J Korean Med Sci.
2024 May;39(20):e168. 10.3346/jkms.2024.39.e168.
Future Blood Debt: Projecting Blood Supply and Demand of Korea Based on Subnational Population Projections (2021–2050)
- Affiliations
-
- 1Department of Geography, Graduate School of Korea University, Seoul, Korea
- 2Department of Geography Education, College of Education, Korea University, Seoul, Korea
- 3Institute of Future Land, Korea University, Korea University, Seoul, Korea
- 4Division of Geriatrics, Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 5Department of Sociology and Criminology, Penn State University, University Park, PA, USA
- 6Department of Anthropology, Penn State University, University Park, PA, USA
- 7Corporate R&D Center for Biological Standards and Control, Resources and Innovation Cooperative, Hanam, Korea
- 8Department of Internal Medicine, Hospital Medicine Center, Seoul National University Hospital, Seoul, Korea
- 9Department of Big Data Science, Korea University, Sejong, Korea
- KMID: 2556285
- DOI: http://doi.org/10.3346/jkms.2024.39.e168
Abstract
- Background
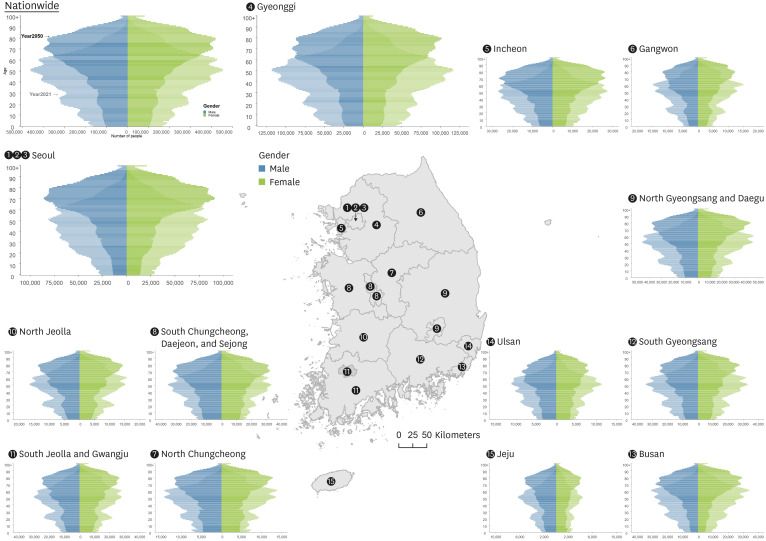
South Korea faces a critical challenge with its rapidly declining fertility rates and an increasingly aging population, which significantly impacts the country's blood supply and demand. Despite these nationwide trends, regional disparities in blood supply and demand have not been thoroughly studied.
Methods
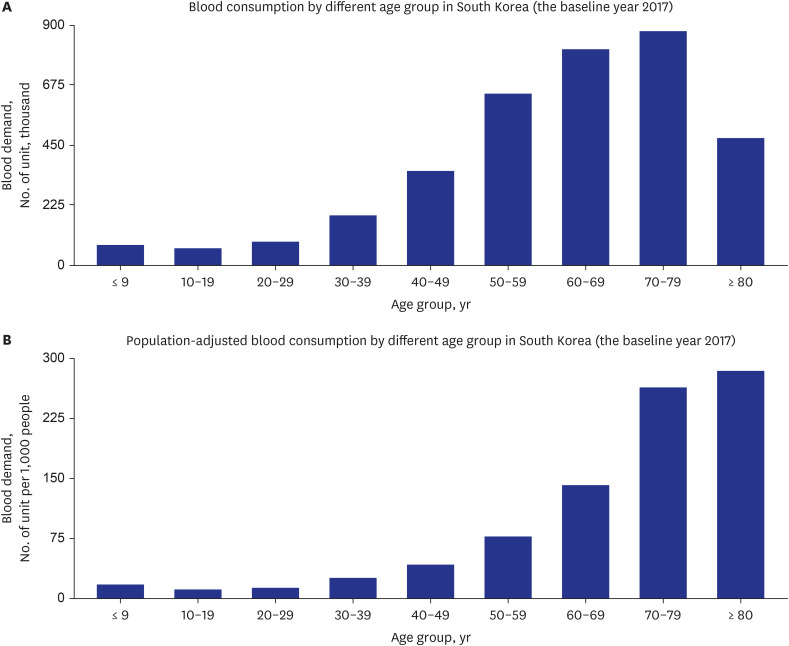
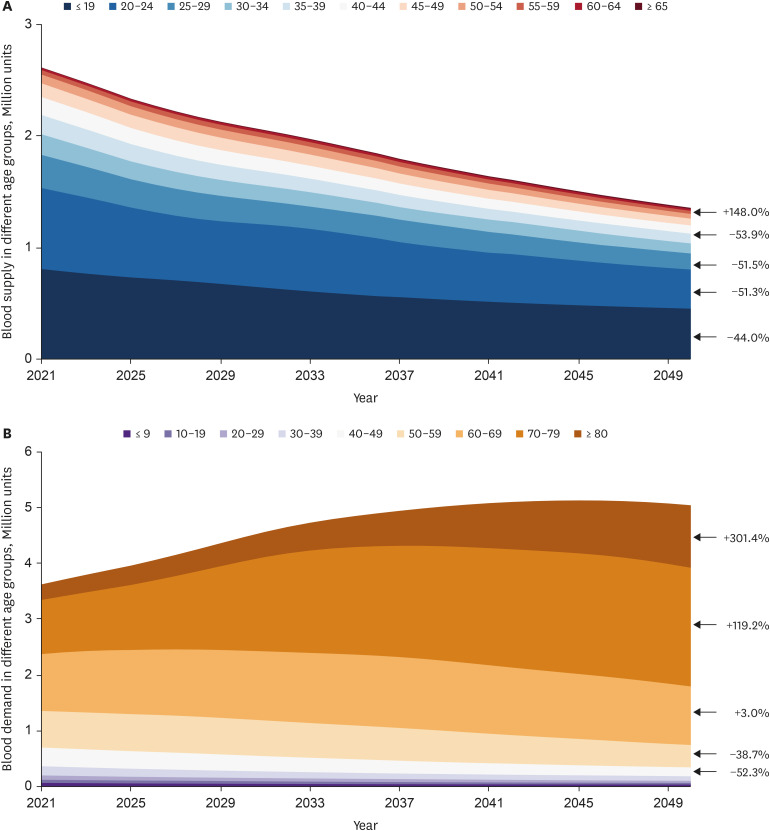
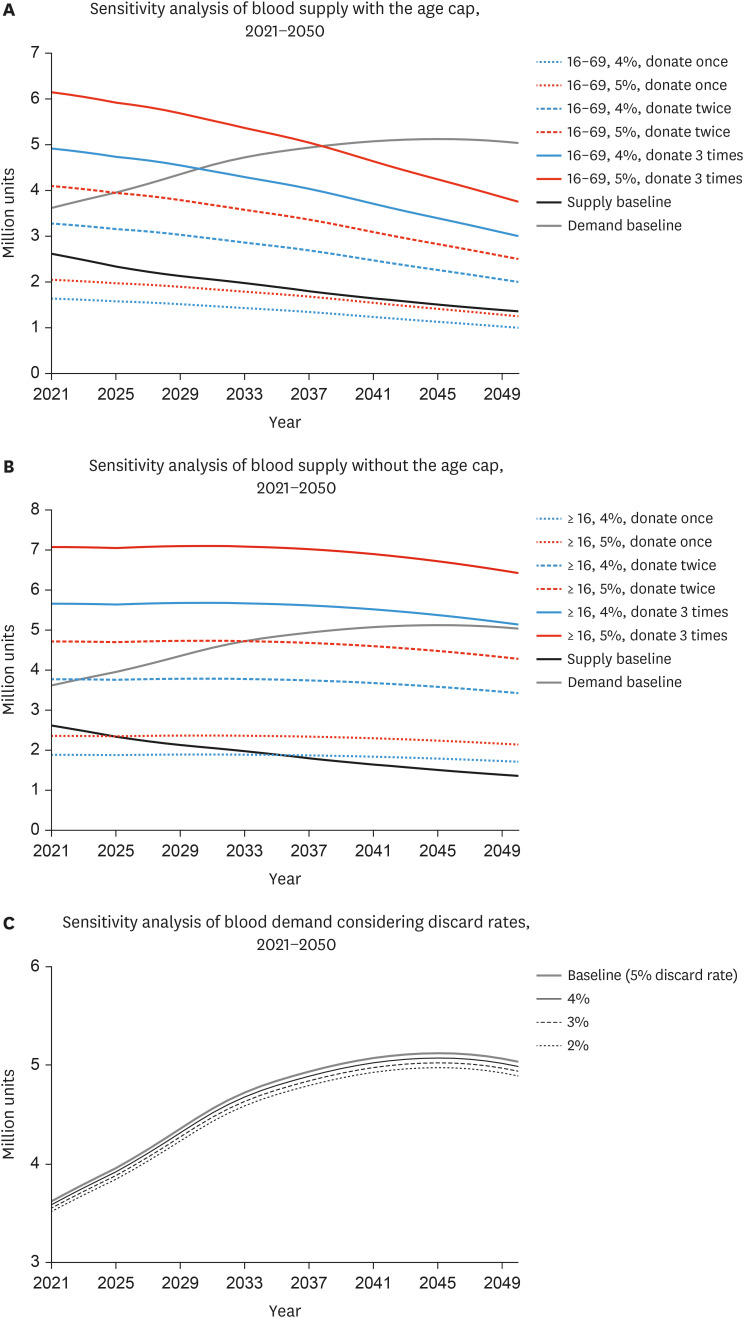
This research utilized blood donation data from the Korean Red Cross and blood transfusion data from the Health Insurance Review and Assessment Service. We analyzed these datasets in conjunction with regional population projections to simulate blood supply and demand from 2021 to 2050 across South Korea. Sensitivity analyses were conducted to assess the impact of various factors, including the number of donors, age eligibility criteria for donations, frequency of donations, and blood discard rates.
