J Korean Med Sci.
2024 May;39(19):e164. 10.3346/jkms.2024.39.e164.
Clinical Characteristics and Frequency of Chronic Obstructive Pulmonary Disease Exacerbations in Korean Patients: Findings From the KOCOSS Cohort 2012–2021
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Incheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Division of Pulmonary, Allergy and Critical Care Medicine, Department of Internal Medicine, Hallym University Kangdong Sacred Heart Hospital, Seoul, Korea
- 4Division of Pulmonary, Allergy and Critical Care Medicine, Department of Internal Medicine, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea
- KMID: 2555914
- DOI: http://doi.org/10.3346/jkms.2024.39.e164
Abstract
- Background
Acute exacerbations of chronic obstructive pulmonary disease (AECOPD) exert a substantial burden on patients and healthcare systems; however, data related to the frequency of AECOPD in the Korean population are limited. Therefore, this study aimed to describe the frequency of severe, and moderate or severe AECOPD, as well as clinical and demographic characteristics of patients with chronic obstructive pulmonary disease (COPD) in South Korea.
Methods
Data from patients aged > 40 years with post-bronchodilator forced expiratory volume in 1 second (FEV 1 )/forced vital capacity ≤ 70% of the normal predicted value from the Korea COPD Subgroup Study database were analyzed (April 2012 to 2021). The protocol was based on the EXAcerbations of COPD and their OutcomeS International study. Data were collected retrospectively for year 0 (0–12 months before study enrollment) based on patient recall, and prospectively during years 1, 2, and 3 (0–12, 13–24, and 25–36 months after study enrollment, respectively). The data were summarized using descriptive statistics.
Results
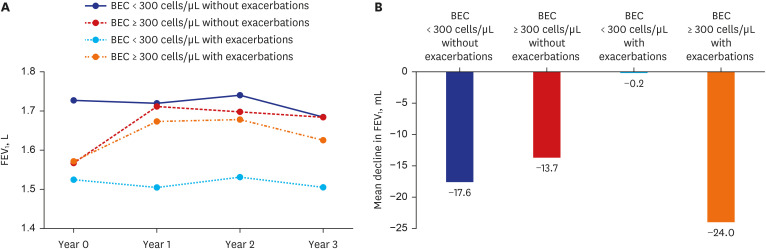
Data from 3,477 Korean patients (mean age, 68.5 years) with COPD were analyzed. Overall, most patients were male (92.3%), former or current smokers (90.8%), had a modified Medical Research Council dyspnea scale score ≥ 1 (83.3%), and had moderate airflow limitation (54.4%). The mean body mass index (BMI) of the study population was 23.1 kg/m 2 , and 27.6% were obese or overweight. Hypertension was the most common comorbidity (37.6%). The mean blood eosinophil count was 226.8 cells/μL, with 21.9% of patients having ≥ 300 cells/μL. A clinically insignificant change in FEV 1 (+1.4%) was observed a year after enrollment. Overall, patients experienced a mean of 0.2 severe annual AECOPD and approximately 1.1 mean moderate or severe AECOPD. Notably, the rates of severe AECOPD remained generally consistent over time. Compared with patients with no exacerbations, patients who experienced severe exacerbations had a lower mean BMI (21.7 vs. 23.1 kg/m2 ; P < 0.001) and lower lung function parameters (all Pvalues < 0.001), but reported high rates of depression (25.5% vs. 15.1%; P = 0.044) and anxiety (37.3% vs. 16.7%; P < 0.001) as a comorbidity.
Conclusion
Findings from this Korean cohort of patients with COPD indicated a high exacerbation burden, which may be attributable to the unique characteristics of the study population and suboptimal disease management. This highlights the need to align clinical practices with the latest treatment recommendations to alleviate AECOPD burden in Korea.
