Ann Hepatobiliary Pancreat Surg.
2024 May;28(2):134-143. 10.14701/ahbps.24-048.
Surgical outcome and risk scoring to predict survival after hepatic resection for hepatocellular carcinoma with portal vein tumor thrombosis
- Affiliations
-
- 1Division of Hepato-Biliary-Pancreatic Surgery, Department of Surgery, Keimyung University Dongsan Hospital, Daegu, Korea
- 2Division of Hepato-Biliary-Pancreatic Surgery, Department of Surgery, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea
- 3Division of Hepatopancreaticobiliary Surgery, Yonsei University College of Medicine, Seoul, Korea
- 4Division of HBP Surgery and Liver Transplantation, Department of Surgery, Korea University College of Medicine, Seoul, Korea
- 5Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 6Department of Surgery, Dong-A University College of Medicine, Busan, Korea
- 7Division of Hepatobiliary, Pancreas, and Abdominal Organ Transplant, Department of Surgery, Incheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea
- 8Department of Surgery, Daegu Catholic University School of Medicine, Daegu, Korea
- 9Department of Surgery, Gacheon University Gil Medical Center, Incheon, Korea
- 10Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2555926
- DOI: http://doi.org/10.14701/ahbps.24-048
Abstract
- Backgrounds/Aims
The hepatocellular carcinoma (HCC) with portal vein tumor thrombosis (PVTT) is classified as the advanced stage (BCLC stage C) with extremely poor prognosis, and in current guidelines is recommended for systemic therapy. This study aimed to evaluate the surgical outcomes and long-term prognosis after hepatic resection (HR) for patients who have HCC combined with PVTT.
Methods
We retrospectively analyzed 332 patients who underwent HR for HCC with PVTT at ten tertiary referral hospitals in South Korea.
Results
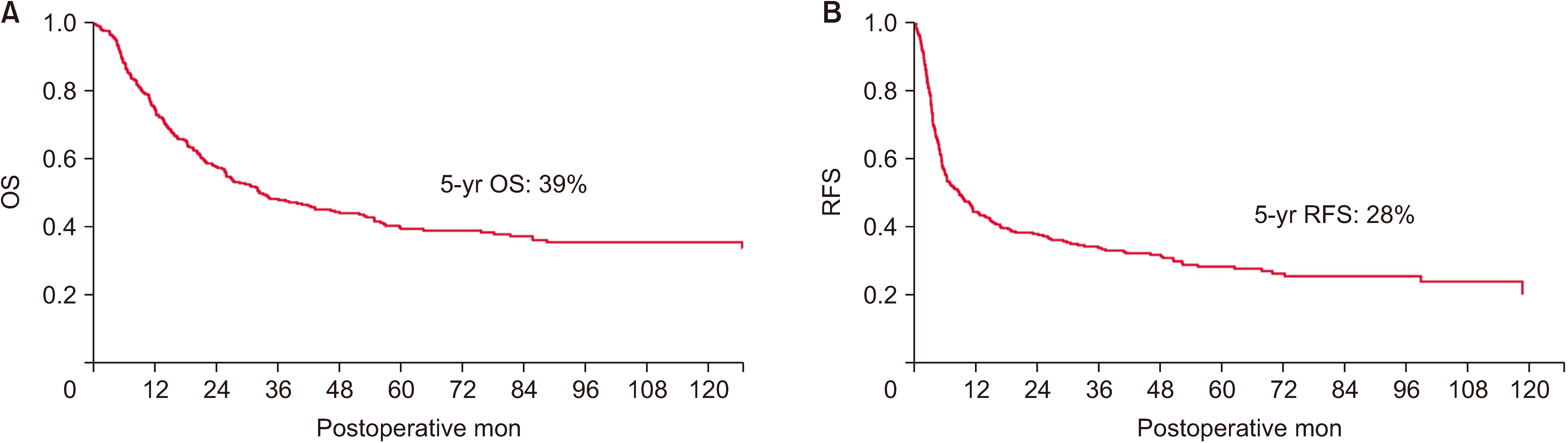
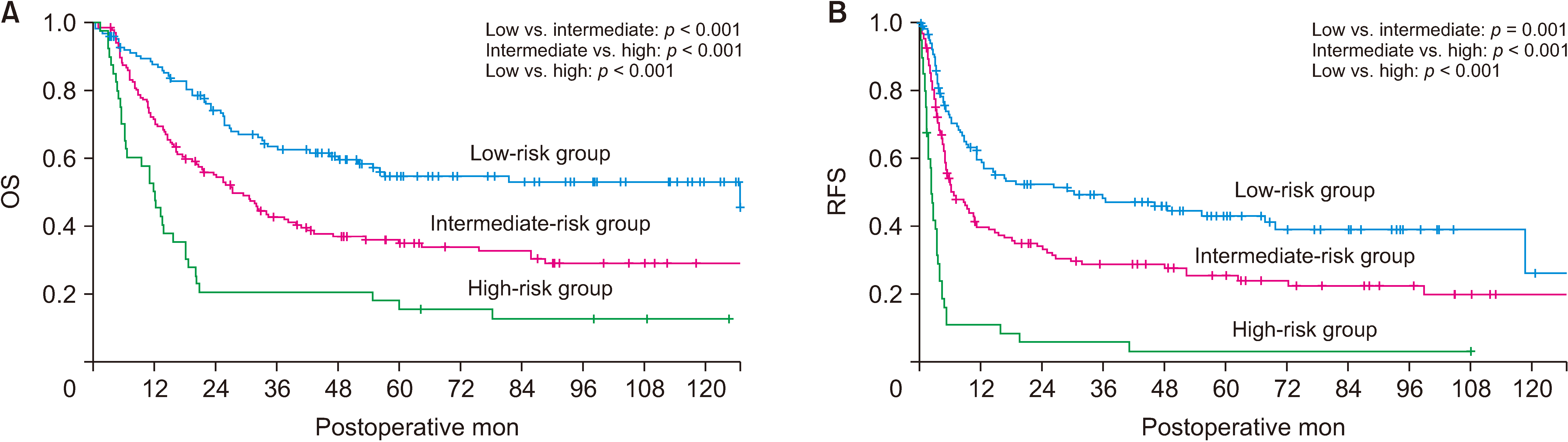
