Ann Hepatobiliary Pancreat Surg.
2024 May;28(2):248-261. 10.14701/ahbps.23-149.
Prognostication for recurrence patterns after curative resection for pancreatic ductal adenocarcinoma
- Affiliations
-
- 1The Royal London Hospital, Barts Health NHS Trust, London, UK
- 2Barts Cancer Institute, Queen Mary University of London, John Vane Science Centre, Charterhouse Square, London, UK
- KMID: 2555935
- DOI: http://doi.org/10.14701/ahbps.23-149
Abstract
- Backgrounds/Aims
This study aimed to investigate patterns and factors affecting recurrence after curative resection for pancreatic ductal adenocarcinoma (PDAC).
Methods
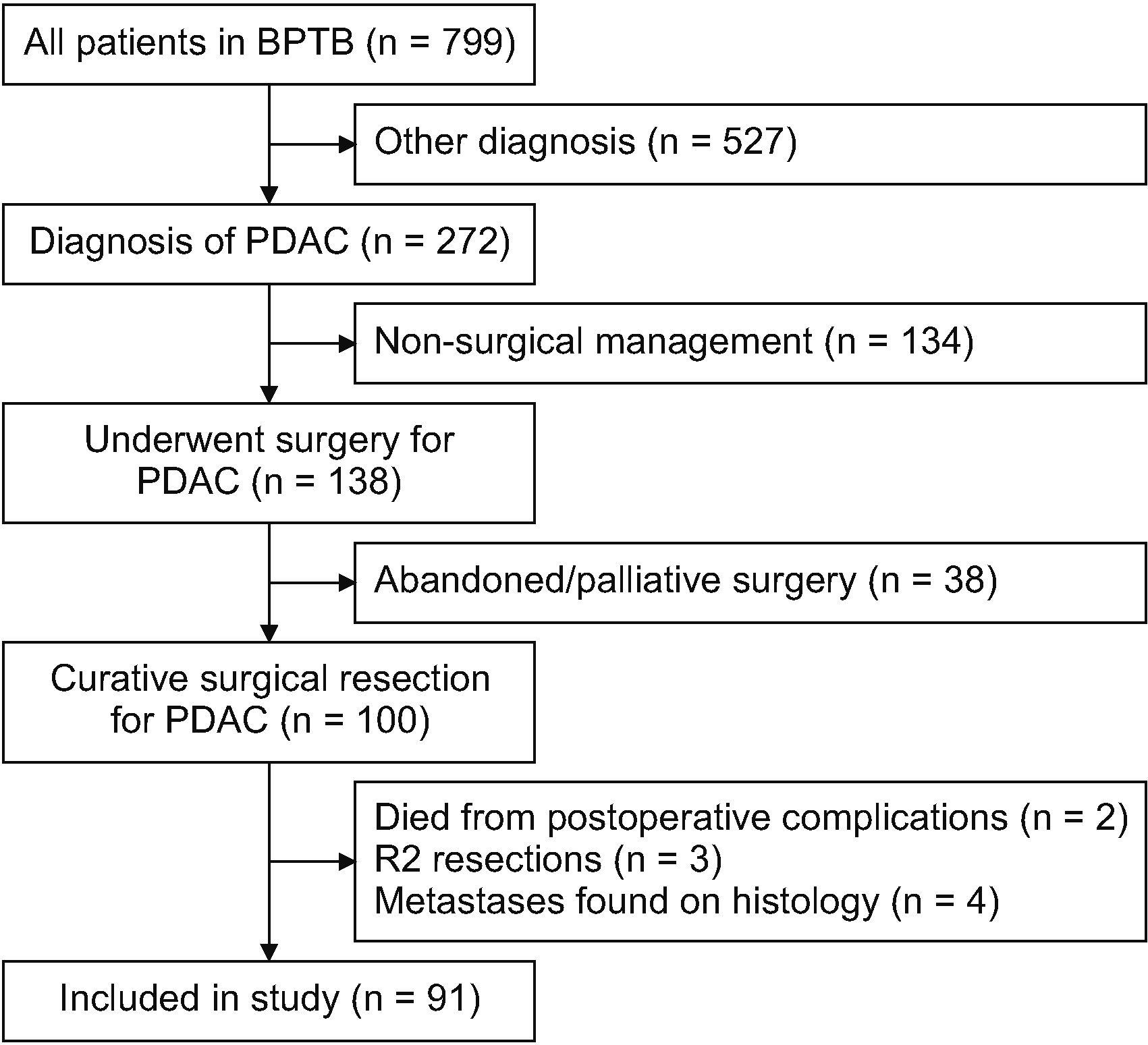
Consecutive patients who underwent curative resection for PDAC (2011-21) and consented to data and tissue collection (Barts Pancreas Tissue Bank) were followed up until May 2023. Clinico-pathological variables were analysed using Cox proportional hazards model.