Keyword
Figure
Reference
-
1. Global Initiative for Chronic Obstructive Lung Disease (GOLD). 2023 GOLD report. Updated 2023. Accessed March 25, 2024. https://goldcopd.org/2023-gold-report-2/# .2. World Health Organization. Chronic obstructive pulmonary disease (COPD). Updated 2023. Accessed March 27, 2023. https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd) .3. Choi JY, Kim SY, Lee JH, Park YB, Kim YH, Um SJ, et al. Clinical characteristics of chronic obstructive pulmonary disease in female patients: findings from a KOCOSS cohort. Int J Chron Obstruct Pulmon Dis. 2020; 15:2217–2224. PMID: 33061339.4. Hanania NA. Chronic obstructive pulmonary disease (COPD) is a major cause of morbidity and mortality worldwide. Respir Med. 2012; 106(Suppl 2):S1–S2.5. Kim SH, Lee H, Kim Y, Rhee CK, Min KH, Hwang YI, et al. Recent prevalence of and factors associated with chronic obstructive pulmonary disease in a rapidly aging society: Korea National Health and Nutrition Examination Survey 2015–2019. J Korean Med Sci. 2023; 38(14):e108. PMID: 37038644.6. National Health Insurance Service. Health security system. Updated 2020. Accessed March 27, 2023. https://www.nhis.or.kr/english/wbheaa02300m01.do .7. Park SC, Kim DW, Park EC, Shin CS, Rhee CK, Kang YA, et al. Mortality of patients with chronic obstructive pulmonary disease: a nationwide populationbased cohort study. Korean J Intern Med. 2019; 34(6):1272–1278. PMID: 31610634.8. Kim C, Kim Y, Yang DW, Rhee CK, Kim SK, Hwang YI, et al. Direct and indirect costs of chronic obstructive pulmonary disease in Korea. Tuberc Respir Dis (Seoul). 2019; 82(1):27–34. PMID: 30302958.9. Yoon J, Seo H, Oh IH, Yoon SJ. The non-communicable disease burden in Korea: findings from the 2012 Korean Burden of Disease Study. J Korean Med Sci. 2016; 31(Suppl 2):S158–S167. PMID: 27775253.10. Whittaker H, Rubino A, Müllerová H, Morris T, Varghese P, Xu Y, et al. Frequency and severity of exacerbations of COPD associated with future risk of exacerbations and mortality: a UK routine health care data study. Int J Chron Obstruct Pulmon Dis. 2022; 17:427–437. PMID: 35264849.11. Wedzicha JA, Brill SE, Allinson JP, Donaldson GC. Mechanisms and impact of the frequent exacerbator phenotype in chronic obstructive pulmonary disease. BMC Med. 2013; 11(1):181. PMID: 23945277.12. Rothnie KJ, Müllerová H, Smeeth L, Quint JK. Natural history of chronic obstructive pulmonary disease exacerbations in a general practice-based population with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018; 198(4):464–471. PMID: 29474094.13. Song JH, Lee CH, Um SJ, Park YB, Yoo KH, Jung KS, et al. Clinical impacts of the classification by 2017 GOLD guideline comparing previous ones on outcomes of COPD in real-world cohorts. Int J Chron Obstruct Pulmon Dis. 2018; 13:3473–3484. PMID: 30498337.14. Choi JY, Kim JW, Kim YH, Yoo KH, Jung KS, Lee JH, et al. Clinical characteristics of non-smoking chronic obstructive pulmonary disease patients: findings from the KOCOSS cohort. COPD. 2022; 19(1):174–181. PMID: 35392750.15. Kim TO, Shin HJ, Kim YI, Rhee CK, Lee WY, Lim SY, et al. Adherence to the GOLD guideline in COPD management of South Korea: findings from KOCOSS study 2011–2018. Chonnam Med J. 2019; 55(1):47–53. PMID: 30740340.16. Lee JY, Chon GR, Rhee CK, Kim DK, Yoon HK, Lee JH, et al. Characteristics of patients with chronic obstructive pulmonary disease at the first visit to a pulmonary medical center in Korea: the Korea COPD Subgroup Study team cohort. J Korean Med Sci. 2016; 31(4):553–560. PMID: 27051239.17. Yoon HY, Park SY, Lee CH, Byun MK, Na JO, Lee JS, et al. Prediction of first acute exacerbation using COPD subtypes identified by cluster analysis. Int J Chron Obstruct Pulmon Dis. 2019; 14:1389–1397. PMID: 31388298.18. National Library of Medicine. Exacerbations and their outcomes international (EXACOS International). Updated 2023. Accessed March 27, 2023. https://classic.clinicaltrials.gov/ct2/show/NCT05750810?cond=EXACOS&draw=2&rank=1 .19. National Library of Medicine. Exacerbations and their outcomes international (EXACOS International) (EXACOS-Intl). Updated 2023. Accessed March 27, 2023. https://clinicaltrials.gov/ct2/show/NCT04928417 .20. Choi JY, Milne S, Yunus F, Rhee CK, Matsunaga K. Current chronic obstructive pulmonary disease treatment status in Asia: a position statement of the Asian Pacific Society of Respirology. Tuberc Respir Dis (Seoul). 