Neonatal Med.
2024 May;31(2):17-23. 10.5385/nm.2024.31.2.17.
Clinical Characteristics of Hypospadias and Its Association with Very Low Birth Weight Infants with Small for Gestational Age
- Affiliations
-
- 1Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2The Research Center for Future Medicine, Samsung Medical Center, Seoul, Korea
- KMID: 2556150
- DOI: http://doi.org/10.5385/nm.2024.31.2.17
Abstract
- Purpose
To investigate the risk factors associated with hypospadias in very low birth weight (VLBW) infants (VLBWIs).
Methods
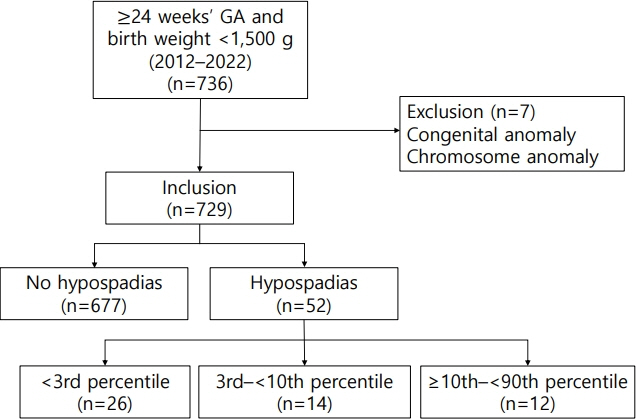
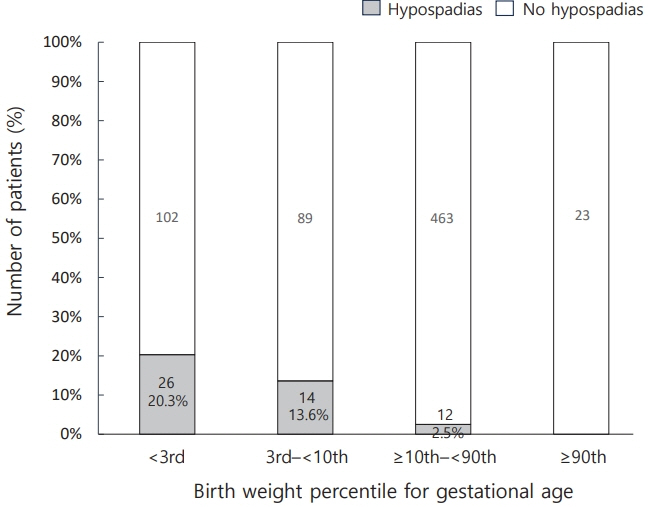
We retrospectively analyzed 729 infants born at ≥24 weeks of gestational age and weighing <1,500 g from January 2012 to December 2022. We assessed the prevalence of hypospadias by birth weight percentiles and also compared the demographics and placental histopathology of the infants with hypospadias (n=52) and those without hypospadias (n=677).
Results
Of the 729 patients analysed, hypospadias was recorded in 26 (20.3%), 14 (26.9%), and 12 (2.5%) infants in the <3rd, ≥3rd–<10th, and ≥10th–<90th percentiles, respectively. Of all of the patients with hypospadias, 50% had birth weights <3rd percentile (p<0.001). The hypospadias group demonstrated a longer mean gestational age (30.1 weeks vs. 27.9 weeks, p<0.001), lower incidence of maternal pregnancy-induced hypertension (48.1% vs. 17.3%, p<0.001), lower incidence of premature rupture of membrane (11.5% vs. 27.1%, p=0.013), lower acute chorioamniotic maternal response (9.1% vs. 35.2%, p<0.001), and higher maternal underperfusion (95.5% vs. 71.9%, p<0.001).
Conclusion
The frequency of hypospadias was found to be the highest among VBLWIs <3rd percentile, who were severely small for their gestational age (SGA). Additionally, the incidence increased with a decreasing birth weight. Physical examination is necessary at birth for VLBWIs classified as SGA. Moreover, the data on the incidence of hypospadias among VLBWIs in neonatal intensive care units can assist in tracking counseling from the prenatal to the postnatal period for patients born <3rd percentile.
Figure
Reference
-
1. Yu X, Nassar N, Mastroiacovo P, Canfield M, Groisman B, Bermejo-Sanchez E, et al. Hypospadias prevalence and trends in international birth defect surveillance systems, 1980-2010. Eur Urol. 2019; 76:482–90.
Article2. Ashina M, Fujioka K, Yoshimoto S, Ioroi T, Iijima K. Incidence of hypospadias in severe small-for-gestational-age infants: a multicenter Asian population study. Pediatr Neonatol. 2020; 61:548–50.
Article3. Gatti JM, Kirsch AJ, Troyer WA, Perez-Brayfield MR, Smith EA, Scherz HC. Increased incidence of hypospadias in small-forgestational age infants in a neonatal intensive-care unit. BJU Int. 2001; 87:548–50.
Article4. Chen MJ, Karaviti LP, Roth DR, Schlomer BJ. Birth prevalence of hypospadias and hypospadias risk factors in newborn males in the United States from 1997 to 2012. J Pediatr Urol. 2018; 14:425.
Article5. Kim SC, Kwon SK, Hong YP. Trends in the incidence of cryptorchidism and hypospadias of registry-based data in Korea: a comparison between industrialized areas of petrochemical estates and a non-industrialized area. Asian J Androl. 2011; 13:715–8.
