J Korean Assoc Oral Maxillofac Surg.
2024 Apr;50(2):110-115. 10.5125/jkaoms.2024.50.2.110.
Anatomical study to determine a new approach to treat benign masses located in the anterior condyle region: a case report
- Affiliations
-
- 1Life Dental Clinic, Seoul, 2 Snow Dental Clinic, Seoul, Korea
- 2Kangdong Sacred Heart Hospital, Seoul, 4 Life Dental Clinic, Yangpyeong, Korea
- KMID: 2555741
- DOI: http://doi.org/10.5125/jkaoms.2024.50.2.110
Abstract
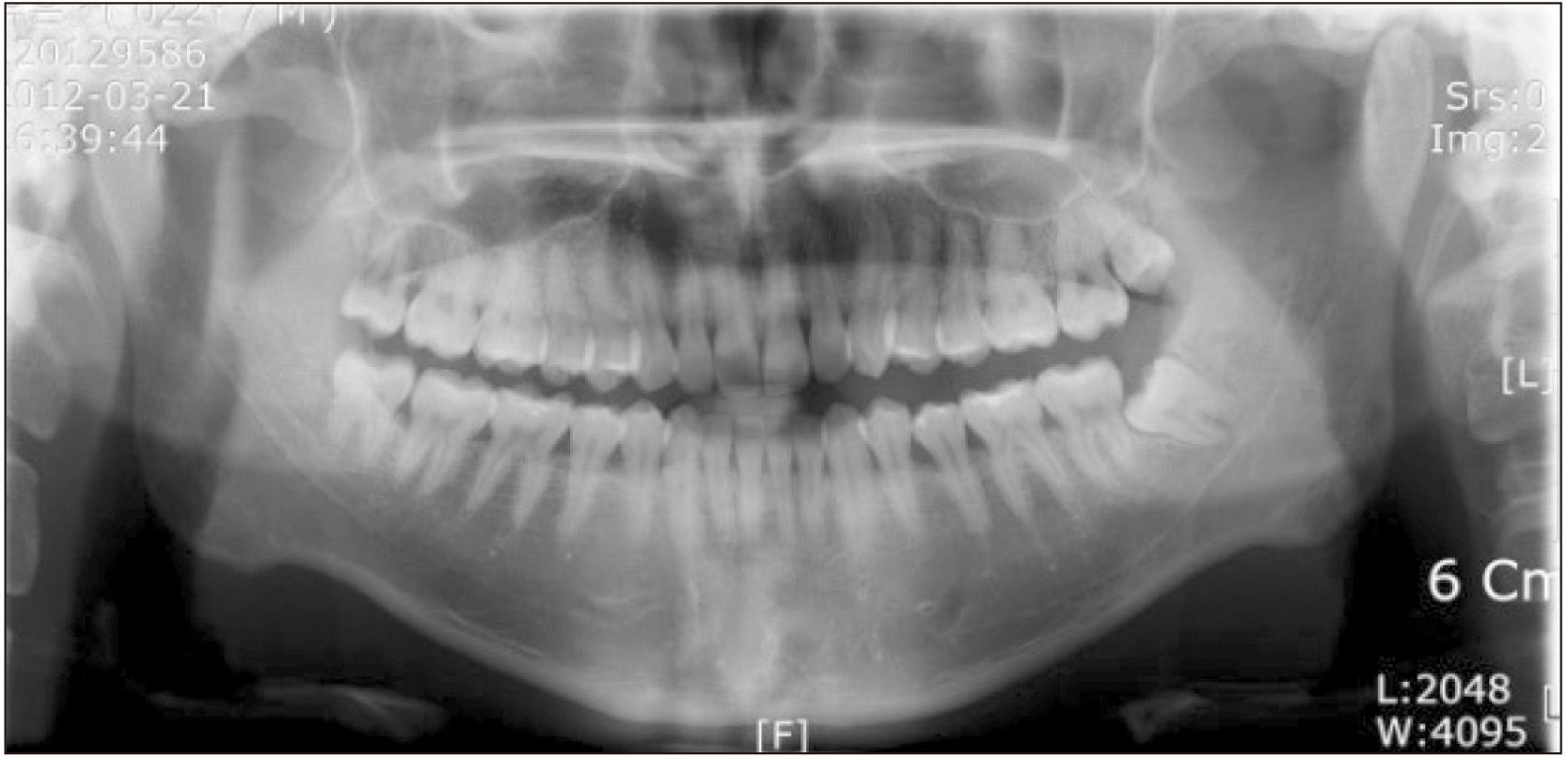
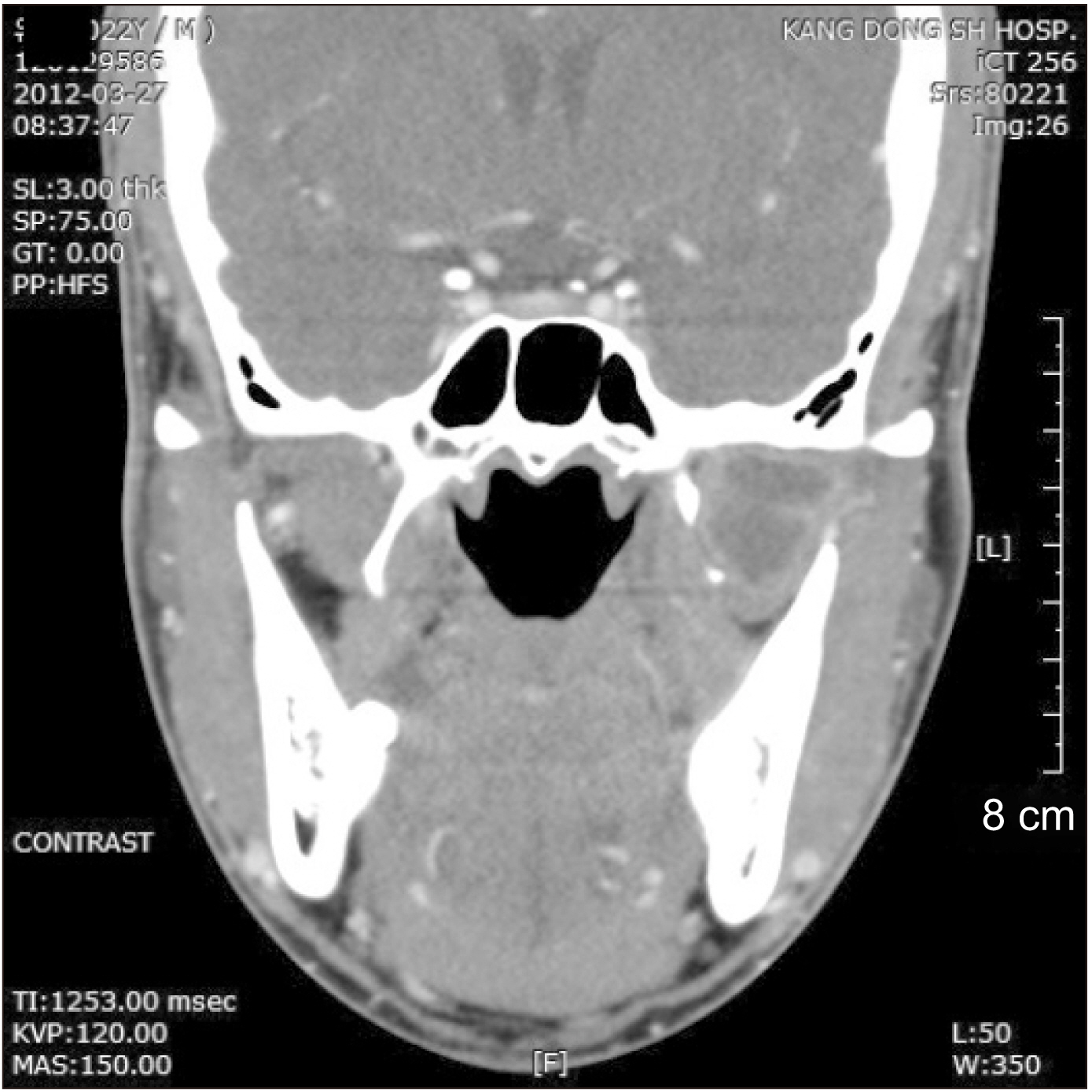
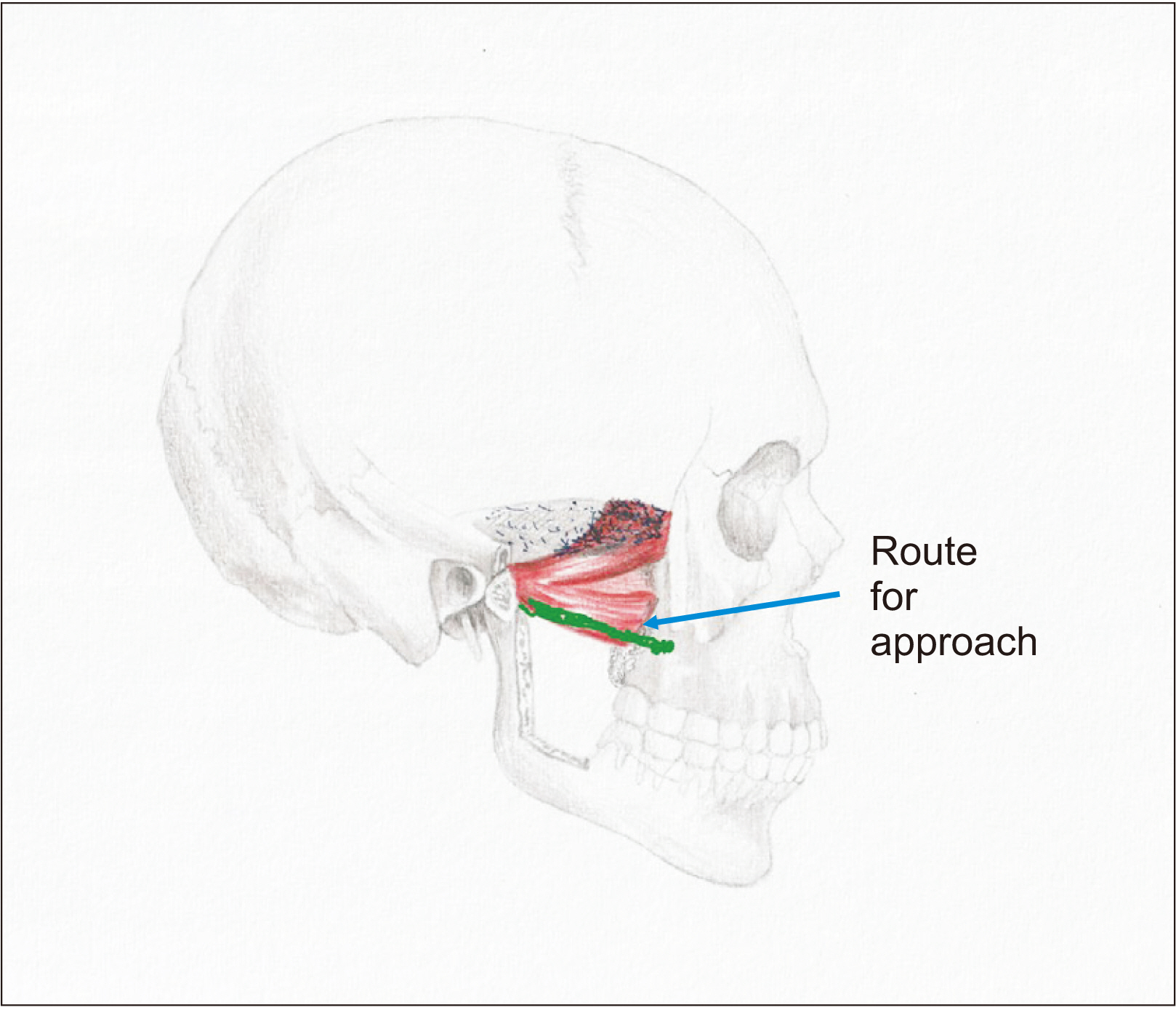
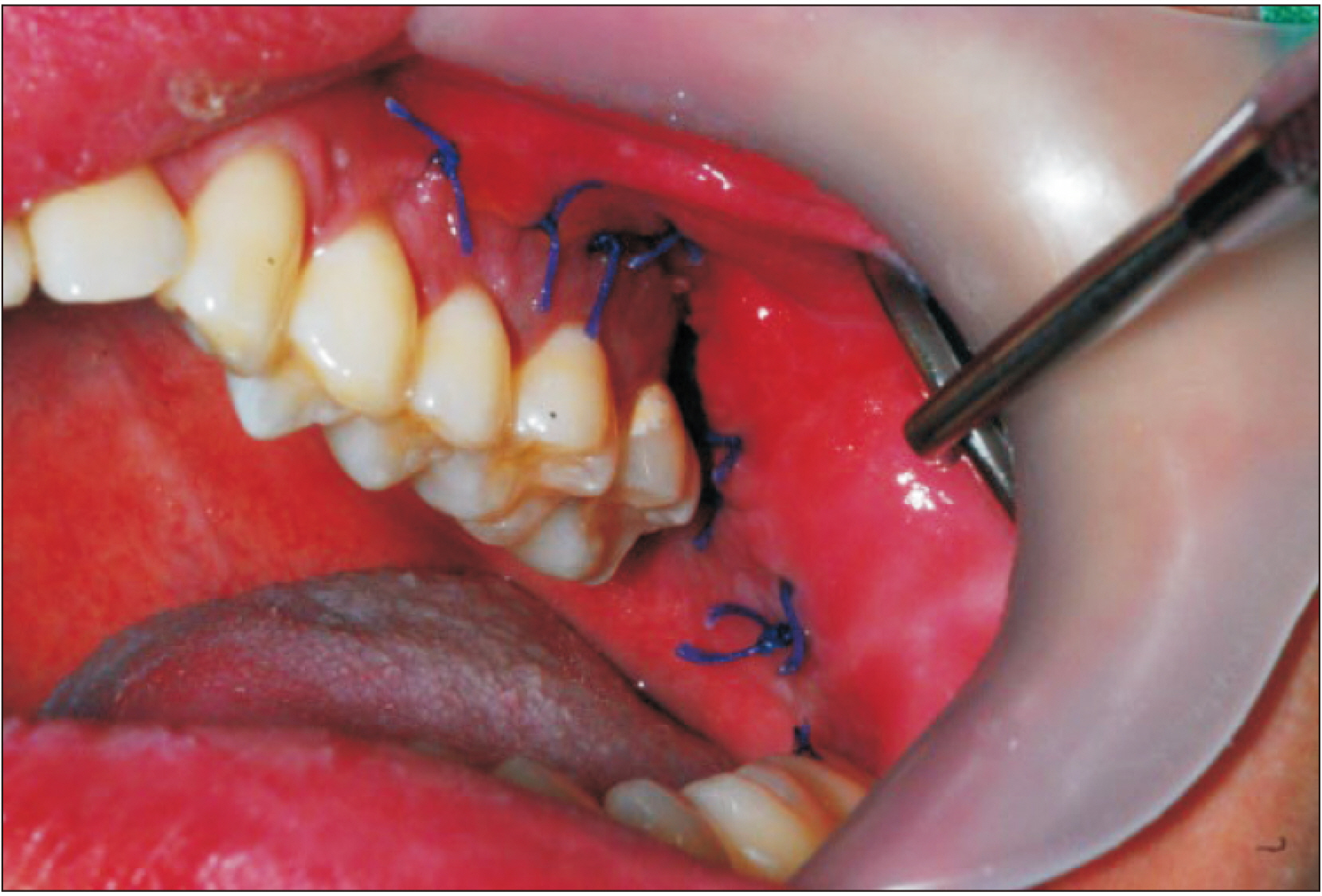
