J Stroke.
2024 May;26(2):290-299. 10.5853/jos.2024.00458.
Endovascular Thrombectomy Versus Intravenous Thrombolysis of Posterior Cerebral Artery Occlusion Stroke
- Affiliations
-
- 1Department of Neurology, Helsinki University Hospital and University of Helsinki, Helsinki, Finland
- 2Department of Radiology, Boston Medical Center, Boston, MA, USA
- 3Department of Neurology, Boston Medical Center, Boston, MA, USA
- 4Department of Neurology, Klinikum Ludwigshafen, Ludwigshafen, Germany
- 5Department of Neurology, Heidelberg University Hospital, Heidelberg, Germany
- 6Department of Neurology, Lausanne University Hospital and University of Lausanne, Lausanne, Switzerland
- 7Department of Neuroradiology, Heidelberg University Hospital, Heidelberg, Germany
- 8Department of Radiology, Helsinki University Hospital and University of Helsinki, Helsinki, Finland
- 9Department of Neurology, University Hospital Vall d’Hebron, Barcelona, Spain
- 10Department of Neuroradiology, University Hospital Basel, University of Basel, Basel, Switzerland
- 11Department of Neurology, University of Erlangen, Erlangen, Germany
- 12Department of Neurology, Universitätsklinikum Essen, Essen, Germany
- 13Department of Radiology, Universitätsklinikum Essen, Essen, Germany
- 14Department of Neurology, UZ Leuven, Leuven, Belgium
- 15Department of Neurology, Rhode Island Hospital, Providence, RI, USA
- 16Department of Neurology, University Hospital Carl Gustav Carus, Technische Universität Dresden, Dresden, Germany
- 17Dresden Neurovascular Center, University Hospital Carl Gustav Carus, Technische Universität Dresden, Dresden, Germany
- 18Institute of Neuroradiology, University Hospital Carl Gustav Carus, Technische Universität Dresden, Dresden, Germany
- 19Institute of Diagnostic and Interventional Neuroradiology, University Hospital Bern, University of Bern, Bern, Switzerland
- 20Department of Neuroradiology, University of Erlangen, Erlangen, Germany
- 21Department of Neurology, Grady Memorial Hospital, Atlanta, GA, USA
- 22Department of Neuroradiology, Centro Hospitalar Universitario de Lisboa Central, Lisbon, Portugal
- 23Neurology and Stroke Unit, Department of Neuroscience, Bufalini Hospital, Cesena, Italy
- 24Department of Neurology, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China, Hefei, China
- 25Department of Neurosurgery, Mount Sinai Hospital, New York, NY, USA
- 26Department of Neurology, UT Health McGovern Medical School, Houston, TX, USA
- 27Department of Neurology, Hospital de Egas Moniz, Centro Hospitalar Lisboa Ocidental, Lisbon, Portugal
- 28Department of Neuroradiology, Hospital de Egas Moniz, Centro Hospitalar Lisboa Ocidental, Lisbon, Portugal
- 29Department of Neuroradiology, Charité - Universitätsmedizin Berlin, and Berlin Institute of Health (BIH), Freie Universität Berlin and Humboldt-Universität, Berlin, Germany
- 30Department of Neurology with Experimental Neurology, Charité - Universitätsmedizin Berlin, and Berlin Institute of Health (BIH), Freie Universität Berlin and Humboldt-Universität, Berlin, Germany
- 31Hertie-Institute for Clinical Brain Research, Tübingen University, Tübingen, Germany
- 32Department of Neurosurgery, Barrow Neurological Institute, Phoenix, AZ, USA
- 33Department of Radiology, Neuroradiology and Nuclear Medicine, University Hospital Knappschaftskrankenhaus Bochum, Bochum, Germany
- 34Department of Neurosurgery, University of Buffalo, Buffalo, NY, USA
- 35Department of Interventional Neuroradiology, University Hospital Vall d’Hebron, Barcelona, Spain
- 36Department of Neurology, New York Upstate Medical University, Syracuse, NY, USA
- 37Department of Neurosurgery, University of South Florida, Tampa, FL, USA
- 38Department of Neurology, Turku University Hospital and University of Turku, Turku, Finland
- 39Department of Radiology, Turku University Hospital and University of Turku, Turku, Finland
- 40Department of Neurology, University of Chicago, Chicago, IL, USA
- 41Miami Neuroscience Institute, Miami, FL, USA
- 42Department of Neurology, University of Miami Miller School of Medicine, Miami, FL, USA
- 43Department of Neurology, University of Pittsburgh Medical Center, Pittsburgh, PA, USA
- 44Department of Diagnostic and Interventional Neuroradiology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany
- 45Department of Neurology, University Hospital Basel, University of Basel, Basel, Switzerland
- 46Department of Neurology, University Hospital Bern, University of Bern, Bern, Switzerland
- KMID: 2556049
- DOI: http://doi.org/10.5853/jos.2024.00458
Abstract
- Background and Purpose
Posterior cerebral artery occlusion (PCAo) can cause long-term disability, yet randomized controlled trials to guide optimal reperfusion strategy are lacking. We compared the outcomes of PCAo patients treated with endovascular thrombectomy (EVT) with or without intravenous thrombolysis (IVT) to patients treated with IVT alone.