Results
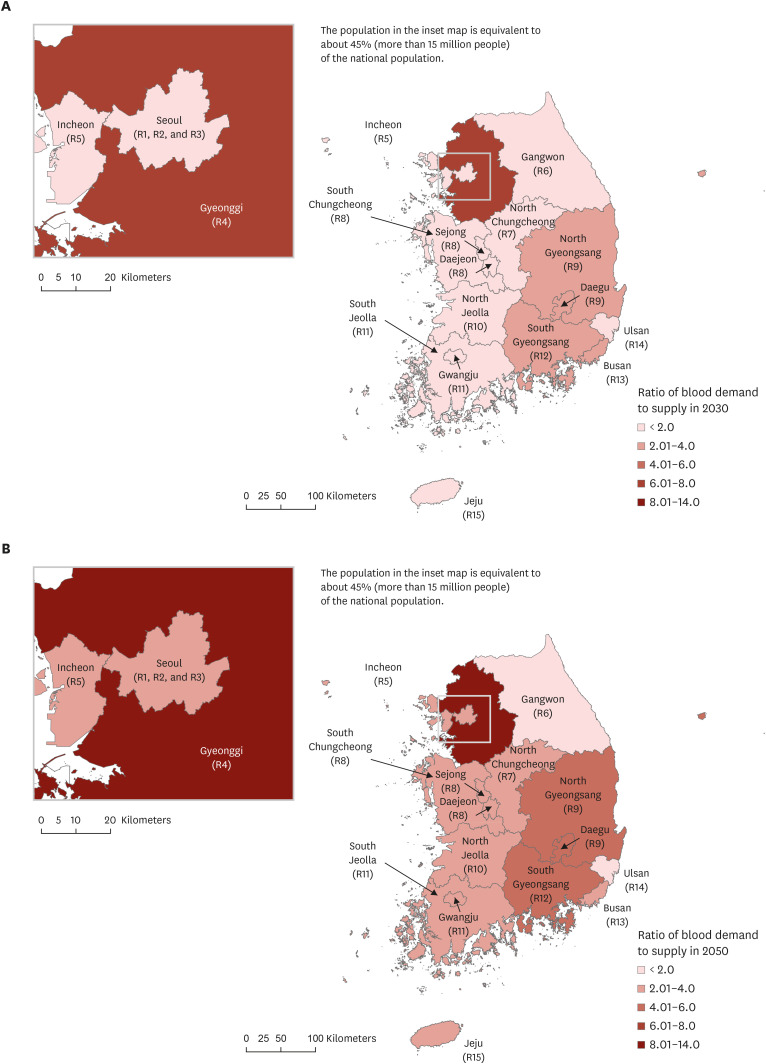
Our projections indicate a decreasing trend in blood supply, from 2.6 million units in 2021 to 1.4 million units by 2050, while demand is expected to peak at 5.1 million units by 2045 before declining. Metropolitan areas, particularly Gyeonggi Province, are projected to experience the most severe shortages. Sensitivity analyses suggest that increasing the donation frequency of existing donors and relaxing age eligibility criteria are more effective strategies in addressing these imbalances than merely increasing the number of new donors. Blood discard rates showed minimal impact on the overall blood shortage.