- A 22-year-old male patient presented to the clinic with severe pain in the preauricular area with an inability to completely occlude the jaw. Facial computed tomography and magnetic resonance imaging revealed a well-defined lesion that was tentatively diagnosed as a benign tumor or cystic mass. Surgical approach of a lesion in the condyle is delicate and problematic as many vulnerable anatomical structures are present. There are several methods for surgery in this area. Typically, an extraoral approach is dangerous because of potential injuries to nerves and arteries. The intraoral approach also presents difficulties due to the lack of visibility and accessibility. On occasion, coronoidectomy may be performed. The goal here was to determine an easier and safer new surgical approach to the condyle. We reached the anterior part of the pterygoid plate in the same method as in Le Fort I surgery. From this point, through the external pterygoid muscle, approaching the anterior aspect of the condyle is relatively easy and safe, with minimal damage to the surrounding tissues. Pus was drained at the site, and the lesion was diagnosed as an abscess. Pain and inability to close the mouth resolved without recurrence.
Keyword
Figure
Reference
-
References
1. Sear AJ. 1972; Intra-oral condylectomy applied to unilateral condylar hyperplasia. Br J Oral Surg. 10:143–53. https://doi.org/10.1016/s0007-117x(72)80030-1. DOI: 10.1016/S0007-117X(72)80030-1. PMID: 4509977.
