Obstet Gynecol Sci.
2024 May;67(3):335-338. 10.5468/ogs.23287.
Prognosis of subsequent pregnancy in uterine necrosis after uterine artery embolization
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Bucheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Bucheon, Korea
- 2Department of Obstetrics and Gynecology, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Pathology, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Department of Radiology, Bucheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Bucheon, Korea
- KMID: 2555517
- DOI: http://doi.org/10.5468/ogs.23287
Abstract
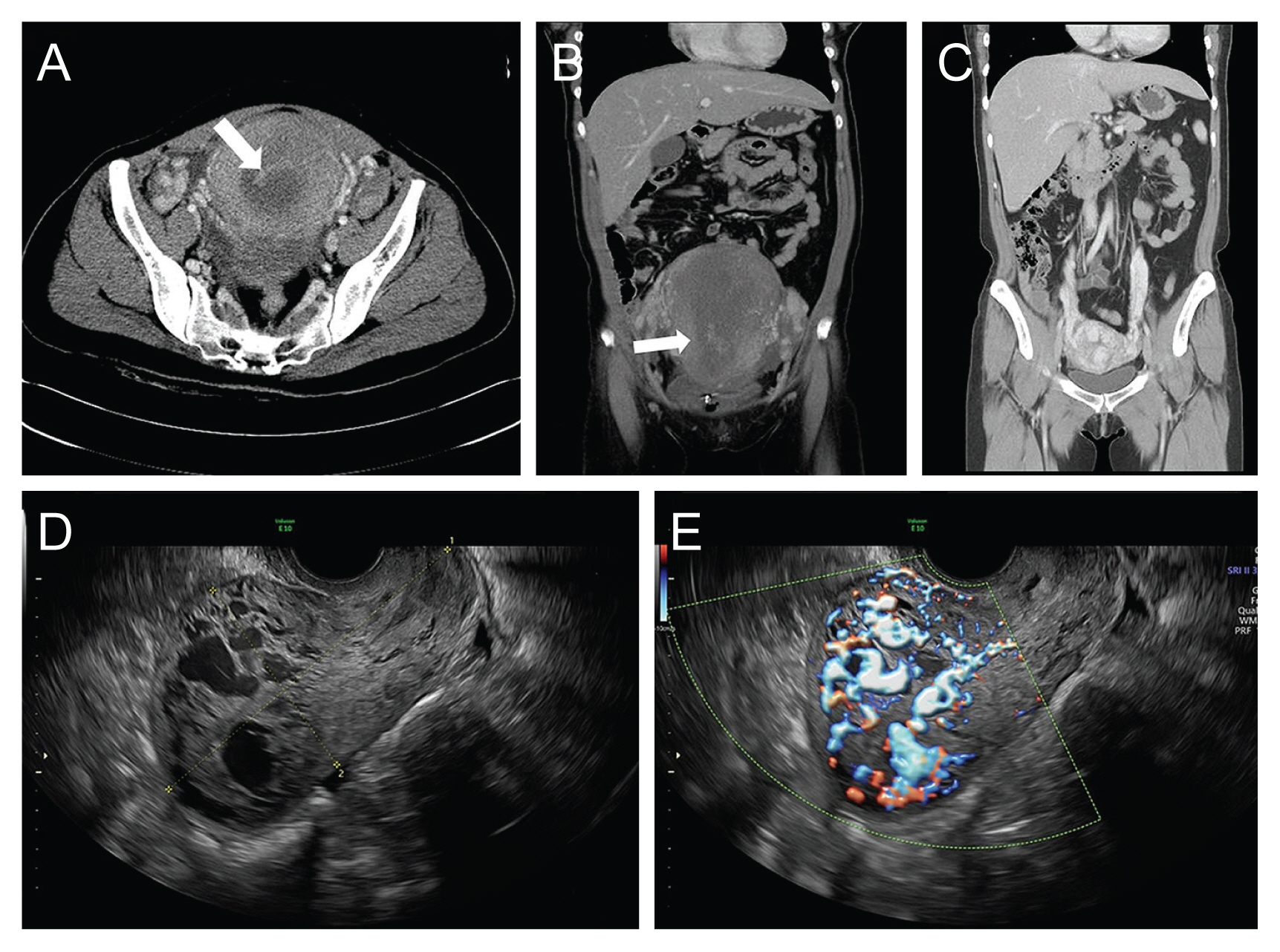
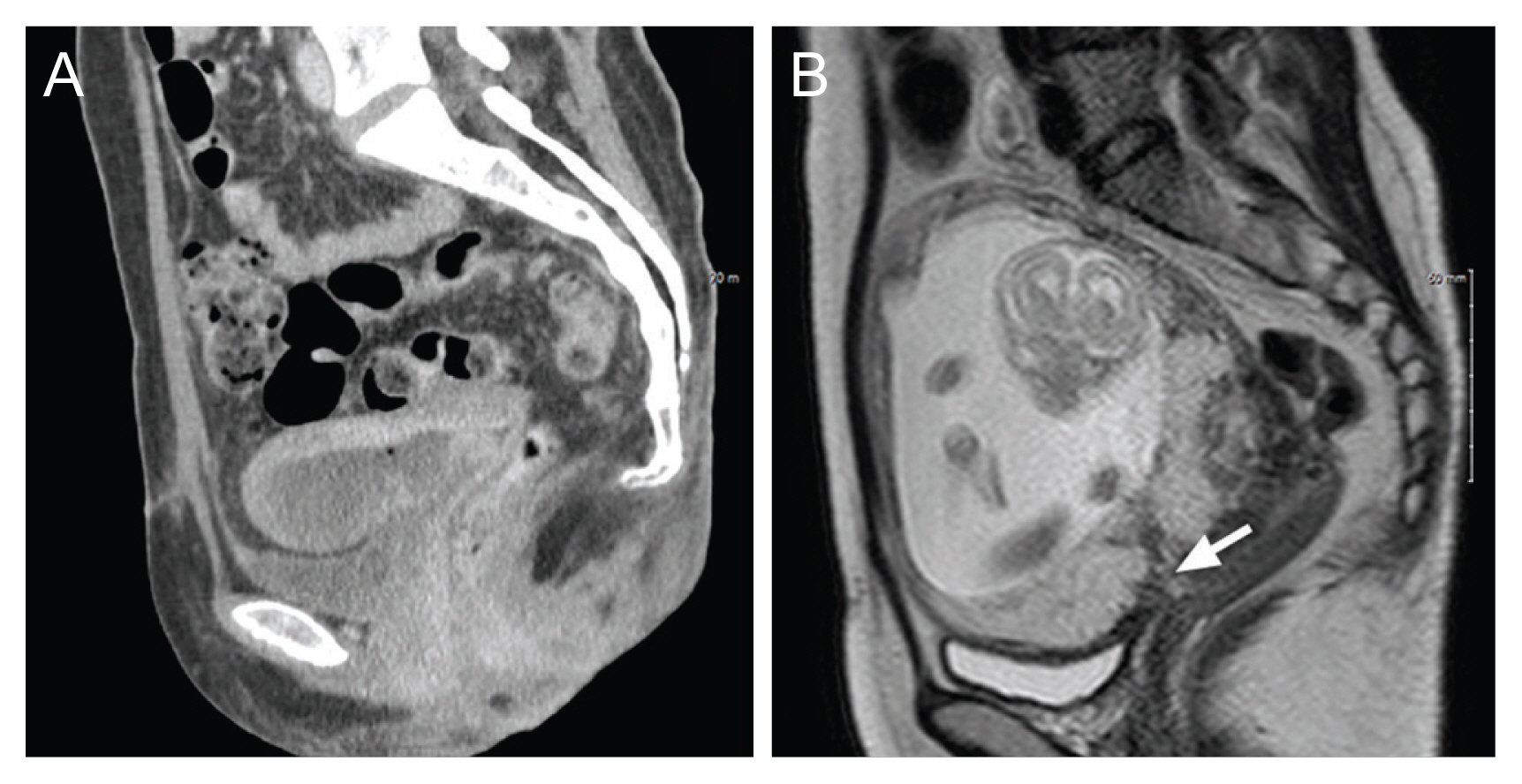
- In an 8-year period at two medical center, 138 patients underwent uterine artery embolization, and 11 of them were diagnosed with uterine necrosis. Among them, three were successfully conceived. However, one of them developed an arteriovenous malformation after an artificial abortion, and another experienced complications, including placenta previa and placenta accreta spectrum, which resulted in early preterm delivery and recurrent postpartum hemorrhage, necessitating subtotal hysterectomy. Therefore, it is crucial to prepare for potential adverse pregnancy outcomes in subsequent pregnancies for patients with a history of uterine necrosis.
