J Korean Med Sci.
2024 May;39(19):e163. 10.3346/jkms.2024.39.e163.
Diagnostic Pitfall and Clinical Characteristics of Variant Versus Wild-Type Transthyretin Amyloid Cardiomyopathy in Asian Population: The Korean Nationwide Cohort Study
- Affiliations
-
- 1Division of Cardiology, Department of Medicine, Heart Vascular Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Division of Cardiology, Department of Internal Medicine, Seoul St. Mary’s Hospital, Catholic Research Institute for Intractable Cardiovascular Disease, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Cardiology, Medical Research Institute, Pusan National University Hospital, Pusan National University College of Medicine, Busan, Korea
- 4Division of Cardiology, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 5Division of Cardiology, Wonju Severance Christian Hospital, Yonsei University Wonju College of Medicine, Wonju, Korea
- 6Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 7Medical Affairs, Pfizer Pharmaceuticals Korea Ltd., Seoul, Korea
- 8Division of Cardiology, Department of Medicine, Warren Alpert Medical School of Brown University, Providence, RI, USA
- 9Department of Cardiology, Smidt Heart Institute, Cedars-Sinai Medical Center, Los Angeles, CA, USA
- KMID: 2555913
- DOI: http://doi.org/10.3346/jkms.2024.39.e163
Abstract
- Background
Transthyretin amyloidosis cardiomyopathy (ATTR-CM) is an under-recognized cause of heart failure (HF) with clinical phenotypes that vary across regions and genotypes. We sought to characterize the clinical characteristics of ATTR-CM in Asia.
Methods
Data from a nationwide cohort of patients with ATTR-CM from six major tertiary centres in South Korea were analysed between 2010 and 2021. All patients underwent clinical evaluation, biochemical laboratory tests, echocardiography, and transthyretin (TTR) genotyping at the time of diagnosis. The study population comprised 105 Asian ATTR-CM patients (mean age: 69 years; male: 65.7%, wild-type ATTR-CM: 41.9%).
Results
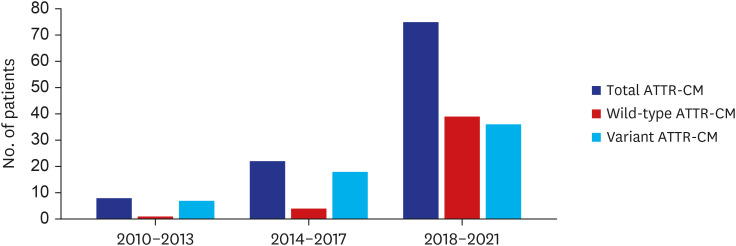
Among our cohort, 18% of the patients had a mean left ventricular (LV) wall thickness < 12 mm. The diagnosis of ATTR-CM increased notably during the study period (8 [7.6%] during 2010–2013 vs. 22 [21.0%] during 2014–2017 vs. 75 [71.4%] during 2018–2021). Although the duration between symptom onset and diagnosis did not differ, the proportion of patients with HF presenting mild symptoms increased during the study period (25% NYHA class I/II between 2010–2013 to 77% between 2018–2021). In contrast to other international registry data, male predominance was less prominent in wild-type ATTR-CM (68.2%). The distribution of TTR variants was also different from Western countries and from Japan. Asp38Ala was the most common mutation.
Conclusion
A nationwide cohort of ATTR-CM exhibited less male predominance, a proportion of patients without increased LV wall thickness, and distinct characteristics of genetic mutations, compared to cohorts in other parts of the world. Our results highlight the ethnic variation in ATTR-CM and may contribute to improving the screening process for ATTR-CM in the Asian population.