Article2. Eller DJ, Blakemore JR, Stein M, Byers S. 1977; Transoral resection of a condylar osteochondroma: report of case. J Oral Surg. 35:409–13.3. Kreutziger KL. 1984; Surgery of the temporomandibular joint. I. Surgical anatomy and surgical incisions. Oral Surg Oral Med Oral Pathol. 58:637–46. https://doi.org/10.1016/0030-4220(84)90027-6. DOI: 10.1016/0030-4220(84)90027-6. PMID: 6594653.
Article4. Vallerand WP, Dolwick MF. 1990; Complications of temporomandibular joint surgery. Oral Maxillofac Surg Clin North Am. 2:481–8.5. Keith DA. 2003; Complications of temporomandibular joint surgery. Oral Maxillofac Surg Clin North Am. 15:187–94. https://doi.org/10.1016/s1042-3699(03)00016-5. DOI: 10.1016/S1042-3699(03)00016-5. PMID: 18088674.
Article6. Knepil GJ, Kanatas AN, Loukota RJ. 2011; Classification of surgical approaches to the mandibular condyle. Br J Oral Maxillofac Surg. 49:664–5. https://doi.org/10.1016/j.bjoms.2011.02.009. DOI: 10.1016/j.bjoms.2011.02.009. PMID: 21453998.
Article7. Vesnaver A. 2008; Open reduction and internal fixation of intra-articular fractures of the mandibular condyle: our first experiences. J Oral Maxillofac Surg. 66:2123–9. https://doi.org/10.1016/j.joms.2008.06.010. DOI: 10.1016/j.joms.2008.06.010. PMID: 18848112.
Article8. Vesnaver A, Ahčan U, Rozman J. 2012; Evaluation of surgical treatment in mandibular condyle fractures. J Craniomaxillofac Surg. 40:647–53. https://doi.org/10.1016/j.jcms.2011.10.029. DOI: 10.1016/j.jcms.2011.10.029. PMID: 22079126.
