Clin Transplant Res.
2024 Mar;38(1):18-22. 10.4285/kjt.23.0062.
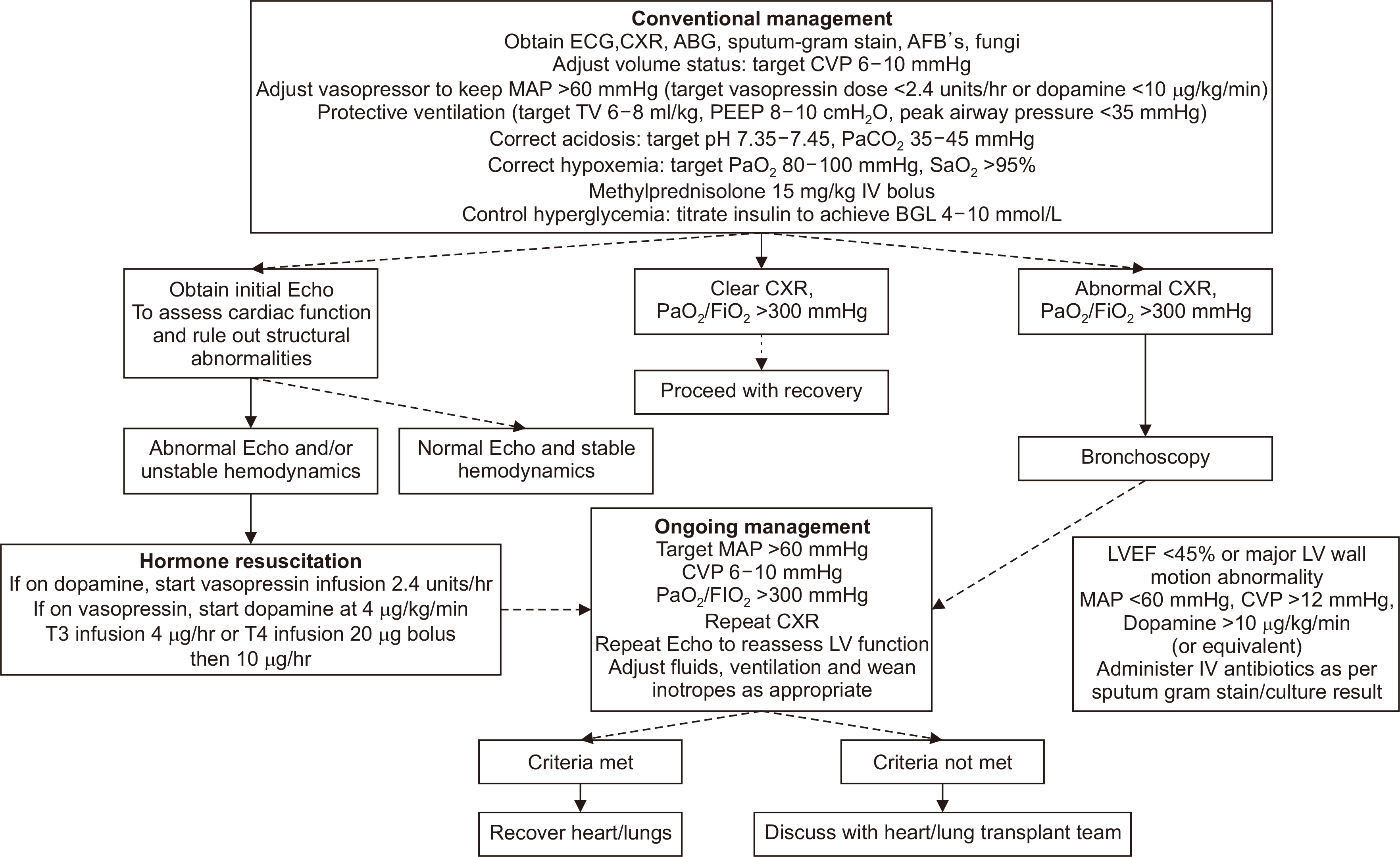
Patient management for thoracic organ donor candidates: the lung transplantation team’s view
- Affiliations
-
- 1Division of Pulmonary, Allergy and Critical Care Medicine, Department of Internal Medicine, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea
- 2Transplantation Research Center and Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea
- KMID: 2555993
- DOI: http://doi.org/10.4285/kjt.23.0062
Abstract
- Despite the increasing demand for lung transplants, donor lungs remain in short supply. Although organ donations have been steadily increasing in Korea, with the utilization rate for donor lungs increasing to 40% in recent years, many potential donor organs remain unused. To match the increasing number of patients on the lung transplant waitlist, it is essential to increase the donor procurement rate through optimal management. Improvements in donor lung management programs can lead to expansion of the donor pool and optimal posttransplant outcomes. This review focuses on basic protocols for the optimal management of donor lungs and summarizes coronavirus disease 2019-related considerations for donor lung evaluation.
Keyword
Figure
Reference
-
1. Valapour M, Lehr CJ, Schladt DP, Smith JM, Goff R, Mupfudze TG, et al. 2023; OPTN/SRTR 2021 annual data report: lung. Am J Transplant. 23(2 Suppl 1):S379–442. DOI: 10.1016/j.ajt.2023.02.009. PMID: 37132345. PMCID: PMC9970343.
Article2. Yeo HJ, Oh DK, Yu WS, Choi SM, Jeon K, Ha M, et al. 2022; Outcomes of patients on the lung transplantation waitlist in Korea: a Korean Network for Organ Sharing data analysis. J Korean Med Sci. 37:e294. DOI: 10.3346/jkms.2022.37.e294. PMID: 36281485. PMCID: PMC9592937.