Figure
Reference
-
1. Writing Committee. Kittleson MM, Ruberg FL, Ambardekar AV, Brannagan TH, Cheng RK, et al. 2023 ACC Expert Consensus decision pathway on comprehensive multidisciplinary care for the patient with cardiac amyloidosis: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2023; 81(11):1076–1126. PMID: 36697326.2. Kittleson MM, Maurer MS, Ambardekar AV, Bullock-Palmer RP, Chang PP, Eisen HJ, et al. Cardiac amyloidosis: evolving diagnosis and management: a scientific statement from the American Heart Association. Circulation. 2020; 142(1):e7–e22. PMID: 32476490.3. Ruberg FL, Grogan M, Hanna M, Kelly JW, Maurer MS. Transthyretin amyloid cardiomyopathy: JACC State-of-the-Art Review. J Am Coll Cardiol. 2019; 73(22):2872–2891. PMID: 31171094.4. Yingchoncharoen T, Wu TC, Choi DJ, Ong TK, Liew HB, Cho MC. Economic burden of heart failure in asian countries with different healthcare systems. Korean Circ J. 2021; 51(8):681–693. PMID: 34227265.5. Park JJ, Lee CJ, Park SJ, Choi JO, Choi S, Park SM, et al. Heart failure statistics in Korea, 2020: a report from the Korean Society of Heart Failure. Int J Heart Fail. 2021; 3(4):224–236. PMID: 36262554.6. Lee HH, Cho SM, Lee H, Baek J, Bae JH, Chung WJ, et al. Korea Heart Disease Fact Sheet 2020: analysis of nationwide data. Korean Circ J. 2021; 51(6):495–503. PMID: 34085422.7. Kim D, Choi JO, Kim K, Kim SJ, Kim JS, Jeon ES. Clinical and prognostic implications of capillary density in patients with cardiac light chain amyloidosis. ESC Heart Fail. 2021; 8(6):5594–5599. PMID: 34528755.8. Gillmore JD, Maurer MS, Falk RH, Merlini G, Damy T, Dispenzieri A, et al. Nonbiopsy diagnosis of cardiac transthyretin amyloidosis. Circulation. 2016; 133(24):2404–2412. PMID: 27143678.9. Maurer MS, Schwartz JH, Gundapaneni B, Elliott PM, Merlini G, Waddington-Cruz M, et al. Tafamidis treatment for patients with transthyretin amyloid cardiomyopathy. N Engl J Med. 2018; 379(11):1007–1016. PMID: 30145929.10. Dasgupta NR, Rissing SM, Smith J, Jung J, Benson MD. Inotersen therapy of transthyretin amyloid cardiomyopathy. Amyloid. 2020; 27(1):52–58. PMID: 31713445.11. Perugini E, Guidalotti PL, Salvi F, Cooke RM, Pettinato C, Riva L, et al. Noninvasive etiologic diagnosis of cardiac amyloidosis using 99mTc-3,3-diphosphono-1,2-propanodicarboxylic acid scintigraphy. J Am Coll Cardiol. 2005; 46(6):1076–1084. PMID: 16168294.12. Hanna M, Ruberg FL, Maurer MS, Dispenzieri A, Dorbala S, Falk RH, et al. Cardiac scintigraphy with technetium-99m-labeled bone-seeking tracers for suspected amyloidosis: JACC Review Topic of the Week. J Am Coll Cardiol. 2020; 75(22):2851–2862. PMID: 32498813.13. Gilstrap LG, Dominici F, Wang Y, El-Sady MS, Singh A, Di Carli MF, et al. Epidemiology of cardiac amyloidosis-associated heart failure hospitalizations among fee-for-service Medicare beneficiaries in the United States. Circ Heart Fail. 2019; 12(6):e005407. PMID: 31170802.14. AbouEzzeddine OF, Davies DR, Scott CG, Fayyaz AU, Askew JW, McKie PM, et al. Prevalence of transthyretin amyloid cardiomyopathy in heart failure with preserved ejection fraction. JAMA Cardiol. 2021; 6(11):1267–1274. PMID: 34431962.15. Tanskanen M, Peuralinna T, Polvikoski T, Notkola IL, Sulkava R, Hardy J, et al. Senile systemic amyloidosis affects 25% of the very aged and associates with genetic variation in alpha2-macroglobulin and tau: a population-based autopsy study. Ann Med. 2008; 40(3):232–239. PMID: 18382889.16. Lane T, Fontana M, Martinez-Naharro A, Quarta CC, Whelan CJ, Petrie A, et al. Natural history, quality of life, and outcome in cardiac transthyretin amyloidosis. Circulation. 