Korean Circ J.
2024 Apr;54(4):189-200. 10.4070/kcj.2023.0268.
The Association of CHADS-P2A2RC Risk Score With Clinical Outcomes in Patients Taking P2Y12 Inhibitor Monotherapy After 3 Months of Dual Antiplatelet Therapy Following Percutaneous Coronary Intervention
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Chungnam National University Hospital, Chungnam National University College of Medicine, Daejeon, Korea
- 2Division of Cardiology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Division of Cardiology, Department of Internal Medicine, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea
- 4Division of Cardiology, Department of Internal Medicine, Keimyung University Dongsan Medical Center, Daegu, Korea
- 5Department of Internal Medicine, Chungbuk National University Hospital, Chungbuk National University College of Medicine, Cheongju, Korea
- KMID: 2555531
- DOI: http://doi.org/10.4070/kcj.2023.0268
Abstract
- Background and Objectives
Concerns remain that early aspirin cessation may be associated with potential harm in subsets at high risk of ischemic events. This study aimed to assess the effects of P2Y12 inhibitor monotherapy after 3-month dual antiplatelet therapy (DAPT) vs. prolonged DAPT (12-month or longer) based on the ischemic risk stratification, the CHADSP2A2RC, after percutaneous coronary intervention (PCI).
Methods
This was a sub-study of the SMART-CHOICE trial. The effect of the randomized antiplatelet strategies was assessed across 3 CHADS-P2A2RC risk score categories. The primary outcome was a major adverse cardiac and cerebral event (MACCE), a composite of all-cause death, myocardial infarction, or stroke.
Results
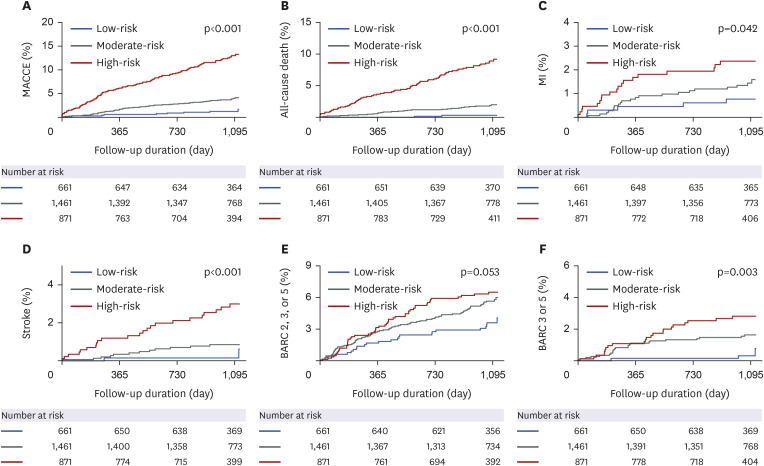
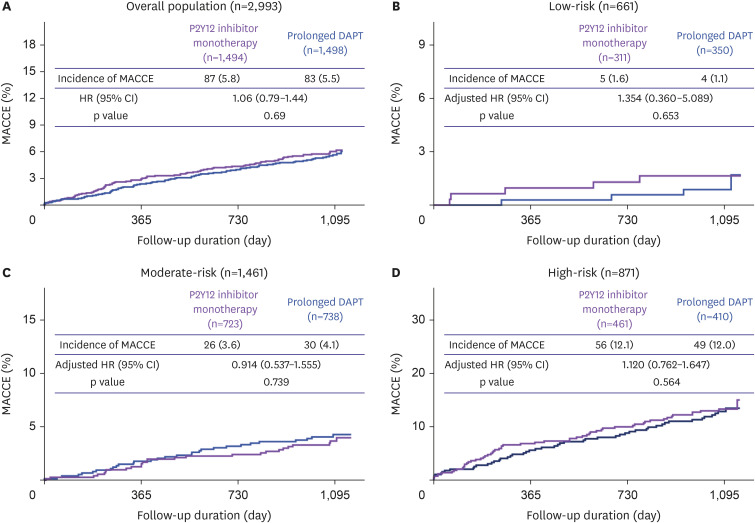
Up to 3 years, the high CHADS-P2A2RC risk score group had the highest incidence of MACCE (105 [12.1%], adjusted hazard ratio [HR], 2.927; 95% confidence interval [CI], 1.358–6.309; p=0.006) followed by moderate-risk (40 [1.4%], adjusted HR, 1.786; 95% CI, 0.868–3.674; p=0.115) and low-risk (9 [0.5%], reference). In secondary analyses, P2Y12 inhibitor monotherapy reduced the Bleeding Academic Research Consortium (BARC) types 2, 3, or 5 bleeding without increasing the risk of MACCE as compared with prolonged DAPT across the 3 CHADS-P2A2RC risk strata without significant interaction term (interaction p for MACCE=0.705 and interaction p for BARC types 2, 3, or 5 bleeding=0.055).
