Neonatal Med.
2024 May;31(2):38-46. 10.5385/nm.2024.31.2.38.
Quality Improvement Project to Reduce Admission Hypothermia of Preterm Infants Born at Less than 32 Weeks or 1,500 g
- Affiliations
-
- 1Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Cell and Gene Therapy Institute for Future Medicine, Samsung Medical Center, Seoul, Korea
- 3Department of Health Science and Technology, Samsung Advanced Institute for Health Sciences & Technology, Sungkyunkwan University, Seoul, Korea
- KMID: 2556153
- DOI: http://doi.org/10.5385/nm.2024.31.2.38
Abstract
- Purpose
Hypothermia upon admission to the neonatal intensive care unit (NICU) contributes significantly to various neonatal complications, particularly in preterm infants. This study aimed to assess the impact of quality improvement (QI) interventions, including using plastic bags and head caps, and adjusting delivery room temperatures, on improving the admission body temperature and reducing hypothermia in infants born at less than 32 weeks or weighing 1,500 g.
Methods
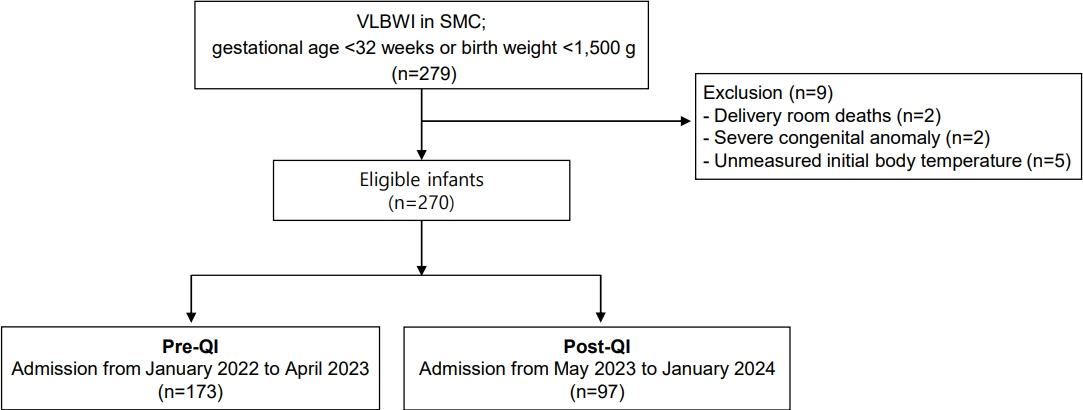
This study retrospectively analyzed the medical records of infants born at less than 32 weeks or weighing 1,500 g who admitted to the NICU at Samsung Medical Center from January 2022 to February 2024. The QI program that was initiated in April 2023 focused on managing admission temperatures using plastic bags and head caps, and maintaining delivery room temperatures at ≥25 °C. The admission temperature and short-term outcomes pre- and post-QI were compared.
Results
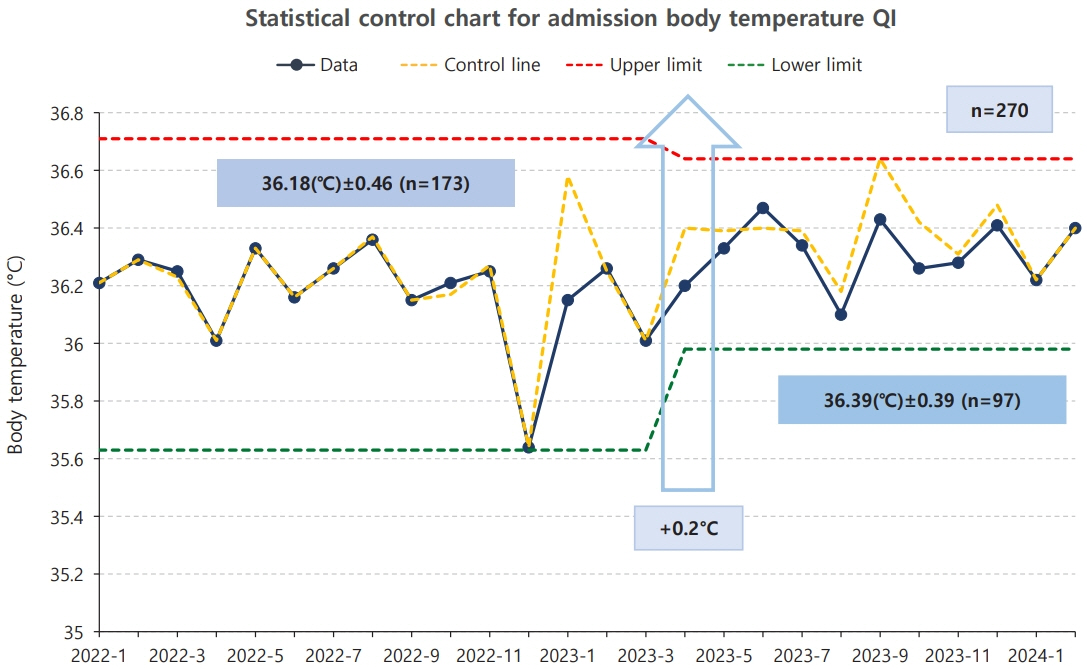
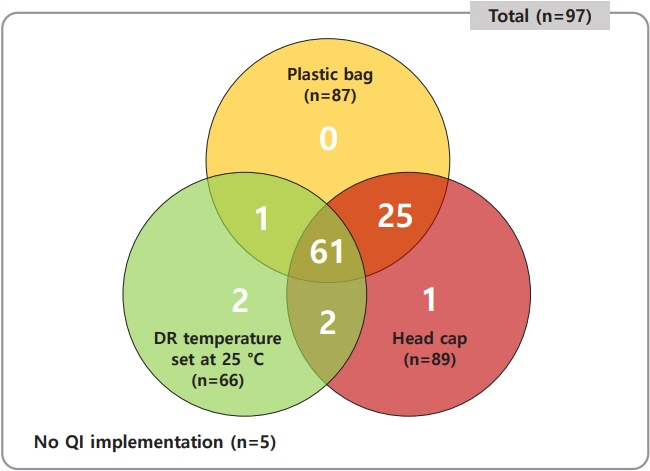
In a study of 270 patients, implementing QI initiatives significantly raised the admission temperature from 36.2±0.5 to 36.4±0.4 °C (p<0.01), particularly impacting infants weighing ≥1,000 g, in whom mild hypothermia occurrences dropped from 76.3% to 43.9% (p<0.01). This improvement in temperature management significantly decreased both mild and severe hypothermia rates post-QI. Additionally, implementing all three initiatives was more effective than when two or fewer initiatives were implemented.