Figure
Reference
-
References
1. Kim MJ, Kim IJ, Kim S, Park IY. Postpartum hemorrhage with uterine artery embolization: the risk of complications of uterine artery embolization. Minim Invasive Ther Allied Technol. 2022; 31:276–83.2. Brown M, Hong M Jr, Lindquist J. Uterine artery embolization for primary postpartum hemorrhage. Tech Vasc Interv Radiol. 2021; 24:100727.
Article3. Inoue S, Masuyama H, Hiramatsu Y. Efficacy of transarterial embolisation in the management of post-partum haemorrhage and its impact on subsequent pregnancies. Aust N Z J Obstet Gynaecol. 2014; 54:541–5.4. Poggi SH, Yaeger A, Wahdan Y, Ghidini A. Outcome of pregnancies after pelvic artery embolization for postpartum hemorrhage: retrospective cohort study. Am J Obstet Gynecol. 2015; 213:576.e1–5.5. Matsuzaki S, Lee M, Nagase Y, Jitsumori M, Matsuzaki S, Maeda M, et al. A systematic review and meta-analysis of obstetric and maternal outcomes after prior uterine artery embolization. Sci Rep. 2021; 11:16914.6. Salomon LJ, deTayrac R, Castaigne-Meary V, Audibert F, Musset D, Ciorascu R, et al. Fertility and pregnancy outcome following pelvic arterial embolization for severe post-partum haemorrhage. A cohort study. Hum Reprod. 2003; 18:849–52.7. Boulleret C, Chahid T, Gallot D, Mofid R, Tran Hai D, Ravel A, et al. Hypogastric arterial selective and superselective embolization for severe postpartum hemorrhage: a retrospective review of 36 cases. Cardiovasc Intervent Radiol. 2004; 27:344–8.8. Cheong JY, Kong TW, Son JH, Won JH, Yang JI, Kim HS. Outcome of pelvic arterial embolization for postpartum hemorrhage: a retrospective review of 117 cases. Obstet Gynecol Sci. 2014; 57:17–27.9. Holub Z, Mara M, Kuzel D, Jabor A, Maskova J, Eim J. Pregnancy outcomes after uterine artery occlusion: prospective multicentric study. Fertil Steril. 2008; 90:1886–91.10. Jitsumori M, Matsuzaki S, Endo M, Hara T, Tomimatsu T, Matsuzaki S, et al. Obstetric outcomes of pregnancy after uterine artery embolization. Int J Womens Health. 2020; 12:151–8.11. Piñas Carrillo A, Chandraharan E. Placenta accreta spectrum: risk factors, diagnosis and management with special reference to the triple P procedure. Womens Health (Lond). 2019; 15:1745506519878081.12. Lee JY, Hwang JY, Lee HA, Lee DH, Lee SK. Uterine necrosis after partial obstruction of the uterine artery via selective embolization in postpartum hemorrhage: a case report. Korean J Obstet Gynecol. 2009; 52:576–80.13. Poujade O, Ceccaldi PF, Davitian C, Amate P, Chatel P, Khater C, et al. Uterine necrosis following pelvic arterial embolization for post-partum hemorrhage: review of the literature. Eur J Obstet Gynecol Reprod Biol. 2013; 170:309–14.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous Uterine Rupture after Uterine Artery Embolization for the Treatment of Uterine Myomas
- Uterine necrosis after partial obstruction of the uterine artery via selective embolization in postpartum hemorrhage: A case report
- A Case of Uterine Fibroids Necrosis after Transarterial Embolization for Treatment of Uterine Fibroids
- A case of preoperative angiographic uterine artery embolization for the conservative treatment of cervical pregnancy
- Uterine Necrosis after Uterine Artery Embolization for Postpartum Hemorrhage