Conclusion
The findings emphasize the urgent need for targeted strategies to mitigate national and regional blood supply shortages in South Korea. Encouraging frequent donations from experienced donors and broadening eligibility criteria are critical steps toward stabilizing the blood supply amidst demographic shifts. These strategies must be prioritized to address the impending regional disparities in blood availability.
Keyword
Figure
Reference
-
1. Fastag E, Varon J, Sternbach G. Richard Lower: the origins of blood transfusion. J Emerg Med. 2013; 44(6):1146–1150. PMID: 23499352.2. World Health Organization. WHO model list of essential medicines. Updated July 2023. Accessed January 5, 2024. http://www.who.int/medicines/publications/essentialmedicines/en/ .3. Klein HG. Should blood be an essential medicine? N Engl J Med. 2013; 368(3):199–201. PMID: 23323895.4. Dzik WH. Innocent lives lost and saved: the importance of blood transfusion for children in sub-Saharan Africa. BMC Med. 2015; 13(1):22. PMID: 25640864.5. Roberts N, James S, Delaney M, Fitzmaurice C. The global need and availability of blood products: a modelling study. Lancet Haematol. 2019; 6(12):e606–e615. PMID: 31631023.6. Roh J, Choi SJ, Kim S, Min H, Kim HO. Blood supply and demand in Korea: what is in store for the future? Yonsei Med J. 2020; 61(5):400–405. PMID: 32390363.7. Greinacher A, Fendrich K, Brzenska R, Kiefel V, Hoffmann W. Implications of demographics on future blood supply: a population-based cross-sectional study. Transfusion. 2011; 51(4):702–709. PMID: 20849411.8. Greinacher A, Weitmann K, Schönborn L, Alpen U, Gloger D, Stangenberg W, et al. A population-based longitudinal study on the implication of demographic changes on blood donation and transfusion demand. Blood Adv. 2017; 1(14):867–874. PMID: 29296730.9. Goldman M, O’Brien SF. Our older population: donors as well as recipients? ISBT Sci Ser. 2017; 12(4):401–404.10. Drackley A, Newbold KB, Paez A, Heddle N. Forecasting Ontario’s blood supply and demand. Transfusion. 2012; 52(2):366–374. PMID: 21810099.11. Akita T, Tanaka J, Ohisa M, Sugiyama A, Nishida K, Inoue S, et al. Predicting future blood supply and demand in Japan with a Markov model: application to the sex- and age-specific probability of blood donation. Transfusion. 2016; 56(11):2750–2759. PMID: 27595917.12. Jökulsdóttir G. The Impact of Demographics on Future Blood Supply and Demand in Iceland. Reykjavik, Iceland: Reykjavík University;2013. p. 1–83.13. Kasai DT. Preparing for population ageing in the Western Pacific Region. Lancet Reg Health West Pac. 2020; 6:100069. PMID: 34327404.14. Liu WJ, Chen YY, Hsu LI, Chen JW, Wei ST, Hou SM. An imbalance in blood collection and demand is anticipated to occur in the near future in Taiwan. J Formos Med Assoc. 2022; 121(8):1610–1614. PMID: 34407921.15. Volken T, Buser A, Castelli D, Fontana S, Frey BM, Rüsges-Wolter I, et al. Red blood cell use in Switzerland: trends and demographic challenges. Blood Transfus. 2018; 16(1):73–82. PMID: 27723455.16. Ali A, Auvinen MK, Rautonen J. The aging population poses a global challenge for blood services. Transfusion. 2010; 50(3):584–588. PMID: 19912582.17. Yu X, Wang Z, Shen Y, Liu Z, Wang H, Zhang S, et al. Population-based projections of blood supply and demand, China, 2017-2036. Bull World Health Organ. 2020; 98(1):10–18. PMID: 31902958.18. Kim KW, Kim OS. Super aging in South Korea unstoppable but mitigatable: a sub-national scale population projection for best policy planning. Spat Demogr. 2020; 8(2):155–173. PMID: 34222615.19. Kontis V, Bennett JE, Mathers CD, Li G, Foreman K, Ezzati M. Future life expectancy in 35 industrialised countries: projections with a Bayesian model ensemble. Lancet. 