Brain Tumor Res Treat.
2024 Apr;12(2):115-120. 10.14791/btrt.2024.0003.
Primary Intracranial Ewing Sarcoma With an Unusual Presentation: A Case Report
- Affiliations
-
- 1Department of Neurosurgery, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 2Department of Neurosurgery, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea
- KMID: 2555870
- DOI: http://doi.org/10.14791/btrt.2024.0003
Abstract
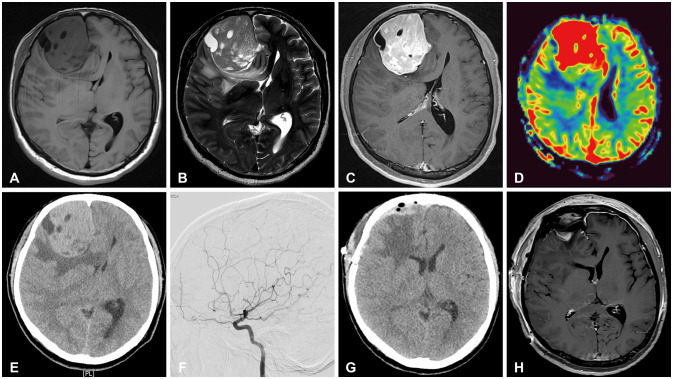
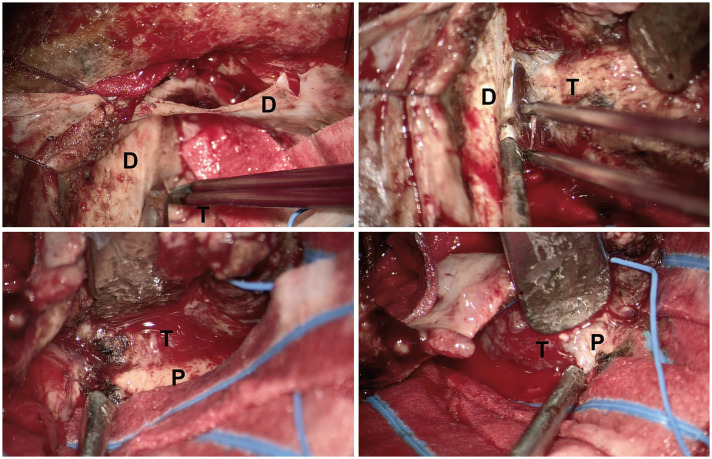
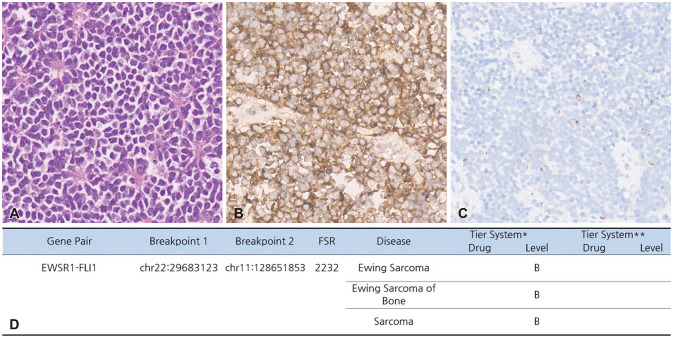
- Primary extraosseous intracranial Ewing sarcoma (ES) is an extremely rare disease, limited to the pediatric population, that primarily originates in the skull. Here, we present an unusual case of adult Ewing’s sarcoma originating from the brain parenchyma. The 50-year-old male patient visited our hospital with severe headache lasting 3 weeks. MRI presented 6.1×6.2×5.2 cm sized heterogeneously enhanced mass containing peritumoral edema in the right frontal lobe. The patient underwent right frontal craniotomy, at which time the gray and red masses adhered to the surrounding brain parenchyma. The mass was completely resected using neuronavigation and electrophysiological monitoring. Histopathological examination revealed ES-compatible findings of small round cell tumor and CD-99 positive membranous immunostaining. Next generation sequencing revealed translocation and fusion of EWSR1 and FLI1, consistent with a confirmed diagnosis of ES. Consequently, the patient underwent postoperative radiotherapy. The present case revealed adult primary intracranial ES arising from the frontal lobe. Although its etiology remains poorly understood, intraparenchymal ES should be included in the differential diagnosis of parenchymal brain tumors.