Results
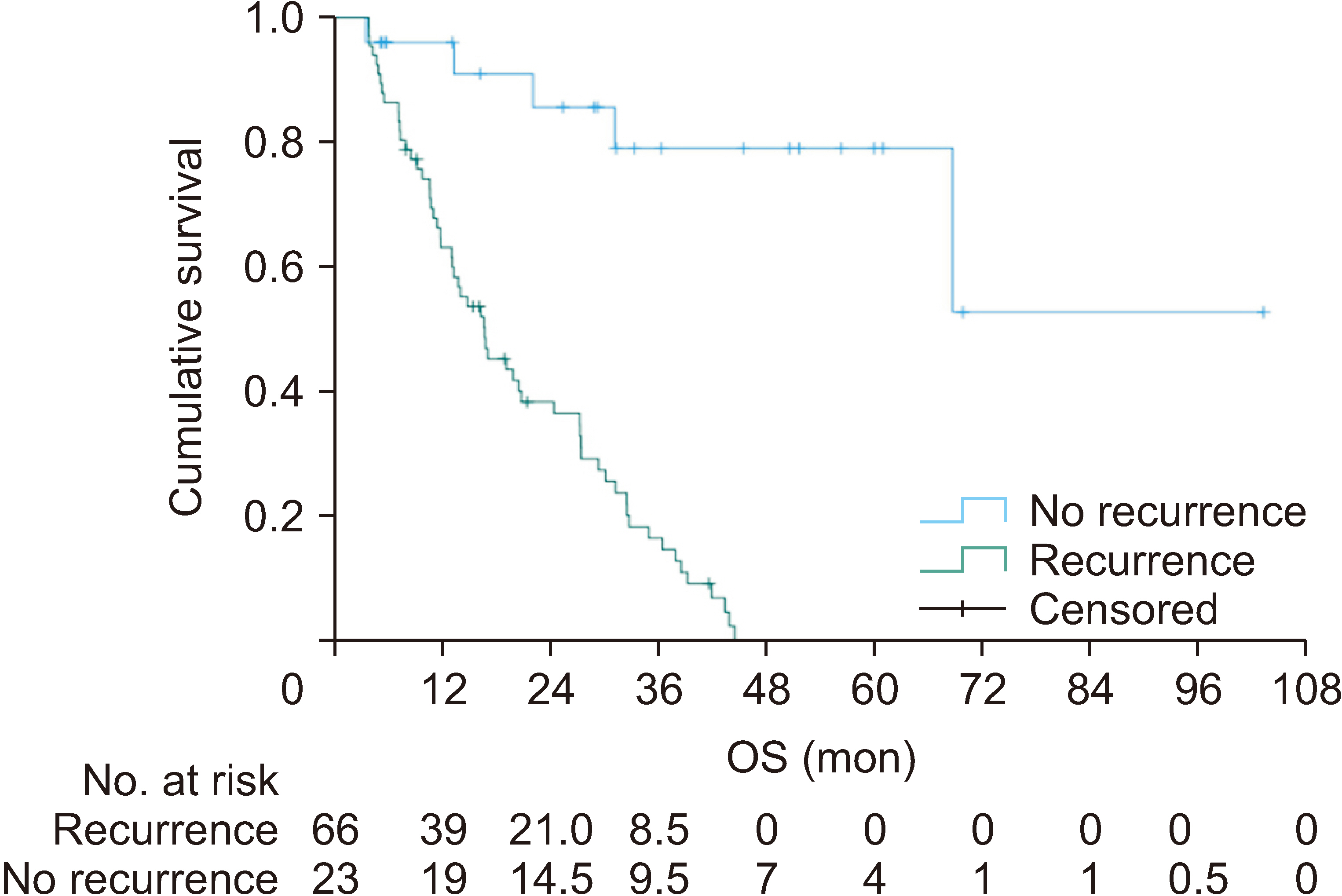
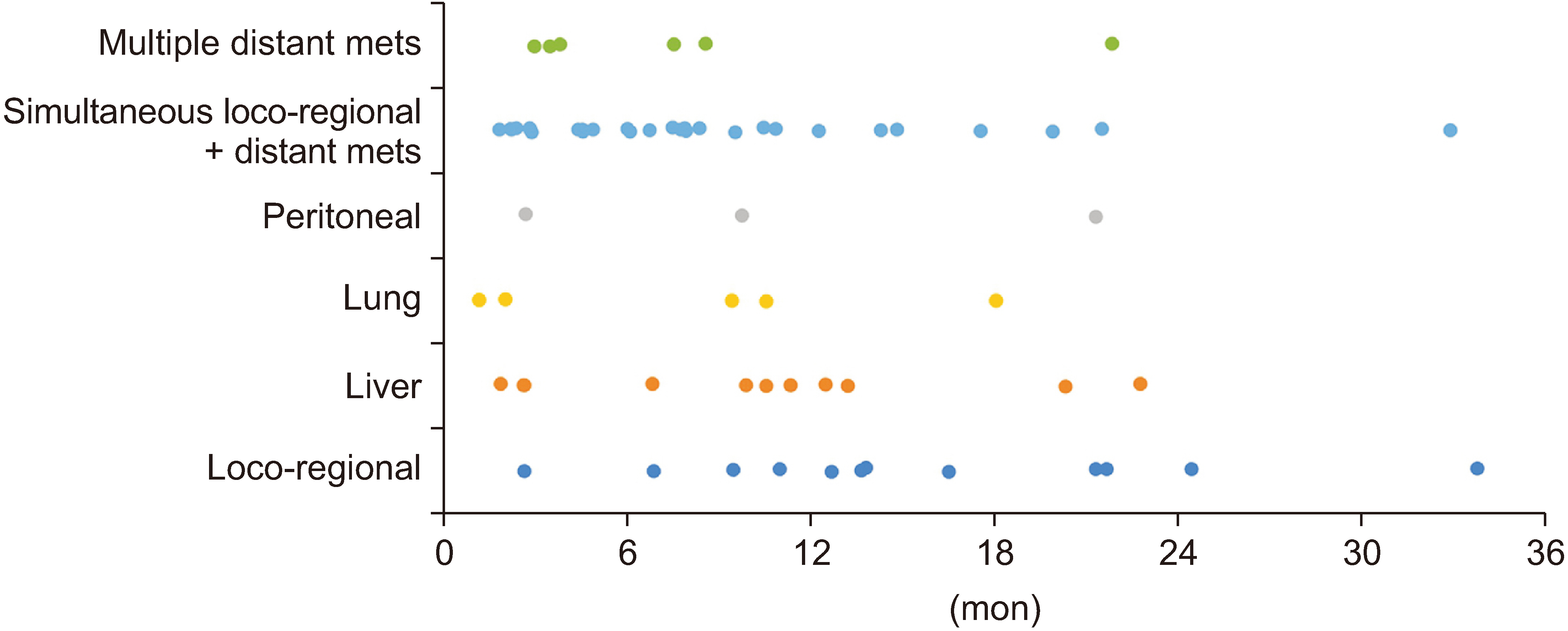
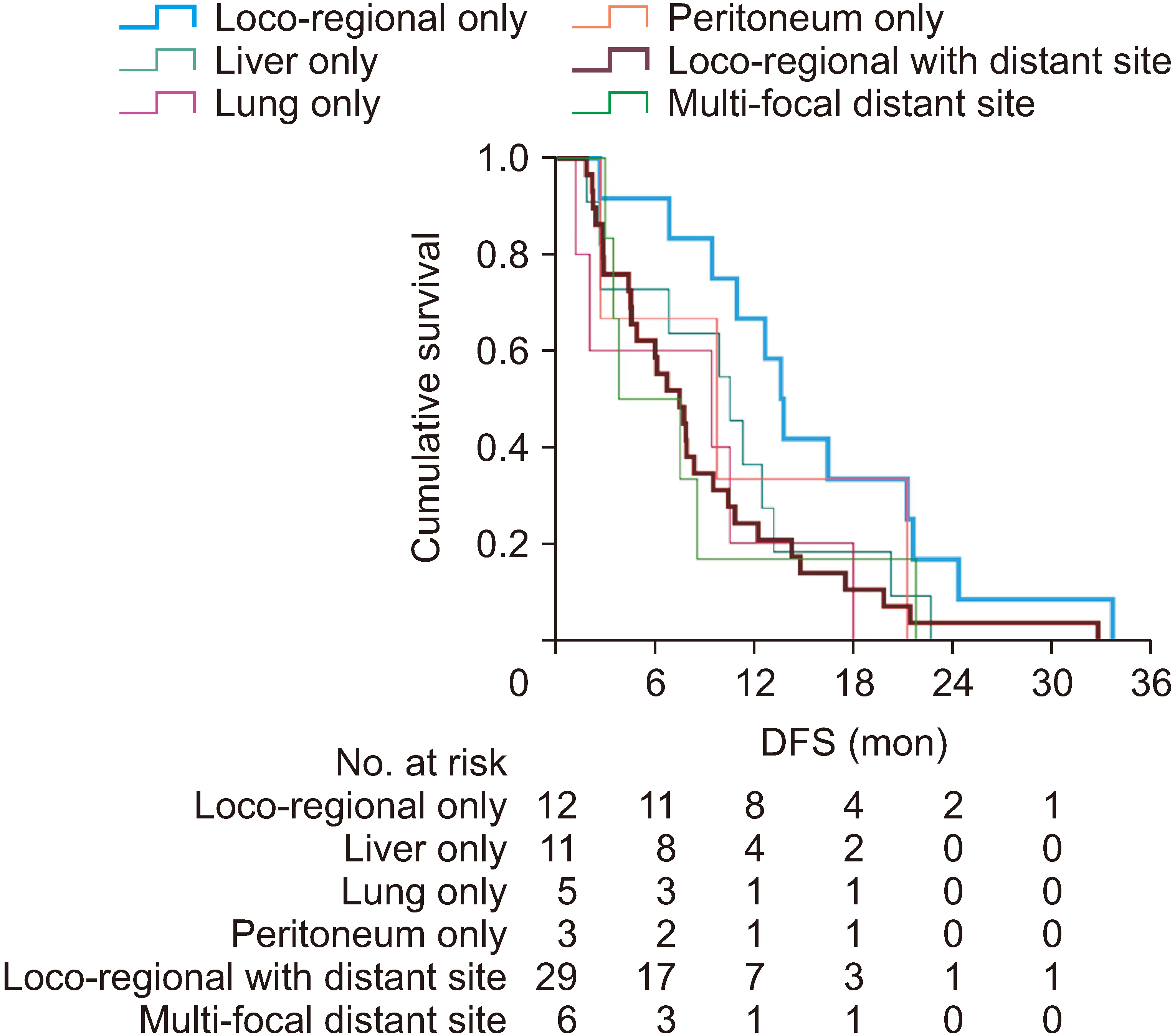
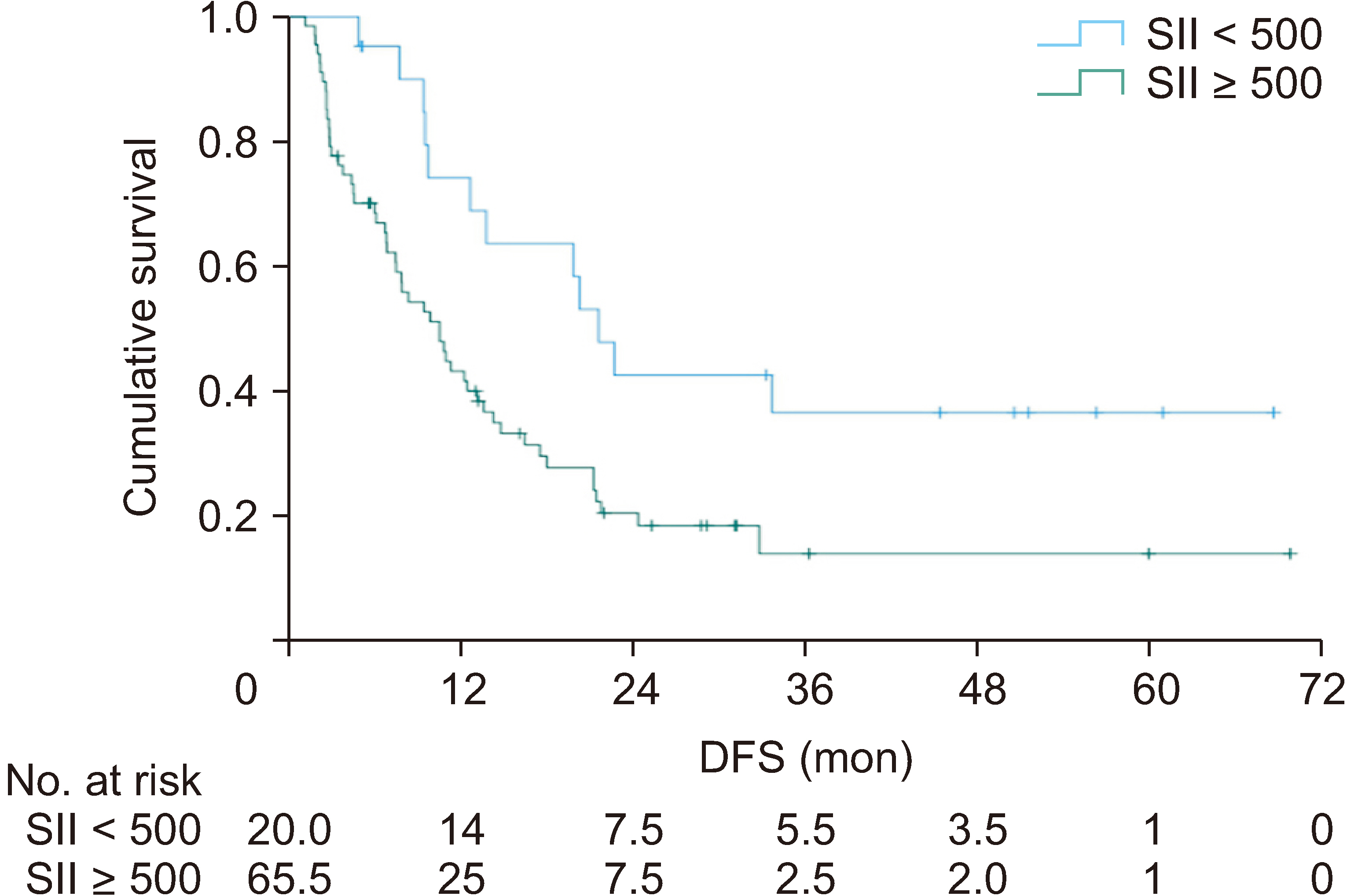
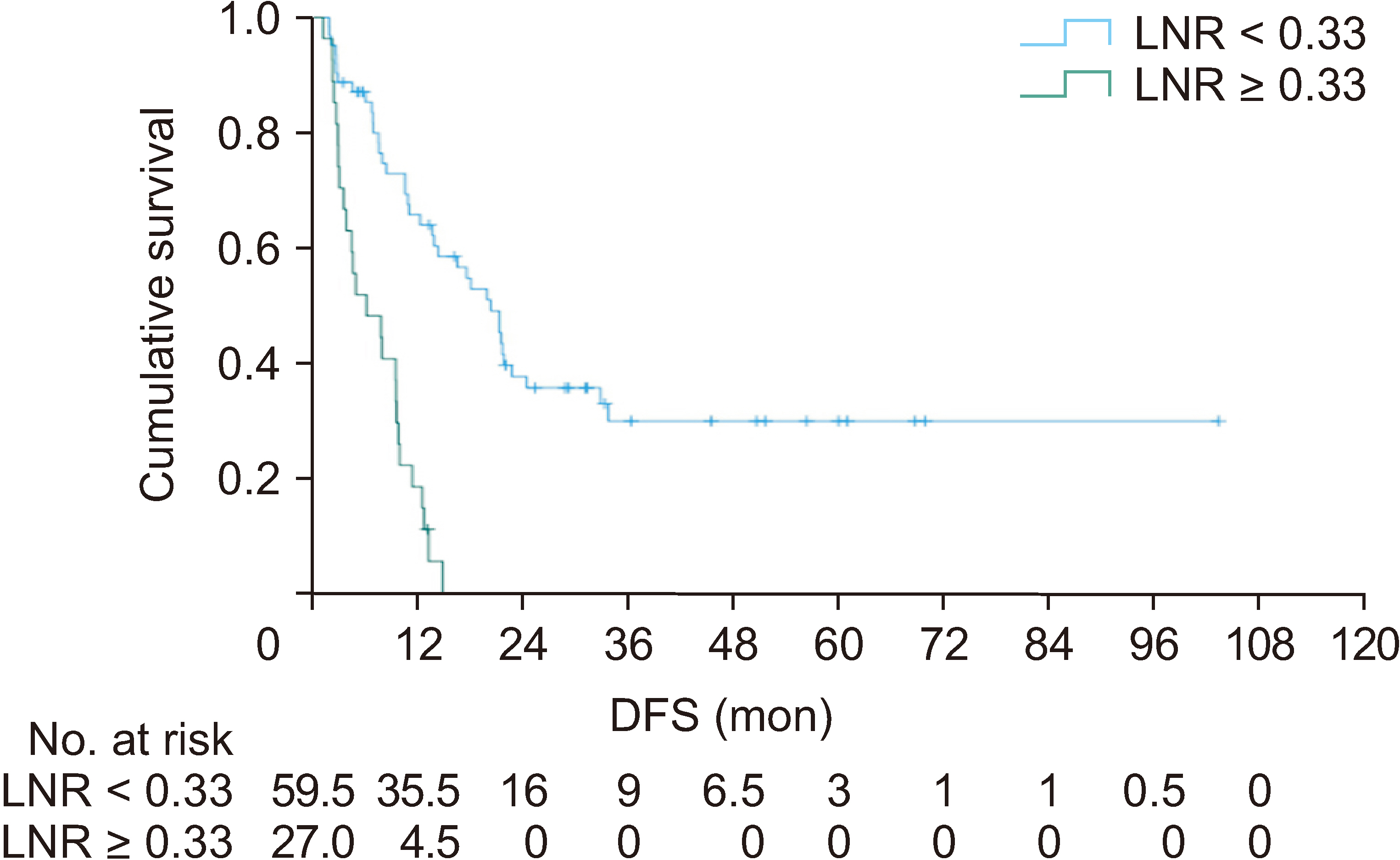
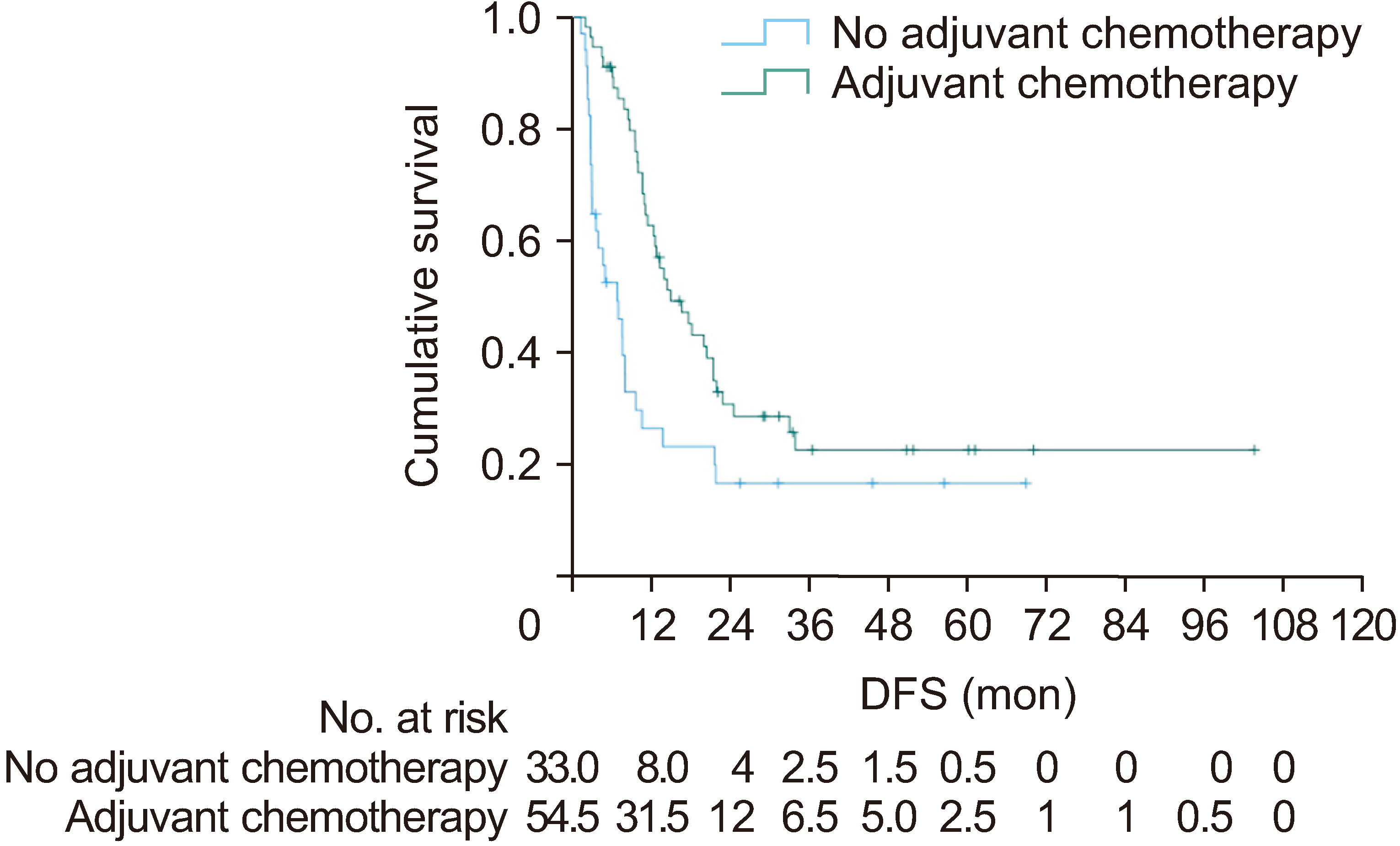
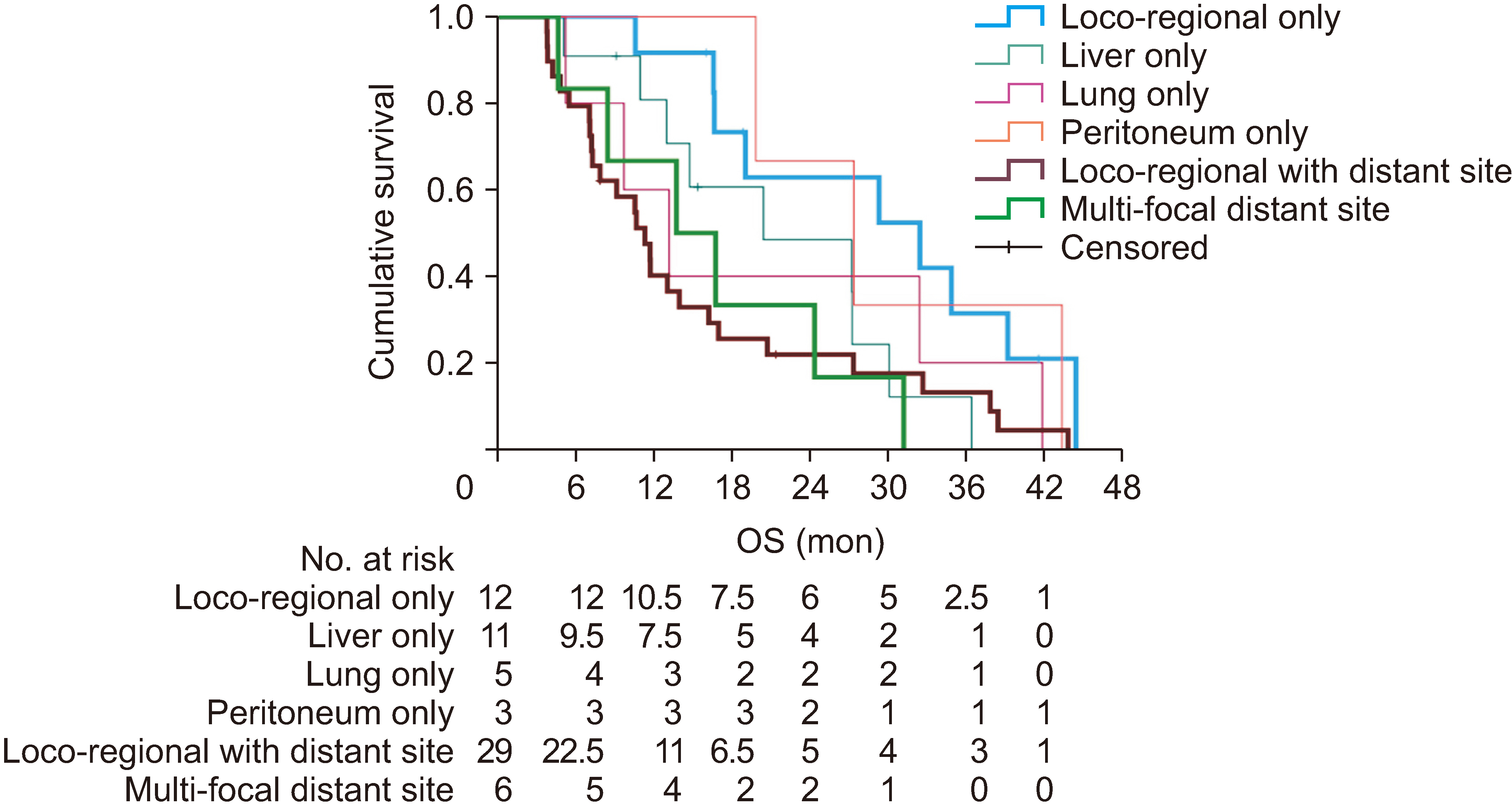
Of 91 people (42 males [46%]; median age, 71 years [range, 43–86 years]) with a median follow-up of 51 months (95% confidence intervals [CIs], 40–61 months), the recurrence rate was 72.5% (n = 66; 12 loco-regional alone, 11 liver alone, 5 lung alone, 3 peritoneal alone, 29 simultaneous loco-regional and distant metastases, and 6 multi-focal distant metastases at first recurrence diagnosis). The median time to recurrence was 8.5 months (95% CI, 6.6–10.5 months). Median survival after recurrence was 5.8 months (95% CI, 4.2–7.3 months). Stratification by recurrence location revealed significant differences in time to recurrence between loco-regional only recurrence (median, 13.6 months; 95% CI, 11.7–15.5 months) and simultaneous loco-regional with distant recurrence (median, 7.5 months; 95% CI, 4.6–10.4 months; p = 0.02, pairwise log-rank test). Significant predictors for recurrence were systemic inflammation index (SII) ≥ 500 (hazard ratio [HR], 4.5; 95% CI, 1.4–14.3), lymph node ratio ≥ 0.33 (HR, 2.8; 95% CI, 1.4–5.8), and adjuvant chemotherapy (HR, 0.4; 95% CI, 0.2–0.7).