2019; 140(1):16–26. PMID: 31109193.17. Jang SY, Kim D, Choi JO, Jeon ES. Incidence, cause of death, and survival of amyloidosis in Korea: a retrospective population-based study. Int J Heart Fail. 2021; 3(3):172–178. PMID: 36262641.18. Kim D, Choi JO, Kim K, Kim SJ, Jeon ES. Untangling amyloidosis: recent advances in cardiac amyloidosis. Int J Heart Fail. 2020; 2(4):231–239. PMID: 36262171.19. Jung MH, Chang S, Han EJ, Youn JC. Multimodal imaging and biomarkers in cardiac amyloidosis. Diagnostics (Basel). 2022; 12(3):627. PMID: 35328180.20. Ravichandran S, Lachmann HJ, Wechalekar AD. Epidemiologic and survival trends in amyloidosis, 1987-2019. N Engl J Med. 2020; 382(16):1567–1568. PMID: 32294353.21. Dispenzieri A, Coelho T, Conceição I, Waddington-Cruz M, Wixner J, Kristen AV, et al. Clinical and genetic profile of patients enrolled in the Transthyretin Amyloidosis Outcomes Survey (THAOS): 14-year update. Orphanet J Rare Dis. 2022; 17(1):236. PMID: 35717381.22. Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015; 28(1):1–39.e14. PMID: 25559473.23. Nativi-Nicolau J, Siu A, Dispenzieri A, Maurer MS, Rapezzi C, Kristen AV, et al. Temporal trends of wild-type transthyretin amyloid cardiomyopathy in the Transthyretin Amyloidosis Outcomes Survey. JACC CardioOncol. 2021; 3(4):537–546. PMID: 34729526.24. Caponetti AG, Rapezzi C, Gagliardi C, Milandri A, Dispenzieri A, Kristen AV, et al. Sex-related risk of cardiac involvement in hereditary transthyretin amyloidosis: insights from THAOS. JACC Heart Fail. 2021; 9(10):736–746. PMID: 34391735.25. Porcari A, Razvi Y, Masi A, Patel R, Ioannou A, Rauf MU, et al. Prevalence, characteristics and outcomes of older patients with hereditary versus wild-type transthyretin amyloid cardiomyopathy. Eur J Heart Fail. 2023; 25(4):515–524. PMID: 36644836.26. Maestro-Benedicto A, Vela P, de Frutos F, Mora N, Pomares A, Gonzalez-Vioque E, et al. Frequency of hereditary transthyretin amyloidosis among elderly patients with transthyretin cardiomyopathy. Eur J Heart Fail. 2022; 24(12):2367–2373. PMID: 35999650.27. Maurer MS, Hanna M, Grogan M, Dispenzieri A, Witteles R, Drachman B, et al. Genotype and phenotype of transthyretin cardiac amyloidosis: THAOS (Transthyretin Amyloid Outcome Survey). J Am Coll Cardiol. 2016; 68(2):161–172. PMID: 27386769.28. Ioannou A, Patel RK, Razvi Y, Porcari A, Sinagra G, Venneri L, et al. Impact of earlier diagnosis in cardiac ATTR amyloidosis over the course of 20 years. Circulation. 2022; 146(22):1657–1670. PMID: 36325894.29. Winburn I, Ishii T, Sumikawa T, Togo K, Yasunaga H. Estimating the prevalence of transthyretin amyloid cardiomyopathy in a large in-hospital database in Japan. Cardiol Ther. 2019; 8(2):297–316. PMID: 31376091.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tafamidis for Cardiac Transthyretin Amyloidosis
- Familial Transthyretin Amyloidosis with Variant Asp38Ala Presenting with Orthostatic Hypotension and Chronic Diarrhea
- Tafamidis for a Transplant Patient with Transthyretin Amyloid Polyneuropathy
- A rare pathogenic variant identified in a heart transplant recipient with hereditary transthyretin amyloidosis: a case report
- A Case of a Senile Systemic Amyloidosis Patient Presenting With Angina Pectoris and Dilated Cardiomyopathy