Conclusion
Simple and cost-effective QI interventions can increase admission temperatures and decrease hypothermia in neonates. Further research is essential to explore the long-term outcomes and develop effective hypothermia management strategies in neonatal care.
Keyword
Figure
Reference
-
1. Dixon KL, Carter B, Harriman T, Doles B, Sitton B, Thompson J. Neonatal thermoregulation: a golden hour protocol update. Adv Neonatal Care. 2021; 21:280–8.2. Uxa F. Thermal control of the newborn. Kangaroo. 1994; 3:67–8.3. Lunze K, Hamer DH. Thermal protection of the newborn in resource-limited environments. J Perinatol. 2012; 32:317–24.
Article4. Guillen U, Weiss EM, Munson D, Maton P, Jefferies A, Norman M, et al. Guidelines for the management of extremely premature deliveries: a systematic review. Pediatrics. 2015; 136:343–50.
Article5. de Almeida MF, Guinsburg R, Sancho GA, Rosa IR, Lamy ZC, Martinez FE, et al. Hypothermia and early neonatal mortality in preterm infants. J Pediatr. 2014; 164:271–5.
Article6. Miller SS, Lee HC, Gould JB. Hypothermia in very low birth weight infants: distribution, risk factors and outcomes. J Perinatol. 2011; 31 Suppl 1:S49–56.
Article7. Laptook A, Jackson GL. Cold stress and hypoglycemia in the late preterm (“near-term”) infant: impact on nursery of admission. Semin Perinatol. 2006; 30:24–7.
Article8. Lunze K, Bloom DE, Jamison DT, Hamer DH. The global burden of neonatal hypothermia: systematic review of a major challenge for newborn survival. BMC Med. 2013; 11:24.
Article9. Ting JY, Synnes AR, Lee SK, Shah PS; Canadian Neonatal Network and Canadian Neonatal Follow-Up Network. Association of admission temperature and death or adverse neurodevelopmental outcomes in extremely low-gestational age neonates. J Perinatol. 2018; 38:844–9.
