Clin Endosc.
2024 May;57(3):293-301. 10.5946/ce.2023.051.
The role of cap-assisted endoscopy and its future implications
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Seoul St. Mary’s Hospital, The Catholic University of Korea, Seoul, Korea
- KMID: 2555889
- DOI: http://doi.org/10.5946/ce.2023.051
Abstract
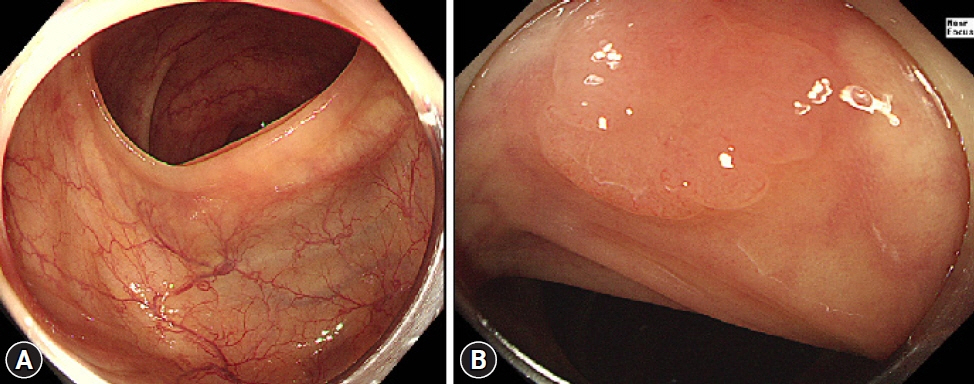
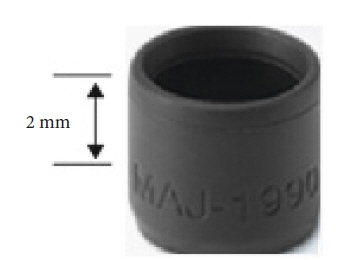
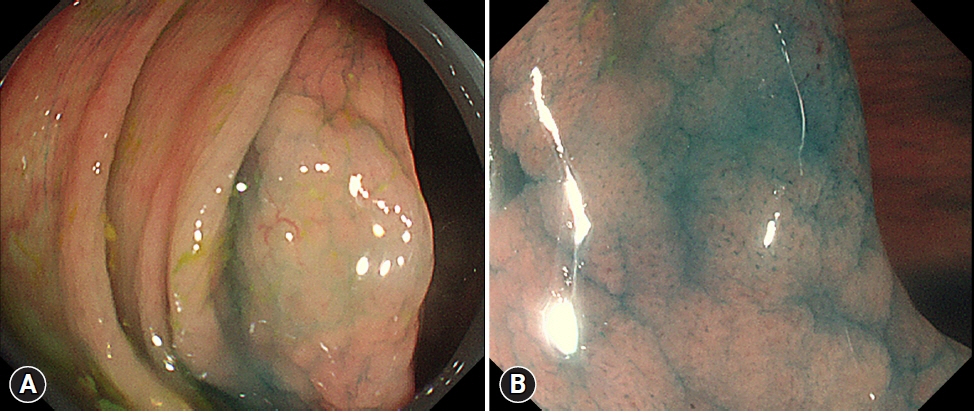
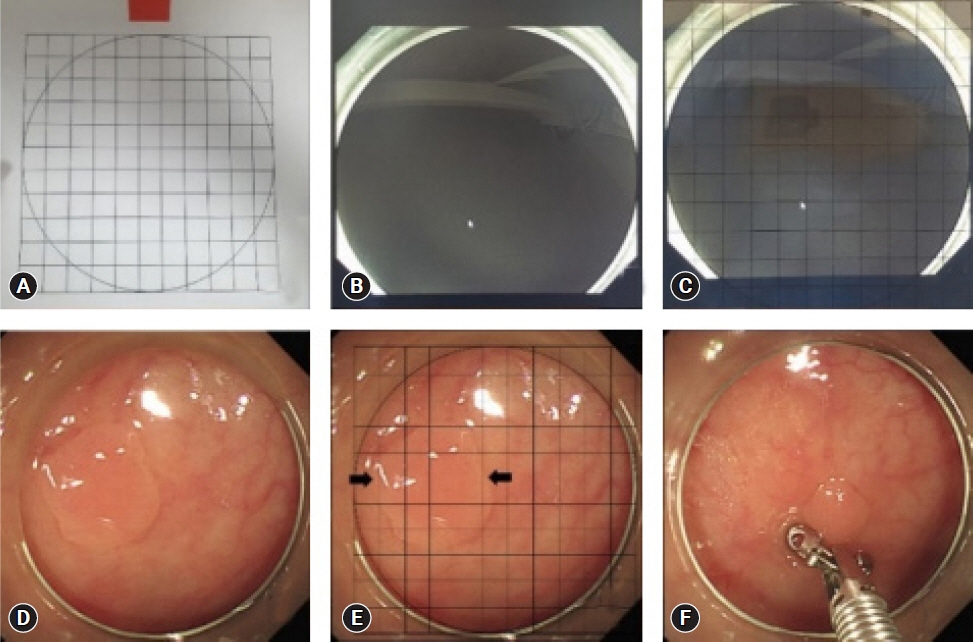
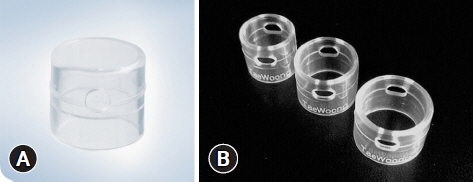
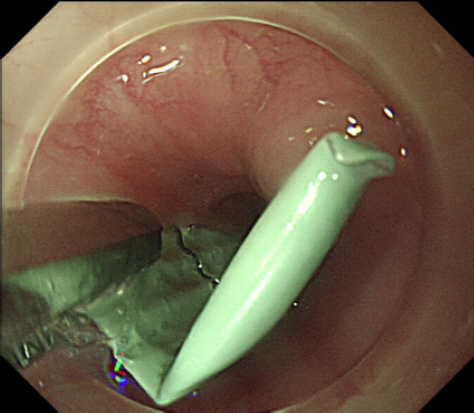
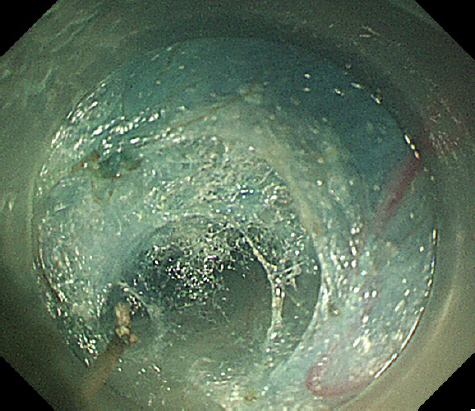
- Cap-assisted endoscopy refers to a procedure in which a short tube made of a polymer (mostly transparent) is attached to the distal tip of the endoscope to enhance its diagnostic and therapeutic capabilities. It is reported to be particularly useful in: (1) minimizing blind spots during screening colonoscopy, (2) providing a constant distance from a lesion for clear visualization during magnifying endoscopy, (3) accurately assessing the size of various gastrointestinal lesions, (4) preventing mucosal injury during foreign body removal, (5) securing adequate workspace in the submucosal space during endoscopic submucosal dissection or third space endoscopy, (6) providing an optimal approach angle to a target, and (7) suctioning mucosal and submucosal tissue with negative pressure for resection or approximation. Here, we review various applications of attachable caps in diagnostic and therapeutic endoscopy and their future implications.
Figure
Reference
-
1. Patel SG, Ahnen DJ. Prevention of interval colorectal cancers: what every clinician needs to know. Clin Gastroenterol Hepatol. 2014; 12:7–15.
Article2. Anderson R, Burr NE, Valori R. Causes of post-colonoscopy colorectal cancers based on world endoscopy organization system of analysis. Gastroenterology. 2020; 158:1287–1299.