Methods
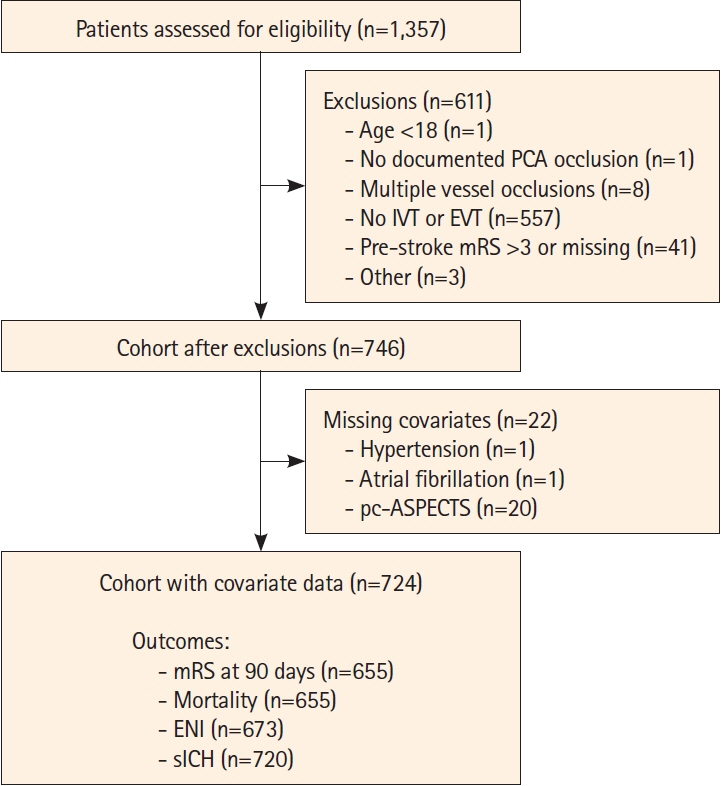
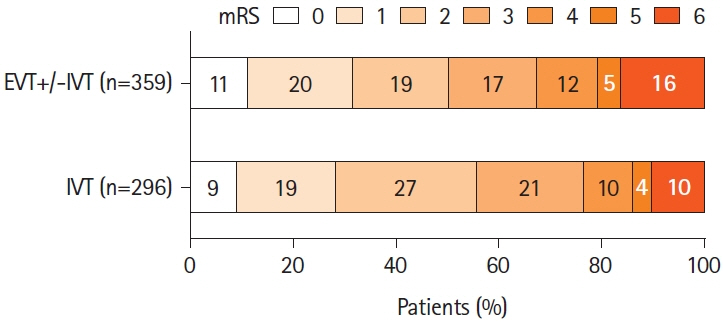
From the multicenter retrospective Posterior cerebraL ArTery Occlusion (PLATO) registry, we included patients with isolated PCAo treated with reperfusion therapy within 24 hours of onset between January 2015 and August 2022. The primary outcome was the distribution of the modified Rankin Scale (mRS) at 3 months. Other outcomes comprised 3-month excellent (mRS 0–1) and independent outcome (mRS 0–2), early neurological improvement (ENI), mortality, and symptomatic intracranial hemorrhage (sICH). The treatments were compared using inverse probability weighted regression adjustment.
Results
Among 724 patients, 400 received EVT+/-IVT and 324 IVT alone (median age 74 years, 57.7% men). The median National Institutes of Health Stroke Scale score on admission was 7, and the occluded segment was P1 (43.9%), P2 (48.3%), P3–P4 (6.1%), bilateral (1.0%), or fetal posterior cerebral artery (0.7%). Compared to IVT alone, EVT+/-IVT was not associated with improved functional outcome (adjusted common odds ratio [OR] 1.07, 95% confidence interval [CI] 0.79–1.43). EVT increased the odds for ENI (adjusted OR [aOR] 1.49, 95% CI 1.05–2.12), sICH (aOR 2.87, 95% CI 1.23–6.72), and mortality (aOR 1.77, 95% CI 1.07–2.95).
Conclusion
Despite higher odds for early improvement, EVT+/-IVT did not affect functional outcome compared to IVT alone after PCAo. This may be driven by the increased risk of sICH and mortality after EVT.
Keyword
Figure
Reference
-
References
1. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016; 387:1723–1731.