Article3. Yeo HJ, Kim DH, Kim YS, Jeon D, Cho WH. 2021; Performance changes following the revision of organ allocation system of lung transplant: analysis of Korean Network for Organ Sharing data. J Korean Med Sci. 36:e79. DOI: 10.3346/jkms.2021.36.e79. PMID: 33783144. PMCID: PMC8007421.
Article4. Busl KM, Bleck TP. 2015; Neurogenic pulmonary edema. Crit Care Med. 43:1710–5. DOI: 10.1097/CCM.0000000000001101. PMID: 26066018.
Article5. Yeo HJ, Yoon SH, Lee SE, Jeon D, Kim YS, Cho WH, et al. 2017; Current status and future of lung donation in Korea. J Korean Med Sci. 32:1953–8. DOI: 10.3346/jkms.2017.32.12.1953. PMID: 29115076. PMCID: PMC5680493.
Article6. Snell GI, Yusen RD, Weill D, Strueber M, Garrity E, Reed A, et al. 2017; Report of the ISHLT working group on primary lung graft dysfunction, part I: definition and grading: a 2016 consensus group statement of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 36:1097–103. DOI: 10.1016/j.healun.2017.07.021. PMID: 28942784.7. Venkata-Subramani M, Nunley DR, Roman J. 2021; Donor factors and risk of primary graft dysfunction and mortality post lung transplantation: a proposed conceptual framework. Clin Transplant. 35:e14480. DOI: 10.1111/ctr.14480. PMID: 34516007.
Article8. Copeland H, Hayanga JW, Neyrinck A, MacDonald P, Dellgren G, Bertolotti A, et al. 2020; Donor heart and lung procurement: a consensus statement. J Heart Lung Transplant. 39:501–17. DOI: 10.1016/j.healun.2020.03.020. PMID: 32503726.
Article9. Angel LF, Levine DJ, Restrepo MI, Johnson S, Sako E, Carpenter A, et al. 2006; Impact of a lung transplantation donor-management protocol on lung donation and recipient outcomes. Am J Respir Crit Care Med. 174:710–6. DOI: 10.1164/rccm.200603-432OC. PMID: 16799075.
Article10. Plurad DS, Bricker S, Neville A, Bongard F, Putnam B. 2012; Arginine vasopressin significantly increases the rate of successful organ procurement in potential donors. Am J Surg. 204:856–60. DOI: 10.1016/j.amjsurg.2012.05.011. PMID: 23116641.
Article11. Kumar L. 2016; Brain death and care of the organ donor. J Anaesthesiol Cli Pharmacol. 32:146–52. DOI: 10.4103/0970-9185.168266. PMID: 27275040. PMCID: PMC4874065.
Article12. Follette DM, Rudich SM, Babcock WD. 1998; Improved oxygenation and increased lung donor recovery with high-dose steroid administration after brain death. J Heart Lung Transplant. 17:423–9.13. Dhar R, Cotton C, Coleman J, Brockmeier D, Kappel D, Marklin G, et al. 2013; Comparison of high- and low-dose corticosteroid regimens for organ donor management. J Crit Care. 28:111.e1–7. DOI: 10.1016/j.jcrc.2012.04.015. PMID: 22762934.
Article14. Callahan DS, Neville A, Bricker S, Kim D, Putnam B, Bongard F, et al. 2014; The effect of arginine vasopressin on organ donor procurement and lung function. J Surg Res. 186:452–7. DOI: 10.1016/j.jss.2013.09.028. PMID: 24176209.
Article15. Mascia L, Pasero D, Slutsky AS, Arguis MJ, Berardino M, Grasso S, et al. 2010; Effect of a lung protective strategy for organ donors on eligibility and availability of lungs for transplantation: a randomized controlled trial. JAMA. 304:2620–7. DOI: 10.1001/jama.2010.1796. PMID: 21156950.
Article16. Son E, Jang J, Cho WH, Kim D, Yeo HJ. 2021; Successful lung transplantation after prone positioning in an ineligible donor: a case report. Gen Thorac Cardiovasc Surg. 69:1352–5. DOI: 10.1007/s11748-021-01676-4. PMID: 34159516. PMCID: PMC8218964.
Article17. Miñambres E, Coll E, Duerto J, Suberviola B, Mons R, Cifrian JM, et al. 2014; Effect of an intensive lung donor-management protocol on lung transplantation outcomes. J Heart Lung Transplant. 33:178–84. DOI: 10.1016/j.healun.2013.10.034. PMID: 24365763.
Article18. Bobba CM, Whitson BA, Henn MC, Mokadam NA, Keller BC, Rosenheck J, et al. 2022; Trends in donation after circulatory death in lung transplantation in the United States: impact of era. Transpl Int. 35:10172. DOI: 10.3389/ti.2022.10172. PMID: 35444490. PMCID: PMC9013720.
Article19. Nakajima D, Date H. 2021; Ex vivo lung perfusion in lung transplantation. Gen Thorac Cardiovasc Surg. 69:625–30. DOI: 10.1007/s11748-021-01609-1. PMID: 33683575. PMCID: PMC7938286.
Article20. Ali A, Wang A, Ribeiro RV, Beroncal EL, Baciu C, Galasso M, et al. 2021; Static lung storage at 10°C maintains mitochondrial health and preserves donor organ function. Sci Transl Med. 13:eabf7601. DOI: 10.1126/scitranslmed.abf7601. PMID: 34524862.
Article