Article10. Sprecher A, Malin K, Finley D, Lembke P, Keller S, Grippe A, et al. Quality improvement approach to reducing admission hypothermia among preterm and term infants. Hosp Pediatr. 2021; 11:270–6.
Article11. Singh TS, Skelton H, Baird J, Padernia AM, Maheshwari R, Shah DM, et al. Improvement in thermoregulation outcomes following the implementation of a thermoregulation bundle for preterm infants. J Paediatr Child Health. 2022; 58:1201–8.
Article12. Cavallin F, Doglioni N, Allodi A, Battajon N, Vedovato S, Capasso L, et al. Thermal management with and without servo-controlled system in preterm infants immediately after birth: a multicentre, randomised controlled study. Arch Dis Child Fetal Neonatal Ed. 2021; 106:572–7.
Article13. Kumar V, Shearer JC, Kumar A, Darmstadt GL. Neonatal hypothermia in low resource settings: a review. J Perinatol. 2009; 29:401–12.
Article14. Bi SY, Yu YH, Li C, Xu P, Xu HY, Li JH, et al. A standardized implementation of multicenter quality improvement program of very low birth weight newborns could significantly reduce admission hypothermia and improve outcomes. BMC Pediatr. 2022; 22:281.
Article15. Yip WY, Quek BH, Fong MC, Ong SS, Lim BL, et al. A quality improvement project to reduce hypothermia in preterm infants on admission to the neonatal intensive care unit. Int J Qual Health Care. 2017; 29:922–8.
Article16. Frazer M, Ciarlo A, Hinderer KA, Briere CE. Reducing admission hypothermia in neonates born at less than 32 weeks or 1500 g. Adv Neonatal Care. 2022; 22:99–107.
Article17. Choi HS, Lee SM, Eun H, Park M, Park KI, Namgung R. The impact of a quality improvement effort in reducing admission hypothermia in preterm infants following delivery. Korean J Pediatr. 2018; 61:239–44.
Article18. Sharma A, Davis A, Shekhawat PS. Hypoglycemia in the preterm neonate: etiopathogenesis, diagnosis, management and longterm outcomes. Transl Pediatr. 2017; 6:335–48.
Article19. Wolfsdorf JI. Hyperinsulinemic hypoglycemia of infancy. J Pediatr. 1998; 132:1–3.
Article20. Meyer MP, Owen LS, Te Pas AB. Use of heated humidified gases for early stabilization of preterm infants: a meta-analysis. Front Pediatr. 2018; 6:319.
Article21. Dunne EA, O’Donnell CP, Nakstad B, McCarthy LK; European Society for Paediatric Research (ESPR) Neonatal Resuscitation Section Writing Group. Thermoregulation for very preterm infants in the delivery room: a narrative review. Pediatr Res. 2024; Jan. 22. [Epub]. https://doi.org/10.1038/s41390-023-02902-w.
Article22. Dunne EA, Pellegrino N, Murphy MC, McDonald K, Dowling L, O’Donnell CP, et al. Thermal care for very preterm infants in the delivery room in the era of delayed cord clamping. Arch Dis Child Fetal Neonatal Ed. 2023; 108:204.
Article23. te Pas AB, Lopriore E, Dito I, Morley CJ, Walther FJ. Humidified and heated air during stabilization at birth improves temperature in preterm infants. Pediatrics. 2010; 125:e1427. –32.
Article24. Bhatt DR, Reddy N, Ruiz R, Bustos DV, Peacock T, Dizon RA, et al. Perinatal quality improvement bundle to decrease hypothermia in extremely low birthweight infants with birth weight less than 1000 g: single-center experience over 6 years. J Investig Med. 2020; 68:1256–60.
Article25. Laptook AR, Bell EF, Shankaran S, Boghossian NS, Wyckoff MH, Kandefer S, et al. Admission temperature and associated mortality and morbidity among moderately and extremely preterm infants. J Pediatr. 2018; 192:53–9.26. Wilson E, Maier RF, Norman M, Misselwitz B, Howell EA, Zeitlin J, et al. Admission hypothermia in very preterm infants and neonatal mortality and morbidity. J Pediatr. 2016; 175:61–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The impact of a quality improvement effort in reducing admission hypothermia in preterm infants following delivery
- Risk Factors Associated with Hypothermia Immediately after Birth among Preterm Infants
- Initial Optimal Body Temperature in Preterm Infants
- Epidemiologic Study of Preterm Birth in Chosun University Hospital
- Evaluation of Preterm Delivery between 32(+0)-33(+6) Weeks of Gestation