Article2. Räty S, Nguyen TN, Nagel S, Puetz V, Alemseged F, Abdalkader M, et al. What is the evidence for endovascular thrombectomy in posterior circulation stroke? Semin Neurol. 2023; 43:345–355.
Article3. Starikova N, Räty S, Strbian D, Kaiser DPO, Gerber JC, Huo X, et al. Endovascular thrombectomy for anterior circulation large vessel occlusion stroke: an evolution of trials. Semin Neurol. 2023; 43:397–407.
Article4. Ntaios G, Spengos K, Vemmou AM, Savvari P, Koroboki E, Stranjalis G, et al. Long-term outcome in posterior cerebral artery stroke. Eur J Neurol. 2011; 18:1074–1080.
Article5. Smith WS, Lev MH, English JD, Camargo EC, Chou M, Johnston SC, et al. Significance of large vessel intracranial occlusion causing acute ischemic stroke and TIA. Stroke. 2009; 40:3834–3840.
Article6. Sabben C, Charbonneau F, Delvoye F, Strambo D, Heldner MR, Ong E, et al. Endovascular therapy or medical management alone for isolated posterior cerebral artery occlusion: a multicenter study. Stroke. 2023; 54:928–937.7. Herweh C, Abdalkader M, Nguyen TN, Puetz V, Schöne D, Kaiser D, et al. Mechanical thrombectomy in isolated occlusion of the proximal posterior cerebral artery. Front Neurol. 2021; 12:697348.
Article8. Strambo D, Bartolini B, Beaud V, Marto JP, Sirimarco G, Dunet V, et al. Thrombectomy and thrombolysis of isolated posterior cerebral artery occlusion: cognitive, visual, and disability outcomes. Stroke. 2020; 51:254–261.
Article9. Cunha B, Baptista M, Pamplona J, Carvalho R, da Câmara CP, Alves M, et al. Acute treatment of isolated posterior cerebral artery occlusion: single center experience. J Stroke Cerebrovasc Dis. 2022; 31:106239.
Article10. Meyer L, Stracke CP, Jungi N, Wallocha M, Broocks G, Sporns PB, et al. Thrombectomy for primary distal posterior cerebral artery occlusion stroke: the TOPMOST study. JAMA Neurol. 2021; 78:434–444.
Article11. Nguyen TN, Qureshi MM, Strambo D, Strbian D, Räty S, Herweh C, et al. Endovascular versus medical management of posterior cerebral artery occlusion stroke: the PLATO study. Stroke. 2023; 54:1708–1717.12. Berge E, Whiteley W, Audebert H, De Marchis GM, Fonseca AC, Padiglioni C, et al. European Stroke Organisation (ESO) guidelines on intravenous thrombolysis for acute ischaemic stroke. Eur Stroke J. 2021; 6:I–LXII.
Article13. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018; 49:e46–e110.
Article14. Maulucci F, Disanto G, Bianco G, Pileggi M, Fischer U, Padlina G, et al. Endovascular therapy outcome in isolated posterior cerebral artery occlusion strokes: a multicenter analysis of the Swiss Stroke Registry. Eur Stroke J. 2023; 8:575–580.
Article15. Alkhiri A, Alamri AF, Alharbi AR, Almaghrabi AA, Alansari N, Niaz AA, et al. Endovascular therapy versus best medical management for isolated posterior cerebral artery occlusion: a systematic review and meta-analysis. Eur Stroke J. 2024; 9:69–77.
Article16. Berberich A, Finitsis S, Strambo D, Michel P, Herweh C, Meyer L, et al. Endovascular therapy versus no endovascular therapy in patients receiving best medical management for acute isolated occlusion of the posterior cerebral artery: a systematic review and meta-analysis. Eur J Neurol. 2022; 29:2664–2673.
Article17. Zetterqvist J, Sjölander A. Doubly robust estimation with the R package drgee. Epidemiol Methods. 2015; 4:69–86.
Article18. Xu S, Ross C, Raebel MA, Shetterly S, Blanchette C, Smith D. Use of stabilized inverse propensity scores as weights to directly estimate relative risk and its confidence intervals. Value Health. 2010; 13:273–277.
Article19. Puetz V, Sylaja PN, Coutts SB, Hill MD, Dzialowski I, Mueller P, et al. Extent of hypoattenuation on CT angiography source images predicts functional outcome in patients with basilar artery occlusion. Stroke. 2008; 39:2485–2490.
Article20. Jovin TG, Li C, Wu L, Wu C, Chen J, Jiang C. Trial of Thrombectomy 6 to 24 hours after stroke due to basilar-artery occlusion. N Engl J Med. 2022; 387:1373–1384.
