Neonatal Med.
2024 May;31(2):31-37. 10.5385/nm.2024.31.2.31.
Risk Factors Contributing to Extrauterine Growth Restriction in Very Low Birth Weight Infants
- Affiliations
-
- 1Department of Pediatrics, Ewha Womans University Mokdong Hospital, Seoul, Korea
- 2Department of Pediatrics, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea
- KMID: 2556152
- DOI: http://doi.org/10.5385/nm.2024.31.2.31
Abstract
- Purpose
Despite advances in neonatal care, extrauterine growth restriction (EUGR) remains common in preterm infants. This retrospective single-center study aimed to determine the incidence and risk factors of EUGR in very low birth weight (VLBW) infants.
Methods
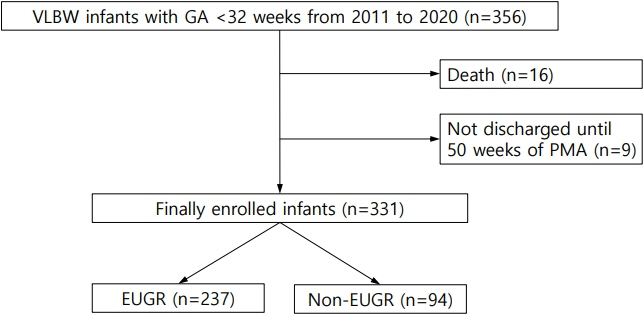
Data were collected concerning VLBW infants with gestational age (GA) <32 weeks between 2011 and 2020. EUGR was defined as a decline in weight z-score >1.2 from birth to discharge, using Fenton growth charts.
Results
Among 331 eligible preterm infants, the prevalence of EUGR at discharge was 71.6%. Infants with EUGR had lower GA and birth weight than those without EUGR. They also underwent prolonged durations of parenteral nutrition, invasive ventilation, and hospitalization. Neonatal morbidities, such as bronchopulmonary dysplasia, patent ductus arteriosus, necrotizing enterocolitis, gastrointestinal surgery, sepsis, and parenteral nutrition-associated cholestasis were more prevalent in the EUGR group. Multivariate analysis identified lower GA and longer time to reach full enteral feeding as independent risk factors, whereas maternal use of antenatal steroids and history of gestational diabetes mellitus were independent protective factors for EUGR.
Conclusion
As VLBW infants are at a high risk of EUGR, continuous attention and efforts to achieve early full enteral nutrition are required to decrease the incidence of EUGR.
Figure
Reference
-
1. Clark RH, Thomas P, Peabody J. Extrauterine growth restriction remains a serious problem in prematurely born neonates. Pediatrics. 2003; 111(5 Pt 1):986–90.
Article2. Horbar JD, Ehrenkranz RA, Badger GJ, Edwards EM, Morrow KA, Soll RF, et al. Weight growth velocity and postnatal growth failure in infants 501 to 1500 grams: 2000-2013. Pediatrics. 2015; 136:e84–92.
Article3. Stevens TP, Shields E, Campbell D, Combs A, Horgan M, La Gamma EF, et al. Statewide initiative to reduce postnatal growth restriction among infants <31 weeks of gestation. J Pediatr. 2018; 197:82–9.
Article4. Avila-Alvarez A, Solar Boga A, Bermudez-Hormigo C, Fuentes Carballal J. Extrauterine growth restriction among neonates with a birthweight less than 1,500 grams. An Pediatr (Engl Ed). 2018; 89:325–32.
Article5. Starc M, Giangreco M, Centomo G, Travan L, Bua J. Extrauterine growth restriction in very low birth weight infants according to different growth charts: a retrospective 10 years observational study. PLoS One. 2023; 18:e0283367.
Article6. Peila C, Spada E, Giuliani F, Maiocco G, Raia M, Cresi F, et al. Extrauterine growth restriction: definitions and predictability of outcomes in a cohort of very low birth weight infants or preterm neonates. Nutrients. 2020; 12:1224.
Article7. Makker K, Ji Y, Hong X, Wang X. Antenatal and neonatal factors contributing to extra uterine growth failure (EUGR) among preterm infants in Boston Birth Cohort (BBC). J Perinatol. 2021; 41:1025–32.
Article8. Lee SM, Kim N, Namgung R, Park M, Park K, Jeon J. Prediction of postnatal growth failure among very low birth weight infants. Sci Rep. 2018; 8:3729.
Article9. Kim YJ, Shin SH, Cho H, Shin SH, Kim SH, Song IG, et al. Extrauterine growth restriction in extremely preterm infants based on the Intergrowth-21st Project Preterm Postnatal Follow-up Study growth charts and the Fenton growth charts. Eur J Pediatr. 2021; 180:817–24.
Article10. Griffin IJ, Tancredi DJ, Bertino E, Lee HC, Profit J. Postnatal growth failure in very low birthweight infants born between 2005 and 2012. Arch Dis Child Fetal Neonatal Ed. 2016; 101:F50–5.
Article11. Lapillonne A, Griffin IJ. Feeding preterm infants today for later metabolic and cardiovascular outcomes. J Pediatr. 2013; 162(3 Suppl):S7–16.12. Ehrenkranz RA, Dusick AM, Vohr BR, Wright LL, Wrage LA, Poole WK. Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics. 2006; 117:1253–61.
Article13. Ruth VA. Extrauterine growth restriction: a review of the literature. Neonatal Netw. 2008; 27:177–84.
Article14. Zozaya C, Diaz C, Saenz de Pipaon M. How should we define postnatal growth restriction in preterm infants? Neonatology. 2018; 114:177–80.
Article15. Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013; 13:59.
Article16. Goldberg DL, Becker PJ, Brigham K, Carlson S, Fleck L, Gollins L, et al. Identifying malnutrition in preterm and neonatal populations: recommended indicators. J Acad Nutr Diet. 2018; 118:1571–82.
Article17. Rohsiswatmo R, Kaban RK, Sjahrulla MA, Hikmahrachim HG, Marsubrin PM, Roeslani RD, et al. Defining postnatal growth failure among preterm infants in Indonesia. Front Nutr. 2023; 10:1101048.
Article18. Wilson DC, Cairns P, Halliday HL, Reid M, McClure G, Dodge JA. Randomised controlled trial of an aggressive nutritional regimen in sick very low birthweight infants. Arch Dis Child Fetal Neonatal Ed. 1997; 77:F4–11.
Article19. Loui A, Tsalikaki E, Maier K, Walch E, Kamarianakis Y, Obladen M. Growth in high risk infants <1500 g birthweight during the first 5 weeks. Early Hum Dev. 2008; 84:645–50.20. Zhang Z, Mei L, Li L, Xiao J, Wu X, Yuan Y. Maternal and neonatal outcomes of twin pregnancies complicated by gestational diabetes mellitus. Endocrine. 2024; 84:388–98.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Clinical Features Based on Different Weight Percentile in Appropriate for Gestational Age Preterm Infants
- Extrauterine Growth Restriction in Very Low Birth Weight Infants
- The impact of nutritional intervention by a nutrition support team on extrauterine growth restriction in very low birth weight infants in Korea: a retrospective cohort study
- Effect of fluid restriction on postnatal weight and outcome in very low birth weight infants
- Failure to Thrive of Very Low Birth Weight Infants up to Corrected 18 Months of Age