The median overall and recurrence-free survival after HR were 32.4 and 8.6 months, while the 1-, 3-, and 5-year overall survival rates were 75%, 48%, and 39%, respectively. In multivariate analysis, tumor number, tumor size, AFP, PIVKA−II, neutrophil-to-lymphocyte ratio, and albumin–bilirubin (ALBI) grade were significant prognostic factors. The risk scoring was developed using these seven factors–tumor, inflammation and hepatic function (TIF), to predict patient prognosis. The prognosis of the patients was well stratified according to the scores (log-rank test, p < 0.001).
Conclusions
HR for patients who have HCC combined with PVTT provided favorable survival outcomes. The risk scoring was useful in predicting prognosis, and determining the appropriate treatment strategy for those patients who have HCC with PVTT.
Figure
Reference
-
References
1. Ikai I, Arii S, Kojiro M, Ichida T, Makuuchi M, Matsuyama Y, et al. 2004; Reevaluation of prognostic factors for survival after liver resection in patients with hepatocellular carcinoma in a japanese nationwide survey. Cancer. 101:796–802. DOI: 10.1002/cncr.20426. PMID: 15305412.
Article2. Minagawa M, Makuuchi M. 2006; Treatment of hepatocellular carcinoma accompanied by portal vein tumor thrombus. World J Gastroenterol. 12:7561–7567. DOI: 10.3748/wjg.v12.i47.7561. PMID: 17171782. PMCID: PMC4088035.
Article3. Reig M, Forner A, Rimola J, Ferrer-Fabrega J, Burrel M, Garcia-Criado Á, et al. 2022; Bclc strategy for prognosis prediction and treatment recommendation: the 2022 update. J Hepatol. 76:681–693. DOI: 10.1016/j.jhep.2021.11.018. PMID: 34801630. PMCID: PMC8866082.
Article4. Omata M, Lesmana LA, Tateishi R, Chen PJ, Lin SM, Yoshida H, et al. 2010; Asian Pacific Association for the Study of the Liver consensus recommendations on hepatocellular carcinoma. Hepatol Int. 4:439–474. DOI: 10.1007/s12072-010-9165-7. PMID: 20827404. PMCID: PMC2900561.
Article5. Peng ZW, Guo RP, Zhang YJ, Lin XJ, Chen MS, Lau WY. 2012; Hepatic resection versus transcatheter arterial chemoembolization for the treatment of hepatocellular carcinoma with portal vein tumor thrombus. Cancer. 118:4725–4736. DOI: 10.1002/cncr.26561. PMID: 22359112.
Article6. Kokudo T, Hasegawa K, Matsuyama Y, Takayama T, Izumi N, Kadoya M, et al. 2016; Survival benefit of liver resection for hepatocellular carcinoma associated with portal vein invasion. J Hepatol. 65:938–943. DOI: 10.1016/j.jhep.2016.05.044. PMID: 27266618.