Article9. Trost O, Trouilloud P, Malka G. 2009; Open reduction and internal fixation of low subcondylar fractures of mandible through high cervical transmasseteric anteroparotid approach. J Oral Maxillofac Surg. 67:2446–51. https://doi.org/10.1016/j.joms.2009.04.109. DOI: 10.1016/j.joms.2009.04.109. PMID: 19837315.
Article10. Narayanan V, Kannan R, Sreekumar K. 2009; Retromandibular approach for reduction and fixation of mandibular condylar fractures: a clinical experience. Int J Oral Maxillofac Surg. 38:835–9. https://doi.org/10.1016/j.ijom.2009.04.008. DOI: 10.1016/j.ijom.2009.04.008. PMID: 19467846.
Article11. Choi EJ, Cha IH, Nam W. 2011; The result of endoscope-assisted open reduction and internal fixation (EAORIF) of lateral overridden subcondyle fracture. J Korean Assoc Oral Maxillofac Surg. 37:62–6. https://doi.org/10.5125/jkaoms.2011.37.1.62. DOI: 10.5125/jkaoms.2011.37.1.62.
Article12. Trost O, Abu El-Naaj I, Trouilloud P, Danino A, Malka G. 2008; High cervical transmasseteric anteroparotid approach for open reduction and internal fixation of condylar fracture. J Oral Maxillofac Surg. 66:201–4. https://doi.org/10.1016/j.joms.2006.09.031. DOI: 10.1016/j.joms.2006.09.031. PMID: 18083441.
Article13. Shi J, Yuan H, Xu B. 2013; Treatment of mandibular condyle fractures using a modified transparotid approach via the parotid mini-incision: experience with 31 cases. PLoS One. 8:e83525. https://doi.org/10.1371/journal.pone.0083525. DOI: 10.1371/journal.pone.0083525. PMID: 24386221. PMCID: PMC3873388.
Article14. Guo Y, Guo C. 2014; Maxillary-fronto-temporal approach for removal of recurrent malignant infratemporal fossa tumors: anatomical and clinical study. J Craniomaxillofac Surg. 42:206–12. https://doi.org/10.1016/j.jcms.2013.05.001. DOI: 10.1016/j.jcms.2013.05.001. PMID: 23932542.
Article15. Utumi ER, Pedron IG, Perrella A, Zambon CE, Ceccheti MM, Cavalcanti MG. 2010; Osteochondroma of the temporomandibular joint: a case report. Braz Dent J. 21:253–8. https://doi.org/10.1590/s0103-64402010000300014. DOI: 10.1590/S0103-64402010000300014. PMID: 21203710.
Article16. Yun KI, Park MK, Kim CH, Park JU. 2008; Chondrosarcoma in the mandibular condyle: case report. J Korean Oral Maxillofac Surg. 34:95–8.17. Ryu DM, Kim HJ, Lee SC, Kim YG, Lee BS. 2002; Osteochonrdoma of the mandibular condyle: a case report. J Korean Oral Maxillofac Surg. 28:132–5.18. Deng M, Long X, Cheng AH, Cheng Y, Cai H. 2009; Modified trans-oral approach for mandibular condylectomy. Int J Oral Maxillofac Surg. 38:374–7. https://doi.org/10.1016/j.ijom.2009.01.020. DOI: 10.1016/j.ijom.2009.01.020. PMID: 19282151.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Treatment of Osteochondroma on the Mandibular Condyle through Intraoral Approach: Case Report
- Testicular Necrosis after Ilioinguinal Approach for Pelvic Nonunion: A Case Report
- Clinical and anatomical importance of foramen magnum and craniocervical junction structures in the perspective of surgical approaches
- Surgical excision of osteochondroma on mandibular condyle via preauricular approach with zygomatic arch osteotomy
- Osteochondroma and synovial chondromatosis of the temporomandibular joint