Conclusions
The CHADS-P2A2RC risk score is valuable in discriminating high-ischemicrisk patients. Even in such patients with a high risk of ischemic events, P2Y12 inhibitor monotherapy was associated with a lower incidence of bleeding without increased risk of ischemic events compared with prolonged DAPT.
Figure
Reference
-
1. Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: executive summary: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2022; 145:e4–17. PMID: 34882436.2. Collet JP, Thiele H, Barbato E, et al. 2020 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021; 42:1289–1367. PMID: 32860058.3. Sinnaeve PR, Adriaenssens T. Dual antiplatelet therapy de-escalation strategies. Am J Cardiol. 2021; 144(Suppl 1):S23–S31. PMID: 33706987.4. Palmerini T, Bruno AG, Redfors B, et al. Risk-benefit of 1-year DAPT after DES implantation in patients stratified by bleeding and ischemic risk. J Am Coll Cardiol. 2021; 78:1968–1986. PMID: 34763774.5. Natsuaki M, Morimoto T, Yamaji K, et al. Prediction of thrombotic and bleeding events after percutaneous coronary intervention: CREDO-Kyoto thrombotic and bleeding risk scores. J Am Heart Assoc. 2018; 7:e008708. PMID: 29789335.6. Simonsson M, Alfredsson J, Szummer K, Jernberg T, Ueda P. Association of ischemic and bleeding events with mortality among patients in Sweden with recent acute myocardial infarction receiving antithrombotic therapy. JAMA Netw Open. 2022; 5:e2220030. PMID: 36036452.7. Park JS, Jeong YH. Unguided de-escalation strategy from potent P2Y12 inhibitors in patients presented with ACS: when, whom and how? Korean Circ J. 2022; 52:320–323. PMID: 35388998.8. Capodanno D, Bhatt DL, Gibson CM, et al. Bleeding avoidance strategies in percutaneous coronary intervention. Nat Rev Cardiol. 2022; 19:117–132. PMID: 34426673.9. Steensig K, Olesen KK, Madsen M, et al. A novel model for prediction of thromboembolic and cardiovascular events in patients without atrial fibrillation. Am J Cardiol. 2020; 131:40–48. PMID: 32718550.10. Song YB, Oh SK, Oh JH, et al. Rationale and design of the comparison between a P2Y12 inhibitor monotherapy versus dual antiplatelet therapy in patients undergoing implantation of coronary drug-eluting stents (SMART-CHOICE): a prospective multicenter randomized trial. Am Heart J. 2018; 197:77–84. PMID: 29447787.11. Choi KH, Park YH, Song YB, et al. Long-term effects of P2Y12 inhibitor monotherapy after percutaneous coronary intervention: 3-year follow-up of the SMART-CHOICE randomized clinical trial. JAMA Cardiol. 2022; 7:1100–1108. PMID: 36169938.12. Capodanno D, Morice MC, Angiolillo DJ, et al. Trial design principles for patients at high bleeding risk undergoing PCI: JACC scientific expert panel. J Am Coll Cardiol. 2020; 76:1468–1483. PMID: 32943165.13. Knuuti J, Wijns W, Saraste A, et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020; 41:407–477. PMID: 31504439.14. Würtz M, Olesen KK, Mortensen MB, et al. Dual antithrombotic treatment in chronic coronary syndrome: European Society of Cardiology criteria vs. CHADS-P2A2RC score. Eur Heart J. 2022; 43:996–1004. PMID: 34871376.15. Leiter LA, Bhatt DL, McGuire DK, et al. Diabetes-related factors and the effects of ticagrelor plus aspirin in the THEMIS and THEMIS-PCI trials. J Am Coll Cardiol. 