2022; 85(3):279–282. PMID: 35501669.21. Park HY, Lee H, Kang D, Choi HS, Ryu YH, Jung KS, et al. Understanding racial differences of COPD patients with an ecological model: two large cohort studies in the US and Korea. Ther Adv Chronic Dis. 2021; 12:2040622320982455. PMID: 33613934.22. Fukuchi Y, Fernandez L, Kuo HP, Mahayiddin A, Celli B, Decramer M, et al. Efficacy of tiotropium in COPD patients from Asia: a subgroup analysis from the UPLIFT trial. Respirology. 2011; 16(5):825–835. PMID: 21539680.23. Lee H, Shin SH, Gu S, Zhao D, Kang D, Joi YR, et al. Racial differences in comorbidity profile among patients with chronic obstructive pulmonary disease. BMC Med. 2018; 16(1):178. PMID: 30285854.24. Wedzicha JA, Zhong N, Ichinose M, Humphries M, Fogel R, Thach C, et al. Indacaterol/glycopyrronium versus salmeterol/fluticasone in Asian patients with COPD at a high risk of exacerbations: results from the FLAME study. Int J Chron Obstruct Pulmon Dis. 2017; 12:339–349. PMID: 28176893.25. Kim KY, Miravitlles M, Sliwinski P, Costello R, Carter V, Tan J, et al. Comparison of clinical baseline characteristics between Asian and Western COPD patients in a prospective, international, multicenter study. Int J Chron Obstruct Pulmon Dis. 2019; 14:1595–1601. PMID: 31440042.26. Jo YS, Hwang YI, Yoo KH, Lee MG, Jung KS, Shin KC, et al. Racial differences in prevalence and clinical characteristics of asthma-chronic obstructive pulmonary disease overlap. Front Med (Lausanne). 2021; 8:780438. PMID: 34881272.27. Jo YS, Kim YH, Lee JY, Kim K, Jung KS, Yoo KH, et al. Impact of BMI on exacerbation and medical care expenses in subjects with mild to moderate airflow obstruction. Int J Chron Obstruct Pulmon Dis. 2018; 13:2261–2269. PMID: 30100716.28. Chang Y, Kang HY, Lim D, Cho HJ, Khang YH. Long-term trends in smoking prevalence and its socioeconomic inequalities in Korea, 1992–2016. Int J Equity Health. 2019; 18(1):148. PMID: 31533732.29. Zahra A, Cheong HK, Park JH. Burden of disease attributable to smoking in Korea. Asia Pac J Public Health. 2017; 29(1):47–59. PMID: 28198651.30. Papadopoulos G, Vardavas CI, Limperi M, Linardis A, Georgoudis G, Behrakis P. Smoking cessation can improve quality of life among COPD patients: validation of the clinical COPD questionnaire into Greek. BMC Pulm Med. 2011; 11(1):13. PMID: 21352544.31. Kim Y, Cho WK. Effects of smoking on disease risk among South Korean adults. Tob Induc Dis. 2018; 16:45. PMID: 31516443.32. Rhee CK, Chau NQ, Yunus F, Matsunaga K, Perng DW. on behalf the COPD Assembly of the APSR. Management of COPD in Asia: a position statement of the Asian Pacific Society of Respirology. Respirology. 2019; 24(10):1018–1025. PMID: 31276272.33. Lee EG, Rhee CK. Epidemiology, burden, and policy of chronic obstructive pulmonary disease in South Korea: a narrative review. J Thorac Dis. 2021; 13(6):3888–3897. PMID: 34277078.34. Han MK, Quibrera PM, Carretta EE, Barr RG, Bleecker ER, Bowler RP, et al. Frequency of exacerbations in patients with chronic obstructive pulmonary disease: an analysis of the SPIROMICS cohort. Lancet Respir Med. 2017; 5(8):619–626. PMID: 28668356.35. Sato M, Chubachi S, Sasaki M, Haraguchi M, Kameyama N, Tsutsumi A, et al. Impact of mild exacerbation on COPD symptoms in a Japanese cohort. Int J Chron Obstruct Pulmon Dis. 2016; 11:1269–1278. PMID: 27354785.36. Sim M, Yii A, Xu X, Bahety P, Loh CH, Navarro Rojas AA, et al. Characteristics of patients with chronic obstructive pulmonary disease treated with long-acting bronchodilators in a real-world setting in Singapore: a single-senter observational study. Int J Chron Obstruct Pulmon Dis. 2022; 17:1349–1363. PMID: 35711173.37. Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999; 54(7):581–586. PMID: 10377201.38. Nishimura K, Izumi T, Tsukino M, Oga T. Dyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPD. Chest. 