Á, Secades-Villa R. Effectiveness of including weight management in smoking cessation treatments: a meta-analysis of behavioral interventions. Addict Behav. 2023; 140:107606. PMID: 36642013.34. Mourino N, Pérez-Ríos M, Yolton K, Lanphear BP, Chen A, Buckley JP, et al. Pre- and postnatal exposure to secondhand tobacco smoke and body composition at 12 years: periods of susceptibility. Obesity (Silver Spring). 2022; 30(8):1659–1669. PMID: 35894081.35. Cleven L, Syrjanen JA, Geda YE, Christenson LR, Petersen RC, Vassilaki M, et al. Association between physical activity and longitudinal change in body mass index in middle-aged and older adults. BMC Public Health. 2023; 23(1):202. PMID: 36717834.36. Williams PT, Wood PD. The effects of changing exercise levels on weight and age-related weight gain. Int J Obes. 2006; 30(3):543–551.37. Macek P, Terek-Derszniak M, Biskup M, Krol H, Smok-Kalwat J, Gozdz S, et al. Assessment of age-induced changes in body fat percentage and BMI aided by bayesian modelling: a cross-sectional cohort study in middle-aged and older adults. Clin Interv Aging. 2020; 15:2301–2311. PMID: 33335389.38. Murphy CC, Claire Yang Y, Shaheen NJ, Hofstetter WL, Sandler RS. An age-period-cohort analysis of obesity and incident esophageal adenocarcinoma among white males: age-period-cohort analysis of esophageal adenocarcinoma. Dis Esophagus. 2017; 30(3):1–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Trends and disparities in avoidable, treatable, and preventable mortalities in South Korea, 2001-2020: comparison of capital and non-capital areas
- The unrealized potential: cohort effects and age-period-cohort analysis
- Multilevel Analysis of Socio-Demographic Disparities in Adulthood Obesity Across the United States Geographic Regions
- The effect of missing levels of nesting in multilevel analysis
- Cross-Sectional Study between Anthropometric Obesity Indices and Intraocular Pressure