Conclusions
Timing to loco-regional only recurrence was significantly longer than simultaneous loco-regional with distant recurrence. Significant predictors for recurrence were SII, lymph node ration, and adjuvant chemotherapy.
Keyword
Figure
Reference
-
References
1. Carioli G, Malvezzi M, Bertuccio P, Boffetta P, Levi F, La Vecchia C, et al. 2021; European cancer mortality predictions for the year 2021 with focus on pancreatic and female lung cancer. Ann Oncol. 32:478–487. DOI: 10.1016/j.annonc.2021.01.006. PMID: 33626377.
Article2. Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, et al. GLOBOCAN 2012: Estimated Cancer Incidence and Mortality Worldwide in 2012 v1.0: IARC cancerbase No. 11. International Agency for Research on Cancer;2012.3. Eliison LF, Wilkins K. 2010; An update on cancer survival. Heal Rep. 21:55–60.4. Ducreux M, Cuhna AS, Caramella C, Hollebecque A, Burtin P, Goéré D, et al. 2015; Cancer of the pancreas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 26 Suppl 5:v56–68. DOI: 10.1093/annonc/mdv295. PMID: 26314780.
Article5. Jones RP, Psarelli EE, Jackson R, Ghaneh P, Halloran CM, Palmer DH, et al. 2019; Patterns of recurrence after resection of pancreatic ductal adenocarcinoma: a secondary analysis of the ESPAC-4 randomized adjuvant chemotherapy trial. JAMA Surg. 154:1038–1048. DOI: 10.1001/jamasurg.2019.3337. PMID: 31483448. PMCID: PMC6727687.
Article6. Conroy T, Castan F, Lopez A, Turpin A, Ben Abdelghani M, Wei AC, et al. 2022; Five-year outcomes of FOLFIRINOX vs gemcitabine as adjuvant therapy for pancreatic cancer: a randomized clinical trial. JAMA Oncol. 8:1571–1578. DOI: 10.1001/jamaoncol.2022.3829. PMID: 36048453. PMCID: PMC9437831.7. Kalisvaart M, Broadhurst D, Marcon F, Pande R, Schlegel A, Sutcliffe R, et al. 2020; Recurrence patterns of pancreatic cancer after pancreatoduodenectomy: systematic review and a single-centre retrospective study. HPB (Oxford). 22:1240–1249. DOI: 10.1016/j.hpb.2020.01.005. PMID: 32046922.
Article8. Tanaka M, Mihaljevic AL, Probst P, Heckler M, Klaiber U, Heger U, et al. 2019; Meta-analysis of recurrence pattern after resection for pancreatic cancer. Br J Surg. 106:1590–1601. DOI: 10.1002/bjs.11295. PMID: 31454073.
Article9. Hayashi K, Ono Y, Takamatsu M, Oba A, Ito H, Sato T, et al. 2022; Prediction of recurrence pattern of pancreatic cancer post-pancreatic surgery using histology-based supervised machine learning algorithms: a single-center retrospective study. Ann Surg Oncol. 29:4624–4634. DOI: 10.1245/s10434-022-11471-x. PMID: 35230581.
Article10. Groot VP, Rezaee N, Wu W, Cameron JL, Fishman EK, Hruban RH, et al. 2018; Patterns, timing, and predictors of recurrence following pancreatectomy for pancreatic ductal adenocarcinoma. Ann Surg. 267:936–945. DOI: 10.1097/SLA.0000000000002234. PMID: 28338509.
Article11. Watanabe Y, Nishihara K, Niina Y, Kudo Y, Kurata K, Okayama T, et al. 2017; Patients with lung recurrence after curative resection for pancreatic ductal adenocarcinoma have a better prognosis than those with recurrence at other sites. JOP J Pancreas. 18:54–61.12. Camp RL, Dolled-Filhart M, Rimm DL. 2004; X-tile: a new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin Cancer Res. 10:7252–7259. DOI: 10.1158/1078-0432.CCR-04-0713. PMID: 15534099.13. Kim JH. 2019; Multicollinearity and misleading statistical results. Korean J Anesthesiol. 72:558–569. DOI: 10.4097/kja.19087. PMID: 31304696. PMCID: PMC6900425.