2002; 121(5):1434–1440. PMID: 12006425.39. Kim Y, Kim YJ, Kang YM, Cho WK. Exploring the impact of number and type of comorbidities on the risk of severe COPD exacerbations in Korean Population: a Nationwide Cohort Study. BMC Pulm Med. 2021; 21(1):151. PMID: 33957924.40. Westerik JA, Metting EI, van Boven JF, Tiersma W, Kocks JW, Schermer TR. Associations between chronic comorbidity and exacerbation risk in primary care patients with COPD. Respir Res. 2017; 18(1):31. PMID: 28166777.41. Jeong SH, Lee H, Carriere KC, Shin SH, Moon SM, Jeong BH, et al. Comorbidity as a contributor to frequent severe acute exacerbation in COPD patients. Int J Chron Obstruct Pulmon Dis. 2016; 11:1857–1865. PMID: 27536097.42. Laurin C, Moullec G, Bacon SL, Lavoie KL. Impact of anxiety and depression on chronic obstructive pulmonary disease exacerbation risk. Am J Respir Crit Care Med. 2012; 185(9):918–923. PMID: 22246177.43. Martínez-Gestoso S, García-Sanz MT, Carreira JM, Salgado FJ, Calvo-Álvarez U, Doval-Oubiña L, et al. Impact of anxiety and depression on the prognosis of copd exacerbations. BMC Pulm Med. 2022; 22(1):169. PMID: 35488330.44. Hawkins NM, Petrie MC, Jhund PS, Chalmers GW, Dunn FG, McMurray JJ. Heart failure and chronic obstructive pulmonary disease: diagnostic pitfalls and epidemiology. Eur J Heart Fail. 2009; 11(2):130–139. PMID: 19168510.45. Chen W, Thomas J, Sadatsafavi M, FitzGerald JM. Risk of cardiovascular comorbidity in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Lancet Respir Med. 2015; 3(8):631–639. PMID: 26208998.46. Nishimura M, Makita H, Nagai K, Konno S, Nasuhara Y, Hasegawa M, et al. Annual change in pulmonary function and clinical phenotype in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012; 185(1):44–52. PMID: 22016444.47. Juthong S, Kaenmuang P. Association between blood eosinophils with exacerbation and patient-reported outcomes in chronic obstructive pulmonary disease patients in an endemic area for parasitic infections: a prospective study. J Thorac Dis. 2020; 12(9):4868–4876. PMID: 33145060.48. Yun JH, Lamb A, Chase R, Singh D, Parker MM, Saferali A, et al. Blood eosinophil count thresholds and exacerbations in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2018; 141(6):2037–2047.e10. PMID: 29709670.49. Dalin DA, Løkke A, Kristiansen P, Jensen C, Birkefoss K, Christensen HR, et al. A systematic review of blood eosinophils and continued treatment with inhaled corticosteroids in patients with COPD. Respir Med. 2022; 198:106880. PMID: 35599064.50. Morel AEG, Varga AN, Heymans MW, Dongen JM, Schaik DJ, Tulder MW, et al. Dealing with missing data in real-world data: a scoping review of simulation studies. Res Sq. 2022.51. Roche N, Reddel H, Martin R, Brusselle G, Papi A, Thomas M, et al. Quality standards for real-world research. Focus on observational database studies of comparative effectiveness. Ann Am Thorac Soc. 2014; 11(Suppl 2):S99–S104. PMID: 24559028.52. Liang Z, Zhong N, Chen R, Ma Q, Sun Y, Wen F, et al. Investigation of the clinical, radiological and biological factors associated with disease progression, phenotypes and endotypes of COPD in China (COMPASS): study design, protocol and rationale. ERJ Open Res. 2021; 7(3):00201–02021. PMID: 34527722.53. Oh SH, Ku H, Park KS. Prevalence and socioeconomic burden of diabetes mellitus in South Korean adults: a population-based study using administrative data. BMC Public Health. 2021; 21(1):548. PMID: 33743612.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pharmacologic Therapies for Preventing Chronic Obstructive Pulmonary Disease Exacerbations: A Comprehensive Review
- Sputum Inflammometry to Manage Chronic Obstructive Pulmonary Disease Exacerbations: Beyond Guidelines
- Blood eosinophil count and treatment patterns of chronic obstructive pulmonary disease patients in South Korea using real-world data
- The Relationship between Airway Inflammation and Exacerbation in Chronic Obstructive Pulmonary Disease
- Status of Studies Investigating Asthma–Chronic Obstructive Pulmonary Disease Overlap in Korea: A Review