Article6. Shin CH, Yang SW. Study on the frequency of receptor insensitivity to androgen using the androgen-receptor binding assay in the genetic male children with abnormalities of sexual differentiation. J Korean Pediatr Soc. 2002; 45:95–102.7. Yoo JH. Differential diagnosis of hypospadias. J Korean Soc Pediatr Endocrinol. 2006; 11:15–21.8. Haid B, Tack LJ, Spinoit AF, Weigl C, Steinkellner L, Gernhold C, et al. Being born small for gestational age (SGA) might be associated with a higher reoperation rate in proximal hypospadias. J Pediatr Urol. 2022; 18:609.
Article9. Nissen KB, Udesen A, Garne E. Hypospadias: prevalence, birthweight and associated major congenital anomalies. Congenit Anom (Kyoto). 2015; 55:37–41.
Article10. Ghirri P, Scaramuzzo RT, Bertelloni S, Pardi D, Celandroni A, Cocchi G, et al. Prevalence of hypospadias in Italy according to severity, gestational age and birthweight: an epidemiological study. Ital J Pediatr. 2009; 35:18.
Article11. Toufaily MH, Roberts DJ, Westgate MN, Hunt AT, Holmes LB. Hypospadias, intrauterine growth restriction, and abnormalities of the placenta. Birth Defects Res. 2018; 110:122–7.
Article12. Hussain N, Chaghtai A, Herndon CD, Herson VC, Rosenkrantz TS, McKenna PH. Hypospadias and early gestation growth restriction in infants. Pediatrics. 2002; 109:473–8.
Article13. Hwang IT. The present condition of Korean children born small for gestational age. Korean J Pediatr. 2009; 52:137–41.
Article14. Shin SM, Chang YP, Lee ES, Lee YA, Son DW, Kim MH, et al. Low birth weight, very low birth weight rates and gestational agespecific birth weight distribution of Korean newborn infants. J Korean Med Sci. 2005; 20:182–7.
Article15. Lim JS, Lim SW, Ahn JH, Song BS, Shim KS, Hwang IT. New Korean reference for birth weight by gestational age and sex: data from the Korean Statistical Information Service (2008-2012). Ann Pediatr Endocrinol Metab. 2014; 19:146–53.
Article16. Aviram A, Sherman C, Kingdom J, Zaltz A, Barrett J, Melamed N. Defining early vs late fetal growth restriction by placental pathology. Acta Obstet Gynecol Scand. 2019; 98:365–73.
Article17. Redline RW. Classification of placental lesions. Am J Obstet Gynecol. 2015; 213(4 Suppl):S21–8.
Article18. Baergen RN. Manual of Benirschke and Kaufmann's pathology of the human placenta. Springer Science & Business Media;2005.19. Chong JH, Wee CK, Ho SK, Chan DK. Factors associated with hypospadias in Asian newborn babies. J Perinat Med. 2006; 34:497–500.
Article20. Fujimoto T, Suwa T, Kabe K, Adachi T, Nakabayashi M, Amamiya T. Placental insufficiency in early gestation is associated with hypospadias. J Pediatr Surg. 2008; 43:358–61.
Article21. Campbell MK, Cartier S, Xie B, Kouniakis G, Huang W, Han V. Determinants of small for gestational age birth at term. Paediatr Perinat Epidemiol. 2012; 26:525–33.
Article22. Yinon Y, Kingdom JC, Proctor LK, Kelly EN, Salle JL, Wherrett D, et al. Hypospadias in males with intrauterine growth restriction due to placental insufficiency: the placental role in the embryogenesis of male external genitalia. Am J Med Genet A. 2010; 152A:75–83.
Article23. Hashimoto Y, Kawai M, Nagai S, Matsukura T, Niwa F, Hasegawa T, et al. Fetal growth restriction but not preterm birth is a risk factor for severe hypospadias. Pediatr Int. 2016; 58:573–7.
Article24. Chen Y, Sun L, Geng H, Lei X, Zhang J. Placental pathology and hypospadias. Pediatr Res. 2017; 81:489–95.
Article25. Jensen MS, Wilcox AJ, Olsen J, Bonde JP, Thulstrup AM, Ramlau-Hansen CH, et al. Cryptorchidism and hypospadias in a cohort of 934,538 Danish boys: the role of birth weight, gestational age, body dimensions, and fetal growth. Am J Epidemiol. 2012; 175:917–25.
Article26. Akre O, Boyd HA, Ahlgren M, Wilbrand K, Westergaard T, Hjalgrim H, et al. Maternal and gestational risk factors for hypospadias. Environ Health Perspect. 2008; 116:1071–6.
Article27. Tannenbaum RL. Risk factors associated with prematurity in patients diagnosed with hypospadias (master’s thesis). University of Cincinnati;2013.28. van der Horst HJ, de Wall LL. Hypospadias, all there is to know. Eur J Pediatr. 2017; 176:435–41.
Article29. Chung KM, Lee JY, Han SW. Review of psychosocial and psychosexual adjustment of persons with hypospadias and their parents. Korean J Health Psychol. 2012; 17:1–25.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors influencing birth weight premature infants
- Mortality and Morbidity among Small for Gestational Age Infants in Extremely Low Birth Weight Infants
- Clinical Study of Prematurity and Low Birth Weight Infants
- A Comparative Study to Analyze the Proportion of Highrisk Neonates from Mothers Residing in Metropolitan Cities and Small-to-Medium-Sized Cities in Korea
- The Clinical Features Based on Different Weight Percentile in Appropriate for Gestational Age Preterm Infants