2017; 389(10076):1323–1335. PMID: 28236464.20. Korean Red Cross. Blood donation and blood supply data, 2005-2019. Accessed January 5, 2024. https://stat.kosis.kr/nsieu/view/tree.do?task=branchView&id=445_02*MT_OTITLE&hOrg=445 .21. Health Insurance Review & Assessment Service. Transfusion Demand Data by Year and Age, 2010-2017. Wonju, Korea: Health Insurance Review & Assessment Service;2018.22. Kim OS, Han J, Kim KW, Matthews SA, Shim C. Depopulation, super aging, and extreme heat events in South Korea. Clim Risk Manage. 2022; 38:100456.23. Zeiler T, Lander-Kox J, Eichler H, Alt T, Bux J. The safety of blood donation by elderly blood donors. Vox Sang. 2011; 101(4):313–319. PMID: 21535439.24. Weidmann C, Schneider S, Litaker D, Weck E, Klüter H. A spatial regression analysis of German community characteristics associated with voluntary non-remunerated blood donor rates. Vox Sang. 2012; 102(1):47–54. PMID: 21534984.25. JoongAng Daily. Fewer young people donating blood, more elderly receiving transfusions... red light on blood supply. Updated October 2017. Accessed April 29, 2024. https://www.joongang.co.kr/article/22038936#home .26. Newsis. Low birth rate and lacking blood donation coming within 5 years... Decrease in blood donor population since 2020. Updated October 2017. Accessed January 5, 2024. https://www.newsis.com/pdf/?id=NISX20171023_0000125206 .27. Makizako H, Nishita Y, Jeong S, Otsuka R, Shimada H, Iijima K, et al. Trends in the prevalence of frailty in Japan: a meta-analysis from the Ilsa-J. J Frailty Aging. 2021; 10(3):211–218. PMID: 34105703.28. Wiltbank TB, Giordano GF, Kamel H, Tomasulo P, Custer B. Faint and prefaint reactions in whole-blood donors: an analysis of predonation measurements and their predictive value. Transfusion. 2008; 48(9):1799–1808. PMID: 18482188.29. Eder AF, Dy BA, Kennedy JM, Notari Iv EP, Strupp A, Wissel ME, et al. The American Red Cross donor hemovigilance program: complications of blood donation reported in 2006. Transfusion. 2008; 48(9):1809–1819. PMID: 18631167.30. Callum JL, Waters JH, Shaz BH, Sloan SR, Murphy MF. The AABB recommendations for the Choosing Wisely campaign of the American Board of Internal Medicine. Transfusion. 2014; 54(9):2344–2352. PMID: 25100209.31. Hicks CW, Liu J, Yang WW, DiBrito SR, Johnson DJ, Brito A, et al. A comprehensive Choosing Wisely quality improvement initiative reduces unnecessary transfusions in an Academic Department of Surgery. Am J Surg. 2017; 214(4):571–576. PMID: 28683893.32. Leahy MF, Hofmann A, Towler S, Trentino KM, Burrows SA, Swain SG, et al. Improved outcomes and reduced costs associated with a health-system-wide patient blood management program: a retrospective observational study in four major adult tertiary-care hospitals. Transfusion. 2017; 57(6):1347–1358. PMID: 28150313.33. Sadana D, Pratzer A, Scher LJ, Saag HS, Adler N, Volpicelli FM, et al. Promoting high-value practice by reducing unnecessary transfusions with a patient blood management program. JAMA Intern Med. 2018; 178(1):116–122. PMID: 29159367.34. Bialas C, Moser C, Sims CA. Artificial oxygen carriers and red blood cell substitutes: A historic overview and recent developments toward military and clinical relevance. J Trauma Acute Care Surg. 2019; 87(1S):Suppl 1. S48–S58. PMID: 31246907.35. Wang Y, Han W, Pan L, Wang C, Liu Y, Hu W, et al. Impact of COVID-19 on blood centres in Zhejiang province China. Vox Sang. 2020; 115(6):502–506. PMID: 32347566.36. Korean Statistical Information Service. Donations per population who are eligible to donate decreased in Korea in 2020 (6.63%) from 2019 (7.08%). Updated January 2024. Accessed April 29, 2024. https://stat.kosis.kr/statHtml_host/statHtml.do?orgId=445&tblId=DT_445001_007&dbUser=NSI_IN_445 .
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Appropriate Adjustment according to the Supply and Demand Status and Trend of Doctors
- The Demand and Supply of Nutritionist Workforce in Korea and Policy Recommendations
- Blood Supply and Demand in Korea:What is in Store for the Future?
- Need for Patient Blood Management to Prepare for an Unstable Blood Supply Crisis
- The future prospects of supply and demand for urologists in Korea