Keyword
Figure
Reference
-
1. Haveman LM, Ranft A, Berg HVD, Klco-Brosius S, Ladenstein R, Paulussen M, et al. Primary and metastatic intracranial Ewing sarcoma at diagnosis: retrospective international study and systematic review. Cancers (Basel). 2020; 12:1675. PMID: 32599807.2. Jiang Y, Zhao L, Wang Y, Liu X, Wu X, Li Y. Primary intracranial Ewing sarcoma/peripheral primitive neuroectodermal tumor mimicking meningioma: a case report and literature review. Front Oncol. 2020; 10:528073. PMID: 33123461.3. Yim J, Lee WS, Kim SK, Kang HJ, Bae J, Park SH. Intracranial Ewing sarcoma with whole genome study. Childs Nerv Syst. 2019; 35:547–552. PMID: 30406421.4. Kumar V, Singh A, Sharma V, Kumar M. Primary intracranial dural-based Ewing sarcoma/peripheral primitive neuroectodermal tumor mimicking a meningioma: a rare tumor with review of literature. Asian J Neurosurg. 2017; 12:351–357. PMID: 28761507.5. Chen J, Jiang Q, Zhang Y, Yu Y, Zheng Y, Chen J, et al. Clinical features and long-term outcome of primary intracranial Ewing sarcoma/peripheral primitive neuroectodermal tumors: 14 cases from a single institution. World Neurosurg. 2019; 122:e1606–e1614. PMID: 30496933.6. Cherif El Asri A, Benzagmout M, Chakour K, Chaoui MF, Laaguili J, Chahdi H, et al. Primary intracranial pPNET/Ewing sarcoma: diagnosis, management, and prognostic factors dilemma–a systematic review of the literature. World Neurosurg. 2018; 115:346–356. PMID: 29729469.7. Gupta S, Kumar A, Rangari KV, Mehrotra A, Pal L, Kumar R. Intracranial peripheral primitive neuroectodermal tumor arising from the clivus with intracranial metastasis in an elderly woman: case report and review of the literature. World Neurosurg. 2018; 119:331–334. PMID: 30144615.8. VandenHeuvel KA, Al-Rohil RN, Stevenson ME, Qian J, Gross NL, McNall-Knapp R, et al. Primary intracranial Ewing’s sarcoma with unusual features. Int J Clin Exp Pathol. 2015; 8:260–274. PMID: 25755713.9. Salunke P, Sharma M, Gupta K. Ewing sarcoma of the occipital bone in an elderly patient. World Neurosurg. 2014; 81:e10–e12.10. Mellai M, Caldera V, Comino A, Fortunato M, Bernucci C, Schiffer D. PNET/ESFT of the cranial vault: a case report. Clin Neuropathol. 2010; 29:372–377. PMID: 21073841.11. Attabib NA, West M, Rhodes RH. Peripheral primitive neuroectodermal tumor of the cavernous sinus: case report. Neurosurgery. 2006; 58:E992. PMID: 16639307.12. Nakagomi T, Molnár Z, Nakano-Doi A, Taguchi A, Saino O, Kubo S, et al. Ischemia-induced neural stem/progenitor cells in the pia mater following cortical infarction. Stem Cells Dev. 2011; 20:2037–2051. PMID: 21838536.13. Ishitsuka K, Ago T, Arimura K, Nakamura K, Tokami H, Makihara N, et al. Neurotrophin production in brain pericytes during hypoxia: a role of pericytes for neuroprotection. Microvasc Res. 2012; 83:352–359. PMID: 22387236.14. Caplan AI. MSCs: the sentinel and safe-guards of injury. J Cell Physiol. 2016; 231:1413–1416. PMID: 26565391.15. Wong YL, Okubo T, Uno E, Suda K, Ishii T. Role of CD99 in regulating homeostasis and differentiation in normal human epidermal keratinocytes. Biochem Biophys Res Commun. 2022; 606:108–113. PMID: 35339749.16. Pasello M, Manara MC, Scotlandi K. CD99 at the crossroads of physiology and pathology. J Cell Commun Signal. 2018; 12:55–68. PMID: 29305692.17. Batur A. Conventional and advanced MR imaging findings of primary Ewing sarcoma of the tentorium: a case report with literature review. Br J Neurosurg. 2023; 37:1322–1325. PMID: 33410362.18. Ke Ch, Duan Q, Yang H, Zhu F, Yan M, Xu SP, et al. Meningeal Ewing sarcoma/peripheral PNET: clinicopathological, immunohistochemical and FISH study of four cases. Neuropathology. 2017; 37:35–44. PMID: 27500883.19. D’Antonio A, Caleo A, Garcia JF, Marsilia GM, De Dominicis G, Boscaino A. Primary peripheral PNET/Ewing’s sarcoma of the dura with FISH analysis. Histopathology. 2004; 45:651–654. PMID: 15569062.20. Hyun C, Lee Y, Kang H, Park HJ, Suh KJ, Choi BS, et al. Primary intracranial Ewing sarcoma with EWSR1-FLI1 gene translocation mimicking a meningioma and a multidisciplinary therapeutic approach: a case report and systematic review of literatures. Brain Tumor Res Treat. 2023; 11:281–288. PMID: 37953453.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ewing's Sarcoma Mimicking a Meningioma in Radiological Findings: A Case Report
- Primary Intradural Extraosseous Ewing's Sarcoma
- Double Primary Presentation of Liposarcoma and Ewing's Sarcoma: A Case Report
- Extraskeletal Neoplasm Resembling Ewing's Sarcoma: Case Report
- Extraskeletal Ewing's Sarcoma: A Case Report