2021; 77:2366–2377. PMID: 33985681.16. Zhu H, Xu X, Fang X, et al. Efficacy and safety of long-term antithrombotic strategies in patients with chronic coronary syndrome: a network meta-analysis of randomized controlled trials. J Am Heart Assoc. 2021; 10:e019184. PMID: 33682435.17. Armstrong PC, Dhanji AR, Truss NJ, et al. Utility of 96-well plate aggregometry and measurement of thrombi adhesion to determine aspirin and clopidogrel effectiveness. Thromb Haemost. 2009; 102:772–778. PMID: 19806265.18. Armstrong PC, Dhanji AR, Tucker AT, Mitchell JA, Warner TD. Reduction of platelet thromboxane A2 production ex vivo and in vivo by clopidogrel therapy. J Thromb Haemost. 2010; 8:613–615. PMID: 19995405.19. Armstrong PC, Leadbeater PD, Chan MV, et al. In the presence of strong P2Y12 receptor blockade, aspirin provides little additional inhibition of platelet aggregation. J Thromb Haemost. 2011; 9:552–561. PMID: 21143373.20. Kinlay S, Quach L, Cormack J, et al. Premature discontinuation of dual antiplatelet therapy after coronary stenting in veterans: characteristics and long-term outcomes. J Am Heart Assoc. 2021; 10:e018481. PMID: 33899501.21. Dehghani P, Cao D, Baber U, et al. Ticagrelor monotherapy after PCI in patients with concomitant diabetes mellitus and chronic kidney disease: TWILIGHT DM-CKD. Eur Heart J Cardiovasc Pharmacother. 2022; 8:707–716. PMID: 35325085.22. Giustino G, Chieffo A, Palmerini T, et al. Efficacy and safety of dual antiplatelet therapy after complex PCI. J Am Coll Cardiol. 2016; 68:1851–1864. PMID: 27595509.23. Gragnano F, Mehran R, Branca M, et al. P2Y12 inhibitor monotherapy or dual antiplatelet therapy after complex percutaneous coronary interventions. J Am Coll Cardiol. 2023; 81:537–552. PMID: 36754514.24. Lee YJ, Suh Y, Kim JS, et al. Ticagrelor monotherapy after 3-month dual antiplatelet therapy in acute coronary syndrome by high bleeding risk: the subanalysis from the TICO trial. Korean Circ J. 2022; 52:324–337. PMID: 35129317.25. Park MW. Balancing between ischemic and bleeding risk in PCI patients with ‘bi-risk’. Korean Circ J. 2022; 52:338–340. PMID: 35388999.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Role of P2Y12 Inhibitor Monotherapy in Patients With Coronary Artery Disease Undergoing Percutaneous Coronary Intervention
- Recent Evidence of Potent P2Y12 Inhibitor Monotherapy After Short-term Dual Antiplatelet Therapy for Patients With Acute Coronary Syndrome
- Sex-Based Outcomes of P2Y12 Inhibitor Monotherapy After Three Months of Dual Antiplatelet Therapy in Patients Undergoing Percutaneous Coronary Intervention
- De-escalation strategies of dual antiplatelet therapy in patients undergoing percutaneous coronary intervention for acute coronary syndrome
- Dual Antiplatelet Therapy after Noncardioembolic Ischemic Stroke or Transient Ischemic Attack: Pros and Cons