Article7. Lee JM, Jang BK, Lee YJ, Choi WY, Choi SM, Chung WJ, et al. 2016; Survival outcomes of hepatic resection compared with transarterial chemoembolization or sorafenib for hepatocellular carcinoma with portal vein tumor thrombosis. Clin Mol Hepatol. 22:160–167. DOI: 10.3350/cmh.2016.22.1.160. PMID: 27044767. PMCID: PMC4825165.
Article8. Hatano E, Uemoto S, Yamaue H, Yamamoto M. Japanese Society of Hepato-Biliary-Pancreatic S. 2018; Significance of hepatic resection and adjuvant hepatic arterial infusion chemotherapy for hepatocellular carcinoma with portal vein tumor thrombus in the first branch of portal vein and the main portal trunk: a project study for hepatic surgery of the japanese society of hepato-biliary-pancreatic surgery. J Hepatobiliary Pancreat Sci. 25:395–402. DOI: 10.1002/jhbp.574. PMID: 30091239.
Article9. Zhang ZY, Dong KS, Zhang EL, Zhang LW, Chen XP, Dong HH. 2019; Resection might be a meaningful choice for hepatocellular carcinoma with portal vein thrombosis: a systematic review and meta-analysis. Medicine (Baltimore). 98:e18362. DOI: 10.1097/MD.0000000000018362. PMID: 31852141. PMCID: PMC6922393.10. Chok KS, Cheung TT, Chan SC, Poon RT, Fan ST, Lo CM. 2014; Surgical outcomes in hepatocellular carcinoma patients with portal vein tumor thrombosis. World J Surg. 38:490–496. DOI: 10.1007/s00268-013-2290-4. PMID: 24132826.
Article11. Kudo M, Kitano M, Sakurai T, Nishida N. 2015; General rules for the clinical and pathological study of primary liver cancer, nationwide follow-up survey and clinical practice guidelines: the outstanding achievements of the liver cancer study group of Japan. Dig Dis. 33:765–770. DOI: 10.1159/000439101. PMID: 26488173.
Article12. Malik HZ, Prasad KR, Halazun KJ, Aldoori A, Al-Mukhtar A, Gomez D, et al. 2007; Preoperative prognostic score for predicting survival after hepatic resection for colorectal liver metastases. Ann Surg. 246:806–814. DOI: 10.1097/SLA.0b013e318142d964. PMID: 17968173.
Article13. Halazun KJ, Najjar M, Abdelmessih RM, Samstein B, Griesemer AD, Guarrera JV, et al. 2017; Recurrence after liver transplantation for hepatocellular carcinoma: a new moral to the story. Ann Surg. 265:557–564. DOI: 10.1097/SLA.0000000000001966. PMID: 27611615.14. Wei Z, Zhao J, Bi X, Zhang Y, Zhou J, Li Z, et al. 2022; Neoadjuvant radiotherapy for resectable hepatocellular carcinoma with portal vein tumor thrombus: a systematic review. Hepatobiliary Surg Nutr. 11:709–717. DOI: 10.21037/hbsn-20-854. PMID: 36268237. PMCID: PMC9577988.
Article15. Famularo S, Donadon M, Cipriani F, Giuliante F, Ferri S, Celsa C, et al. 2022; Hepatectomy versus sorafenib in advanced nonmetastatic hepatocellular carcinoma: a real-life multicentric weighted comparison. Ann Surg. 275:743–752. DOI: 10.1097/SLA.0000000000005373. PMID: 35081572.
Article16. Komatsu S, Ueshima K, Kido M, Kuramitsu K, Tsugawa D, Yanagimoto H, et al. 2023; Hepatectomy versus sorafenib for advanced hepatocellular carcinoma with macroscopic portal vein tumor thrombus: a bi-institutional propensity-matched cohort study. J Hepatobiliary Pancreat Sci. 30:303–314. DOI: 10.1002/jhbp.1236. PMID: 36047804.
Article17. Tsilimigras DI, Bagante F, Moris D, Hyer JM, Sahara K, Paredes AZ, et al. 2020; Recurrence patterns and outcomes after resection of hepatocellular carcinoma within and beyond the barcelona clinic liver cancer criteria. Ann Surg Oncol. 27:2321–2331. DOI: 10.1245/s10434-020-08452-3. PMID: 32285278.
Article18. Konishi M, Ryu M, Kinoshita T, Inoue K. 2001; Surgical treatment of hepatocellular carcinoma with direct removal of the tumor thrombus in the main portal vein. Hepatogastroenterology. 48:1421–1424.19. Pawlik TM, Poon RT, Abdalla EK, Ikai I, Nagorney DM, Belghiti J, et al. 2005; Hepatectomy for hepatocellular carcinoma with major portal or hepatic vein invasion: results of a multicenter study. Surgery. 137:403–410. DOI: 10.1016/j.surg.2004.12.012. PMID: 15800485.