Article21. Tao C, Nogueira RG, Zhu Y, Sun J, Han H, Yuan G, et al. Trial of endovascular treatment of acute basilar-artery occlusion. N Engl J Med. 2022; 387:1361–1372.
Article22. Seners P, Turc G, Maïer B, Mas JL, Oppenheim C, Baron JC. Incidence and predictors of early recanalization after intravenous thrombolysis: a systematic review and meta-analysis. Stroke. 2016; 47:2409–2412.
Article23. Cals N, Devuyst G, Afsar N, Karapanayiotides T, Bogousslavsky J. Pure superficial posterior cerebral artery territory infarction in the Lausanne Stroke Registry. J Neurol. 2002; 249:855–861.
Article24. Arboix A, Arbe G, García-Eroles L, Oliveres M, Parra O, Massons J. Infarctions in the vascular territory of the posterior cerebral artery: clinical features in 232 patients. BMC Res Notes. 2011; 4:329.25. Langezaal LCM, van der Hoeven EJRJ, Mont’Alverne FJA, de Carvalho JJF, Lima FO, Dippel DWJ, et al. Endovascular therapy for stroke due to basilar-artery occlusion. N Engl J Med. 2021; 384:1910–1920.
Article26. Liu X, Dai Q, Ye R, Zi W, Liu Y, Wang H, et al. Endovascular treatment versus standard medical treatment for vertebrobasilar artery occlusion (BEST): an open-label, randomised controlled trial. Lancet Neurol. 2020; 19:115–122.27. Saver JL, Chapot R, Agid R, Hassan A, Jadhav AP, Liebeskind DS, et al. Thrombectomy for distal, medium vessel occlusions: a consensus statement on present knowledge and promising directions. Stroke. 2020; 51:2872–2884.28. Nguyen TN, Abdalkader M, Qureshi MM, Michel P, Strambo D, Strbian D, et al. First-line stent retriever versus contact aspiration or combined technique for endovascular therapy of posterior cerebral artery occlusion stroke: the PLATO study. Stroke Vasc Interv Neurol. 2024; 4:e001004.29. Nie X, Wang D, Pu Y, Wei Y, Lu Q, Yan H, et al. Endovascular treatment with or without intravenous alteplase for acute ischaemic stroke due to basilar artery occlusion. Stroke Vasc Neurol. 2022; 7:190–199.
Article30. Turc G, Tsivgoulis G, Audebert HJ, Boogaarts H, Bhogal P, De Marchis GM, et al. European Stroke Organisation - European Society for Minimally Invasive Neurological Therapy expedited recommendation on indication for intravenous thrombolysis before mechanical thrombectomy in patients with acute ischaemic stroke and anterior circulation large vessel occlusion. Eur Stroke J. 2022; 7:I–XXVI.
Article31. de Haan R, Limburg M, Bossuyt P, van der Meulen J, Aaronson N. The clinical meaning of Rankin ‘handicap’ grades after stroke. Stroke. 1995; 26:2027–2030.
Article32. Pandit RJ, Gales K, Griffiths PG. Effectiveness of testing visual fields by confrontation. Lancet. 2001; 358:1339–1340.
Article33. Psychogios M, Brehm A. EnDovascular therapy plus best medical treatment (BMT) versus BMT alone for medIum vessel occlusion stroke - a pragmatic, international, multicentre, randomized triaL (DISTAL) [Internet]. Bethesda: National Library of Medicine; December 9, 2021 [accessed January 25, 2024]. Available from: www.clinicaltrials.gov/study/NCT05029414.34. Hill MD. A multicentre, prospective, randomized, parallel group, open-label design to determine the efficacy and safety of endovascular thrombectomy for ischemic stroke patients with symptomatic acute medium vessel intracranial occlusions [Internet]. Bethesda: National Library of Medicine; April 15, 2022 [accessed January 25, 2024]. Available from: www.clinicaltrials.gov/study/NCT05151172.35. Clarençon F. Evaluation of mechanical thrombectomy in acute ischemic stroke related to a distal arterial occlusion: a randomized controlled trial [Internet]. Bethesda: National Library of Medicine; November 14, 2021 [accessed January 25, 2024]. Available from: www.clinicaltrials.gov/study/NCT05030142.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intravenous Thrombolysis and Endovascular Thrombectomy in Acute Ischemic Stroke with Minor Symptom
- Dual Mechanical Thrombectomy for Recanalization of a Resistant Acute Posterior Circulation Stroke
- Intravenous Versus Intra-arterial Thrombolysis for Acute Ischemic Stroke Secondary to Basilar Artery Occlusion
- DIRECT-SAFE: A Randomized Controlled Trial of DIRECT Endovascular Clot Retrieval versus Standard Bridging Therapy
- Mechanical Thrombectomy for Acute Ischemic Stroke with Middle Cerebral Artery Occlusion in 11-year-old Patient