Article14. Groot VP, Gemenetzis G, Blair AB, Ding D, Javed AA, Burkhart RA, et al. 2018; Implications of the pattern of disease recurrence on survival following pancreatectomy for pancreatic ductal adenocarcinoma. Ann Surg Oncol. 25:2475–2483. DOI: 10.1245/s10434-018-6558-7. PMID: 29948425. PMCID: PMC6220676.
Article15. Kolbeinsson H, Hoppe A, Bayat A, Kogelschatz B, Mbanugo C, Chung M, et al. 2021; Recurrence patterns and postrecurrence survival after curative intent resection for pancreatic ductal adenocarcinoma. Surgery. 169:649–654. DOI: 10.1016/j.surg.2020.06.042. PMID: 32807504.
Article16. Kubo H, Ohgi K, Sugiura T, Ashida R, Yamada M, Otsuka S, et al. 2022; The association between neoadjuvant therapy and pathological outcomes in pancreatic cancer patients after resection: prognostic significance of microscopic venous invasion. Ann Surg Oncol. 29:4992–5002. DOI: 10.1245/s10434-022-11628-8. PMID: 35368218.
Article17. Zheng B, Ohuchida K, Yan Z, Okumura T, Ohtsuka T, Nakamura M, et al. 2017; Primary recurrence in the lung is related to favorable prognosis in patients with pancreatic cancer and postoperative recurrence. World J Surg. 41:2858–2866. DOI: 10.1007/s00268-017-4068-6. PMID: 28634843.
Article18. Ferguson MD, Dong L, Wan J, Deneve JL, Dickson PV, Behrman SW, et al. 2019; Molecular alterations associated with DNA repair in pancreatic adenocarcinoma are associated with sites of recurrence. J Gastrointest Cancer. 50:285–291. DOI: 10.1007/s12029-018-0073-8. PMID: 29427136.
Article19. Shin SH, Kim HJ, Hwang DW, Lee JH, Song KB, Jun E, et al. 2017; The DPC4/SMAD4 genetic status determines recurrence patterns and treatment outcomes in resected pancreatic ductal adenocarcinoma: a prospective cohort study. Oncotarget. 8:17945–17959. DOI: 10.18632/oncotarget.14901. PMID: 28160547. PMCID: PMC5392299.
Article20. Ng KYY, Chow EWX, Jiang B, Lim C, Goh BKP, Lee SY, et al. 2021; Resected pancreatic adenocarcinoma: an Asian institution's experience. Cancer Rep. 4:e1393. DOI: 10.1002/cnr2.1393. PMID: 33939335. PMCID: PMC8551988.
Article21. Maggino L, Malleo G, Crippa S, Belfiori G, Nobile S, Gasparini G, et al. 2023; CA19.9 response and tumor size predict recurrence following post-neoadjuvant pancreatectomy in initially resectable and borderline resectable pancreatic ductal adenocarcinoma. Ann Surg Oncol. 30:207–219. DOI: 10.1245/s10434-022-12622-w. PMID: 36227391. PMCID: PMC9726670.
Article22. Haeno H, Gonen M, Davis MB, Herman JM, Iacobuzio-Donahue CA, Michor F. 2012; Computational modeling of pancreatic cancer reveals kinetics of metastasis suggesting optimum treatment strategies. Cell. 148:362–375. DOI: 10.1016/j.cell.2011.11.060. PMID: 22265421. PMCID: PMC3289413.
Article23. Barnes CA, Aldakkak M, Christians KK, Clarke CN, Dua K, George B, et al. 2020; Radiographic patterns of first disease recurrence after neoadjuvant therapy and surgery for patients with resectable and borderline resectable pancreatic cancer. Surgery. 168:440–447. DOI: 10.1016/j.surg.2020.04.031. PMID: 32641278.
Article24. Park Y, Jun HR, Choi HW, Hwang DW, Lee JH, Song KB, et al. 2021; Circulating tumour cells as an indicator of early and systemic recurrence after surgical resection in pancreatic ductal adenocarcinoma. Sci Rep. 11:1644. DOI: 10.1038/s41598-020-80383-1. PMID: 33462311. PMCID: PMC7814057.
Article25. Hugenschmidt H, Labori KJ, Borgen E, Brunborg C, Schirmer CB, Seeberg LT, et al. 2021; Preoperative CTC-detection by cellsearch® is associated with early distant metastasis and impaired survival in resected pancreatic cancer. Cancers. 13:485. DOI: 10.3390/cancers13030485. PMID: 33513877. PMCID: PMC7865868.
Article26. Uesaka K, Boku N, Fukutomi A, Okamura Y, Konishi M, Matsumoto I, et al. 2016; Adjuvant chemotherapy of S-1 versus gemcitabine for resected pancreatic cancer: a phase 3, open-label, randomised, non-inferiority trial (JASPAC 01). Lancet. 388:248–257. DOI: 10.1016/S0140-6736(16)30583-9. PMID: 27265347.
Article27. Hernandez JM, Morton CA, Al-Saadi S, Villadolid D, Cooper J, Bowers C, et al. 2010; The natural history of resected pancreatic cancer without adjuvant chemotherapy. Am Surg. 76:480–485. DOI: 10.1177/000313481007600514. PMID: 20506876.
Article28. Hishinuma S, Ogata Y, Tomikawa M, Ozawa I, Hirabayashi K, Igarashi S. 2006; Patterns of recurrence after curative resection of pancreatic cancer, based on autopsy findings. J Gastrointest Surg. 10:511–518. DOI: 10.1016/j.gassur.2005.09.016. PMID: 16627216.
Article29. Honselmann KC, Pergolini I, Castillo CF, Deshpande V, Ting D, Taylor MS, et al. 2020; Timing but not patterns of recurrence are different between node-negative and node-positive resected pancreatic cancer. Ann Surg. 272:357–365. DOI: 10.1097/SLA.0000000000003123. PMID: 32675550. PMCID: PMC6639153.
Article30. Walston S, Salloum J, Grieco C, Wuthrick E, Diaz DA, Barney C, et al. 2018; Identifying clinical factors which predict for early failure patterns following resection for pancreatic adenocarcinoma in patients who received adjuvant chemotherapy without chemoradiation. Am J Clin Oncol. 41:1185–1192. DOI: 10.1097/COC.0000000000000452. PMID: 29727311. PMCID: PMC6215749.