Article20. Kondo K, Chijiiwa K, Kai M, Otani K, Nagaike K, Ohuchida J, et al. 2009; Surgical strategy for hepatocellular carcinoma patients with portal vein tumor thrombus based on prognostic factors. J Gastrointest Surg. 13:1078–1083. DOI: 10.1007/s11605-009-0854-2. PMID: 19296182.
Article21. Ikai I, Hatano E, Hasegawa S, Fujii H, Taura K, Uyama N, et al. 2006; Prognostic index for patients with hepatocellular carcinoma combined with tumor thrombosis in the major portal vein. J Am Coll Surg. 202:431–438. DOI: 10.1016/j.jamcollsurg.2005.11.012. PMID: 16500247.
Article22. Le Treut YP, Hardwigsen J, Ananian P, Saïsse J, Grégoire E, Richa H, et al. 2006; Resection of hepatocellular carcinoma with tumor thrombus in the major vasculature. A European case-control series. J Gastrointest Surg. 10:855–862. DOI: 10.1016/j.gassur.2005.12.011. PMID: 16769542.
Article23. Cheng AL, Qin S, Ikeda M, Galle PR, Ducreux M, Kim TY, et al. 2022; Updated efficacy and safety data from IMbrave150: atezolizumab plus bevacizumab vs. sorafenib for unresectable hepatocellular carcinoma. J Hepatol. 76:862–873. DOI: 10.1016/j.jhep.2021.11.030. PMID: 34902530.
Article24. Abou-Alfa GK, Chan SL, Kudo M, Lau G, Kelley RK, Furuse J, et al. 2022; Phase 3 randomized, open-label, multicenter study of tremelimumab (T) and durvalumab (D) as first-line therapy in patients (PTS) with unresectable hepatocellular carcinoma (uHCC): Himalaya. JCO. 40:379. DOI: 10.1200/JCO.2022.40.4_suppl.379.
Article25. Hwang S, Lee YJ, Kim KH, Ahn CS, Moon DB, Ha TY, et al. 2015; Long-term outcome after resection of huge hepatocellular carcinoma ≥ 10 cm: single-institution experience with 471 patients. World J Surg. 39:2519–2528. DOI: 10.1007/s00268-015-3129-y. PMID: 26126423.
Article26. Jiang JF, Lao YC, Yuan BH, Yin J, Liu X, Chen L, et al. 2017; Treatment of hepatocellular carcinoma with portal vein tumor thrombus: advances and challenges. Oncotarget. 8:33911–33921. DOI: 10.18632/oncotarget.15411. PMID: 28430610. PMCID: PMC5464922.
Article27. Wang HL, Cucchetti A, Zhong JH, Ye XP, Gu JH, Ma L, et al. 2016; Should hepatic resection be recommended to patients with hepatocellular carcinoma and portal vein invasion? J Hepatol. 65:1057–1058. DOI: 10.1016/j.jhep.2016.07.022. PMID: 27475616.
Article28. Liang L, Chen TH, Li C, Xing H, Han J, Wang MD, et al. 2018; A systematic review comparing outcomes of surgical resection and non-surgical treatments for patients with hepatocellular carcinoma and portal vein tumor thrombus. HPB (Oxford). 20:1119–1129. DOI: 10.1016/j.hpb.2018.06.1804. PMID: 30056066.
Article29. Zhang XP, Wang K, Li N, Zhong CQ, Wei XB, Cheng YQ, et al. 2017; Survival benefit of hepatic resection versus transarterial chemoembolization for hepatocellular carcinoma with portal vein tumor thrombus: a systematic review and meta-analysis. BMC Cancer. 17:902. DOI: 10.1186/s12885-017-3895-z. PMID: 29282010. PMCID: PMC5746018.
Article30. Giannini EG, Bucci L, Garuti F, Brunacci M, Lenzi B, Valente M, et al. 2018; Patients with advanced hepatocellular carcinoma need a personalized management: a lesson from clinical practice. Hepatology. 67:1784–1796. DOI: 10.1002/hep.29668. PMID: 29159910.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical features of portal vein thrombosis in hepatocellular carcinoma
- Liver transplantation for hepatocellular carcinoma with portal vein tumor thrombosis
- Management strategies for advanced hepatocellular carcinoma with portal vein tumor thrombosis
- A Case of Hepatocellular Carcinoma with Portal Vein Tumor Thrombosis Treated by Hepatic Artery Injection Chemotherapy and Radiotherapy
- Reappraisal of transarterial radioembolization for liver-confined hepatocellular carcinoma with portal vein tumor thrombosis: Editorial on “Transarterial radioembolization versus tyrosine kinase inhibitor in hepatocellular carcinoma with portal vein thrombosis”