Article3. van Rijn JC, Reitsma JB, Stoker J, et al. Polyp miss rate determined by tandem colonoscopy: a systematic review. Am J Gastroenterol. 2006; 101:343–350.4. Rex DK, Cutler CS, Lemmel GT, et al. Colonoscopic miss rates of adenomas determined by back-to-back colonoscopies. Gastroenterology. 1997; 112:24–28.5. Barclay RI, Vicari JJ, Johanson JF, et al. Variation in adenoma detection rates and colonoscopic withdrawal times during screening colonoscopy. Gastrointest Endosc. 2005; 61:AB107.6. Soetikno RM, Kaltenbach T, Rouse RV, et al. Prevalence of nonpolypoid (flat and depressed) colorectal neoplasms in asymptomatic and symptomatic adults. JAMA. 2008; 299:1027–1035.7. East JE, Saunders BP, Burling D, et al. Surface visualization at CT colonography simulated colonoscopy: effect of varying field of view and retrograde view. Am J Gastroenterol. 2007; 102:2529–2535.
Article8. Takeuchi Y, Inoue T, Hanaoka N, et al. Surveillance colonoscopy using a transparent hood and image-enhanced endoscopy. Dig Endosc. 2010; 22 Suppl 1:S47–S53.
Article9. Pohl H, Bensen SP, Toor A, et al. Cap-assisted colonoscopy and detection of adenomatous polyps (CAP) study: a randomized trial. Endoscopy. 2015; 47:891–897.
Article10. Kim SY, Park HJ, Kim HS, et al. Cap-assisted chromoendoscopy using a mounted cap versus standard colonoscopy for adenoma detection. Am J Gastroenterol. 2020; 115:465–472.
Article11. Ng SC, Tsoi KK, Hirai HW, et al. The efficacy of cap-assisted colonoscopy in polyp detection and cecal intubation: a meta-analysis of randomized controlled trials. Am J Gastroenterol. 2012; 107:1165–1173.
Article12. Desai M, Sanchez-Yague A, Choudhary A, et al. Impact of cap-assisted colonoscopy on detection of proximal colon adenomas: systematic review and meta-analysis. Gastrointest Endosc. 2017; 86:274–281.
Article13. Westwood DA, Alexakis N, Connor SJ. Transparent cap-assisted colonoscopy versus standard adult colonoscopy: a systematic review and meta-analysis. Dis Colon Rectum. 2012; 55:218–225.14. Nutalapati V, Kanakadandi V, Desai M, et al. Cap-assisted colonoscopy: a meta-analysis of high-quality randomized controled trials. Endosc Int Open. 2018; 6:E1214–E1223.15. Singh R, Owen V, Shonde A, et al. White light endoscopy, narrow band imaging and chromoendoscopy with magnification in diagnosing colorectal neoplasia. World J Gastrointest Endosc. 2009; 1:45–50.
Article16. Yao K, Anagnostopoulos GK, Ragunath K. Magnifying endoscopy for diagnosing and delineating early gastric cancer. Endoscopy. 2009; 41:462–467.
Article17. Hirano A, Yao K, Ishihara H, et al. Nature of a white opaque substance visualized by magnifying endoscopy in colorectal hyperplastic polyps. Endosc Int Open. 2021; 9:E1077–E1083.
Article18. Ferlitsch M, Moss A, Hassan C, et al. Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2017; 49:270–297.
Article19. Kaz AM, Anwar A, O'Neill DR, et al. Use of a novel polyp "ruler snare" improves estimation of colon polyp size. Gastrointest Endosc. 2016; 83:812–816.
Article20. Jin HY, Leng Q. Use of disposable graduated biopsy forceps improves accuracy of polyp size measurements during endoscopy. World J Gastroenterol. 2015; 21:623–628.
Article21. Watanabe T, Kume K, Yoshikawa I, et al. Usefulness of a novel calibrated hood to determine indications for colon polypectomy: visual estimation of polyp size is not accurate. Int J Colorectal Dis. 2015; 30:933–938.
Article22. Leng Q, Jin HY. Measurement system that improves the accuracy of polyp size determined at colonoscopy. World J Gastroenterol. 2015; 21:2178–2182.
Article23. Han SK, Kim H, Kim JW, et al. Usefulness of a colonoscopy cap with an external grid for the measurement of small-sized colorectal polyps: a prospective randomized trial. J Clin Med. 2021; 10:2365.
