Brain Tumor Res Treat.
2024 Apr;12(2):93-99. 10.14791/btrt.2024.0005.
Minimally Invasive Approaches in the Surgical Treatment of Intracranial Meningiomas: An Analysis of 54 Cases
- Affiliations
-
- 1General Hospital Bamberg, Bamberg, Germany
- 2University Hospital Tuebingen, Tuebingen, Germany
- 3Houston Methodist Hospital, Houston, Texas, USA
- KMID: 2555867
- DOI: http://doi.org/10.14791/btrt.2024.0005
Abstract
- Background
Intracranial meningiomas, being a fairly common disease in the population, often re-quire surgical treatment, which, in turn, can completely heal the patient. The localization of meningiomas often influences treatment even if they are asymptomatic. By modernizing approaches to surgical treatment, it is possible to minimize intra- and postoperative risks, while achieving complete removal of the tumor. One of these methods is minimally invasive neurosurgery, the development of which in recent years allows it to compete with standard surgical methods. The purpose of this study was the objectification of minimally invasive approaches, such as the calculation of the craniotomy area and the ratio of craniotomy area to the resected tumor volume.
Methods
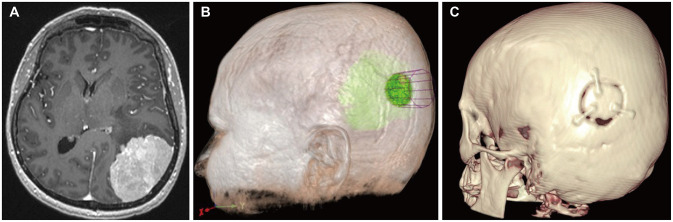
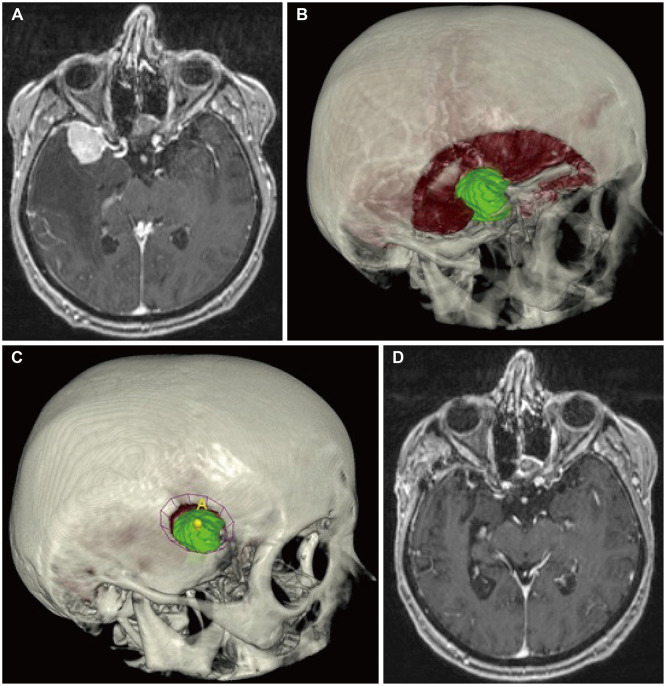
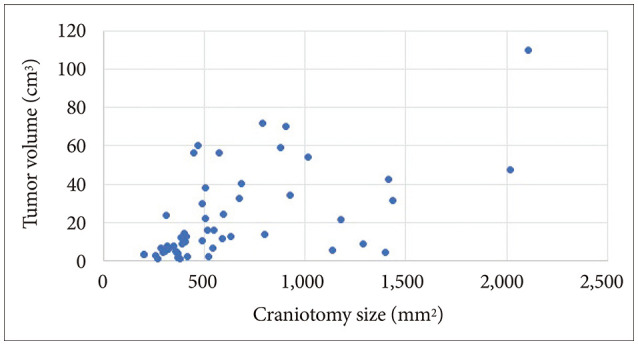
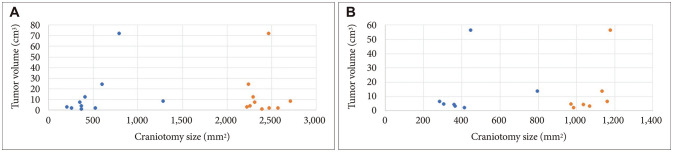
The retrospective study consisted of a group of 54 consecutive patients who were operated on in our neurosurgery clinic specialized on minimally invasive neurosurgery. Preoperative planning was carried out using the Surgical Theater visualization platform. Using this system, the tumor volume and craniotomy surface area were calculated. During the analysis, the symptoms before and after the surgery, classification of tumors, postoperative complications, further treatment and follow-up results were assessed.