Article31. Suto H, Okano K, Oshima M, Ando Y, Takahashi S, Shibata T, et al. 2019; The predictors and patterns of the early recurrence of pancreatic ductal adenocarcinoma after pancreatectomy: the influence of pre- and post- operative adjuvant therapy. BMC Surg. 19:186. DOI: 10.1186/s12893-019-0644-z. PMID: 31796066. PMCID: PMC6891951.
Article32. Schorn S, Demir IE, Samm N, Scheufele F, Calavrezos L, Sargut M, et al. 2018; Meta-analysis of the impact of neoadjuvant therapy on patterns of recurrence in pancreatic ductal adenocarcinoma. BJS Open. 2:52–61. DOI: 10.1002/bjs5.46. PMID: 29951629. PMCID: PMC5989995.
Article33. Zhou Q, Su S, You W, Wang T, Ren T, Zhu L. 2021; Systemic inflammation response index as a prognostic marker in cancer patients: a systematic review and meta-analysis of 38 cohorts. Dose Response. 19:15593258211064744. DOI: 10.1177/15593258211064744. PMID: 34987341. PMCID: PMC8689621.
Article34. Cao W, Shao Y, Zou S, Wang N, Wang J. 2022; Prognostic significance of systemic immune-inflammation index in patients with bladder cancer: a systematic review and meta-analysis. Medicine (Baltimore). 101:e30380. DOI: 10.1097/MD.0000000000030380. PMID: 36086786. PMCID: PMC10980366.
Article35. Liu XC, Jiang YP, Sun XG, Zhao JJ, Zhang LY, Jing X. 2022; Prognostic significance of the systemic immune-inflammation index in patients with cholangiocarcinoma: a meta-analysis. Front Oncol. 12:938549. DOI: 10.3389/fonc.2022.938549. PMID: 35875153. PMCID: PMC9300870.
Article36. Zhang K, Hua YQ, Wang D, Chen LY, Wu CJ, Chen Z, et al. 2019; Systemic immune-inflammation index predicts prognosis of patients with advanced pancreatic cancer. J Transl Med. 17:30. DOI: 10.1186/s12967-019-1782-x. PMID: 30658662. PMCID: PMC6339361.
Article37. Liu X, Sun X, Liu J, Kong P, Chen S, Zhan Y, et al. 2015; Preoperative C-reactive protein/albumin ratio predicts prognosis of patients after curative resection for gastric cancer. Transl Oncol. 8:339–345. DOI: 10.1016/j.tranon.2015.06.006. PMID: 26310380. PMCID: PMC4562973.
Article38. Jomrich G, Gruber ES, Winkler D, Hollenstein M, Gnant M, Sahora K, et al. 2020; Systemic immune-inflammation index (SII) predicts poor survival in pancreatic cancer patients undergoing resection. J Gastrointest Surg. 24:610–618. DOI: 10.1007/s11605-019-04187-z. PMID: 30923999. PMCID: PMC7064450.
Article39. Aziz MH, Sideras K, Aziz NA, Mauff K, Haen R, Roos D, et al. 2019; The systemic-immune-inflammation index independently predicts survival and recurrence in resectable pancreatic cancer and its prognostic value depends on bilirubin levels: a retrospective multicenter cohort study. Ann Surg. 270:139–146. DOI: 10.1097/SLA.0000000000002660. PMID: 29334554.
Article40. Kim HJ, Lee WJ, Kang CM, Hwang HK, Bang SM, Song SY, et al. 2016; Risk factors associated with loco-regional failure after surgical resection in patients with resectable pancreatic cancer. PLoS One. 11:e0157196. DOI: 10.1371/journal.pone.0157196. PMID: 27332708. PMCID: PMC4917092.
Article41. Kwon J, Lee SR, Park SY, Lee JH, Song KB, Hwang DW, et al. 2023; Effect of resection margin status on recurrence pattern and survival in distal pancreatectomy for left-sided pancreatic ductal adenocarcinoma. J Hepatobiliary Pancreat Sci. 30:633–643. DOI: 10.1002/jhbp.1272. PMID: 36380718.
Article42. Raut CP, Tseng JF, Sun CC, Wang H, Wolff RA, Crane CH, et al. 2007; Impact of resection status on pattern of failure and survival after pancreaticoduodenectomy for pancreatic adenocarcinoma. Ann Surg. 246:52–60. DOI: 10.1097/01.sla.0000259391.84304.2b. PMID: 17592291. PMCID: PMC1899216.
Article43. Kurreck A, Weckwerth J, Modest DP, Striefler JK, Bahra M, Bischoff S, et al. 2021; Impact of completeness of adjuvant gemcitabine, relapse pattern, and subsequent therapy on outcome of patients with resected pancreatic ductal adenocarcinoma - A pooled analysis of CONKO-001, CONKO-005, and CONKO-006 trials. Eur J Cancer. 150:250–259. DOI: 10.1016/j.ejca.2021.03.036. PMID: 33940349.
Article44. Tummers WS, Groen JV, Sibinga Mulder BG, Farina-Sarasqueta A, Morreau J, Putter H, et al. 2019; Impact of resection margin status on recurrence and survival in pancreatic cancer surgery. Br J Surg. 106:1055–1065. DOI: 10.1002/bjs.11115. PMID: 30883699. PMCID: PMC6617755.
Article45. Yamamoto T, Uchida Y, Terajima H. 2019; Clinical impact of margin status on survival and recurrence pattern after curative-intent surgery for pancreatic cancer. Asian J Surg. 42:93–99. DOI: 10.1016/j.asjsur.2017.09.003. PMID: 29249392.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Biliary Tract and Pancreas: Survival and Recurrence Pattern after Curative Resection of Pancreatic Cancer
- Analysis on Recurrence of an Invasive Ductal Adenocarcinoma of the Pancreas
- Surgical Outcome of Ductal Adenocarcinoma of the Body and Tail of the Pancreas
- Transcatheter Arterial Chemoembolization for Hepatic Recurrence after Curative Resection of Pancreatic Adenocarcinoma
- Adenocarcinoma of the ampulla of Vater: predictors of survival and recurrence after curative radical resection