Article24. Ooi M, Young EJ, Nguyen NQ. Effectiveness of a cap-assisted device in the endoscopic removal of food bolus obstruction from the esophagus. Gastrointest Endosc. 2018; 87:1198–1203.
Article25. Fang R, Cao B, Zhang Q, et al. The role of a transparent cap in the endoscopic removal of foreign bodies in the esophagus: a propensity score-matched analysis. J Dig Dis. 2020; 21:20–28.
Article26. Nabi Z, Nageshwar Reddy D, Ramchandani M. Recent advances in third-space endoscopy. Gastroenterol Hepatol (N Y). 2018; 14:224–232.27. Nabi Z, Reddy DN. Submucosal endoscopy: the present and future. Clin Endosc. 2023; 56:23–37.
Article28. Sumiyama K, Gostout CJ, Rajan E, et al. Submucosal endoscopy with mucosal flap safety valve. Gastrointest Endosc. 2007; 65:688–694.
Article29. Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010; 42:265–271.
Article30. Han SY, Youn YH. Role of endoscopy in patients with achalasia. Clin Endosc. 2023; 56:537–545.
Article31. Inoue H, Ikeda H, Hosoya T, et al. Submucosal endoscopic tumor resection for subepithelial tumors in the esophagus and cardia. Endoscopy. 2012; 44:225–230.
Article32. Pei Q, Qiao H, Zhang M, et al. Pocket-creation method versus conventional method of endoscopic submucosal dissection for superficial colorectal neoplasms: a meta-analysis. Gastrointest Endosc. 2021; 93:1038–1046.
Article33. Ikezawa N, Toyonaga T, Tanaka S, et al. Feasibility and safety of endoscopic submucosal dissection for lesions in proximity to a colonic diverticulum. Clin Endosc. 2022; 55:417–425.
Article34. Takezawa T, Hayashi Y, Shinozaki S, et al. The pocket-creation method facilitates colonic endoscopic submucosal dissection (with video). Gastrointest Endosc. 2019; 89:1045–1053.
Article35. Miura Y, Shinozaki S, Hayashi Y, et al. Duodenal endoscopic submucosal dissection is feasible using the pocket-creation method. Endoscopy. 2017; 49:8–14.
Article36. Fuke H, Sato H, Saito K, et al. Benefits and limitations of endoscopic hemostasis for upper gastrointestinal bleeding with clipping and gelform. Gastroenterol Endosc. 1996; 38:1993–1998.37. Kim JI, Kim SS, Park S, et al. Endoscopic hemoclipping using a transparent cap in technically difficult cases. Endoscopy. 2003; 35:659–662.
Article38. Silva LC, Arruda RM, Botelho PF, et al. Cap-assisted endoscopy increases ampulla of Vater visualization in high-risk patients. BMC Gastroenterol. 2020; 20:214.
Article39. Abdelhafez M, Phillip V, Hapfelmeier A, et al. Comparison of cap-assisted endoscopy vs. side-viewing endoscopy for examination of the major duodenal papilla: a randomized, controlled, noninferiority crossover study. Endoscopy. 2019; 51:419–426.
Article40. Sanchez-Yague A, Kaltenbach T, Yamamoto H, et al. The endoscopic cap that can (with videos). Gastrointest Endosc. 2012; 76:169–178.
Article41. Soetikno RM, Gotoda T, Nakanishi Y, et al. Endoscopic mucosal resection. Gastrointest Endosc. 2003; 57:567–579.
Article42. Jensen DM, Kovacs T, Ghassemi KA, et al. Randomized controlled trial of over-the-scope clip as initial treatment of severe nonvariceal upper gastrointestinal bleeding. Clin Gastroenterol Hepatol. 2021; 19:2315–2323.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Usefulness of Cap-assisted Endoscopic Retrograde Cholangiopancreatography for Cannulation Complicated by a Periampullary Diverticulum
- Current Status and Future Trends of Cold Atmospheric Plasma as an Oncotherapy
- Cap-assisted ERCP in Surgically Altered Anatomy
- Painless Colonoscopy: Available Techniques and Instruments
- The role of small bowel endoscopy in small bowel Crohn's disease: when and how?