Results
Twelve (22.2%) patients were men and 42 (77.8%) were women. The mean age of the group was 64.2 years (median 67.5). The craniotomy area ranged from 202 to 2,108 mm 2 (mean 631 mm 2 ). Tumor volume ranged from 0.85 to 110.1 cm 3 (mean 21.6 cm 3 ). The craniotomy size of minimally invasive approaches to the skull base was 3–5 times smaller than standard approaches. Skull base meningiomas accounted for 19 cases (35.2%), convexity meningiomas for 26 cases (48.1%), and falx and tentorium meningiomas for 9 cases (16.7%). Three complications were reported: postoperative hemorrhage, CSF leakage, and ophthalmoplegia. Relapse was detected in 2 patients with a mean follow-up of 26.3 months (median 20).
Conclusion
Minimally invasive approaches in the surgical treatment of intracranial meningiomas reduce the possibility of operating trauma by several times; they are safe and sufficient for complete removal of the tumor.
Figure
Reference
-
1. Ogasawara C, Philbrick BD, Adamson DC. Meningioma: a review of epidemiology, pathology, diagnosis, treatment, and future directions. Biomedicines. 2021; 9:319. PMID: 33801089.2. Staneczek W, Jänisch W. Epidemiologic data on meningiomas in East Germany 1961-1986: incidence, localization, age and sex distribution. Clin Neuropathol. 1992; 11:135–141. PMID: 1611725.3. Codd MB, Kurland LT. Descriptive epidemiology of primary intracranial neoplasms. Prog Exp Tumor Res. 1985; 29:1–11.4. Lee YS, Lee YS. Molecular characteristics of meningiomas. J Pathol Transl Med. 2020; 54:45–63. PMID: 31964111.5. Woehrer A, Hackl M, Waldhör T, Weis S, Pichler J, Olschowski A, et al. Relative survival of patients with non-malignant central nervous system tumours: a descriptive study by the Austrian Brain Tumour Registry. Br J Cancer. 2014; 110:286–296. PMID: 24253501.6. Zouaoui S, Darlix A, Rigau V, Mathieu-Daudé H, Bauchet F, Bessaoud F, et al. Descriptive epidemiology of 13,038 newly diagnosed and histologically confirmed meningiomas in France: 2006-2010. Neurochirurgie. 2018; 64:15–21. PMID: 26073920.7. Ostrom QT, Patil N, Cioffi G, Waite K, Kruchko C, Barnholtz-Sloan JS. CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2013-2017. Neuro Oncol. 2020; 22(Suppl 2):iv1–i96. PMID: 33123732.8. Wiemels J, Wrensch M, Claus EB. Epidemiology and etiology of meningioma. J Neurooncol. 2010; 99:307–314. PMID: 20821343.9. Huisman TW, Tanghe HL, Koper JW, Reubi JC, Foekens JA, Avezaat CJ, et al. Progesterone, oestradiol, somatostatin and epidermal growth factor receptors on human meningiomas and their CT characteristics. Eur J Cancer. 1991; 27:1453–1457. PMID: 1660295.10. Sioka C, Kyritsis AP. Chemotherapy, hormonal therapy, and immunotherapy for recurrent meningiomas. J Neurooncol. 2009; 92:1–6. PMID: 19023520.11. Onizuka M, Suyama K, Shibayama A, Hiura T, Horie N, Miyazaki H. Asymptomatic brain tumor detected at brain check-up. Neurol Med Chir (Tokyo). 2001; 41:431–434. discussion 435. PMID: 11593969.12. Tsushima Y, Taketomi-Takahashi A, Endo K. Prevalence of abnormal findings on brain magnetic resonance (MR) examinations in adult participants of brain docking. BMC Neurol. 2005; 5:18. PMID: 16207376.13. Vernooij MW, Ikram MA, Tanghe HL, Vincent AJ, Hofman A, Krestin GP, et al. Incidental findings on brain MRI in the general population. N Engl J Med. 2007; 357:1821–1828. PMID: 17978290.14. Nakamura M, Roser F, Michel J, Jacobs C, Samii M. The natural history of incidental meningiomas. Neurosurgery. 2003; 53:62–71. PMID: 12823874.15. Nakasu S, Hirano A, Shimura T, Llena JF. Incidental meningiomas in autopsy study. Surg Neurol. 1987; 27:319–322. PMID: 3824137.16. Barresi V, Caffo M, Tuccari G. Classification of human meningiomas: lights, shadows, and future perspectives. J Neurosci Res. 2016; 94:1604–1612. PMID: 27376782.17. Nanda A, Bir SC, Maiti TK, Konar SK, Missios S, Guthikonda B. Relevance of Simpson grading system and recurrence-free survival after surgery for World Health Organization Grade I meningioma. J Neurosurg. 2017; 126:201–211. PMID: 27058201.18. Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016; 131:803–820. PMID: 27157931.19. Simpson D. The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry. 1957; 20:22–39. PMID: 13406590.20. Guenther F, Swozil F, Heber S, Buchfelder M, Messlinger K, Fischer MJ. Pre- and postoperative headache in patients with meningioma. Cephalalgia. 2019; 39:533–543. PMID: 30089403.21. Wu A, Garcia MA, Magill ST, Chen W, Vasudevan HN, Perry A, et al. Presenting symptoms and prognostic factors for symptomatic outcomes following resection of meningioma. World Neurosurg. 2018; 111:e149–e159. PMID: 29248774.22. Nassiri F, Suppiah S, Wang JZ, Badhiwala JH, Juraschka K, Meng Y, et al. How to live with a meningioma: experiences, symptoms, and challenges reported by patients. Neurooncol Adv. 2020; 2:vdaa086. PMID: 32793887.23. Tucha O, Smely C, Preier M, Becker G, Paul GM, Lange KW. Preoperative and postoperative cognitive functioning in patients with frontal meningiomas. J Neurosurg. 2003; 98:21–31.24. Whittle IR, Smith C, Navoo P, Collie D. Meningiomas. Lancet. 2004; 363:1535–1543. PMID: 15135603.25. Beaumont A, Whittle IR. The pathogenesis of tumour associated epilepsy. Acta Neurochir (Wien). 2000; 142:1–15. PMID: 10664370.26. Englot DJ, Magill ST, Han SJ, Chang EF, Berger MS, McDermott MW. Seizures in supratentorial meningioma: a systematic review and meta-analysis. J Neurosurg. 2016; 124:1552–1561. PMID: 26636386.27. Lühdorf K, Jensen LK, Plesner AM. Etiology of seizures in the elderly. Epilepsia. 1986; 27:458–463. PMID: 3720706.28. Goldbrunner R, Minniti G, Preusser M, Jenkinson MD, Sallabanda K, Houdart E, et al. EANO guidelines for the diagnosis and treatment of meningiomas. Lancet Oncol. 2016; 17:e383–e391. PMID: 27599143.29. Black PM. Meningiomas. Neurosurgery. 1993; 32:643–657. PMID: 8474655.30. Mirimanoff RO, Dosoretz DE, Linggood RM, Ojemann RG, Martuza RL. Meningioma: analysis of recurrence and progression following neurosurgical resection. J Neurosurg. 1985; 62:18–24. PMID: 3964853.31. Roberti F, Sekhar LN, Kalavakonda C, Wright DC. Posterior fossa meningiomas: surgical experience in 161 cases. Surg Neurol. 2001; 56:8–20. PMID: 11546562.32. Thakur JD, Mallari RJ, Corlin A, Yawitz S, Huang W, Eisenberg A, et al. Minimally invasive surgical treatment of intracranial meningiomas in elderly patients (≥ 65 years): outcomes, readmissions, and tumor control. Neurosurg Focus. 2020; 49:E17.33. Kreissl MC, Hänscheid H, Löhr M, Verburg FA, Schiller M, Lassmann M, et al. Combination of peptide receptor radionuclide therapy with fractionated external beam radiotherapy for treatment of advanced symptomatic meningioma. Radiat Oncol. 2012; 7:99. PMID: 22720902.34. Yao A, Sarkiss CA, Lee J, Zarzour HK, Shrivastava RK. Surgical limitations in convexity meningiomas en-plaque: is radical resection necessary? J Clin Neurosci. 2016; 27:28–33. PMID: 26778515.35. Zhao L, Zhao W, Hou Y, Wen C, Wang J, Wu P, et al. An overview of managements in meningiomas. Front Oncol. 2020; 10:1523. PMID: 32974188.36. Haddad AF, Young JS, Kanungo I, Sudhir S, Chen JS, Raleigh DR, et al. WHO grade I meningioma recurrence: identifying high risk patients using histopathological features and the MIB-1 index. Front Oncol. 2020; 10:1522. PMID: 32983999.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic Resection of Presacral Tumor: A New Approach in the Era of the Minimally Invasive Surgery
- Superciliary Keyhole Approach for Unruptured Anterior Circulation Aneurysms: Surgical Technique, Indications, and Contraindications
- Multiple Intracranial Meningiomas: Case Report
- A New Beginning for the Journal of Minimally Invasive Surgery for the International Recognition and Contribution of Scientific Development of Minimally Invasive Surgery
- Visualizing kidney transplant techniques: a comparative study of open and robotic surgery