Obstet Gynecol Sci.
2024 May;67(3):323-334. 10.5468/ogs.23212.
Analyze, design, develop, implement, and evaluate approach to develop a pelvic floor muscle training guidebook to treat stress urinary incontinence in women
- Affiliations
-
- 1Urogynecology Division, Department of Obstetrics and Gynecology, Dr. Cipto Mangunkusumo Hospital, Jakarta, Indonesia
- 2Faculty of Medicine, University of Indonesia, Jakarta, Indonesia
- 3Department of Urology, Dr. Cipto Mangunkusumo Hospital, Jakarta, Indonesia
- 4Geriatrics Division, Department of Internal Medicine, Dr. Cipto Mangunkusumo Hospital, Jakarta, Indonesia
- 5Department of Physical Medicine and Rehabilitation, Dr. Cipto Mangunkusumo Hospital, Jakarta, Indonesia
- 6Urogynecology Division, Department of Obstetrics and Gynecology, Dr. Kariadi Hospital, Semarang, Indonesia
- 7Department of Community Medicine, Dr. Cipto Mangunkusumo Hospital, Jakarta, Indonesia
- 8Department of Physiology and Biophysics, Faculty of Medicine University of Indonesia, Jakarta, Indonesia
- 9Dermatology and Venereology, Dr. Cipto Mangunkusumo Hospital, Jakarta, Indonesia
- KMID: 2555516
- DOI: http://doi.org/10.5468/ogs.23212
Abstract
Objective
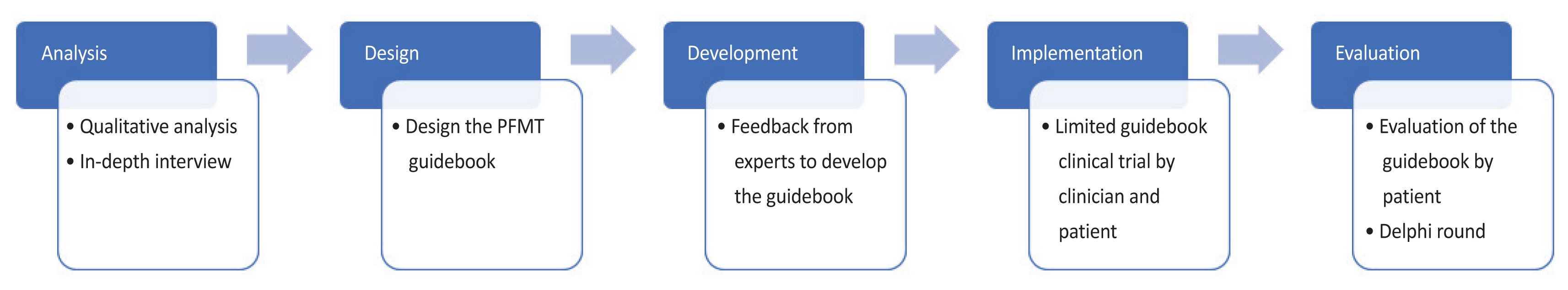
Stress urinary incontinence (SUI) is a common problem that affects the quality of life of women worldwide. Pelvic floor muscle training (PFMT) is an effective conservative first-line treatment for SUI. However, low compliance with PFMT is one of the main reasons for therapeutic failure. Indirect supervision using a guidebook may improve PFMT outcomes. To develop a PFMT guidebook using the analyze, design, development, implementation, and evaluation (ADDIE) method.
Methods
A guidebook was developed from July 2020 to April 2021 using the ADDIE method. This prospective study used mixed methods, namely qualitative analysis, focus group discussions, and in-depth interviews, and involved various experts from urogynecology, urology, medical rehabilitation, and physiotherapy departments. A pilot study was conducted on patients with SUI to evaluate the effectiveness of the guidebook.
Results
The ADDIE method was successfully implemented to develop the PFMT guidebook. The formative evaluation of the ADDIE steps mainly focused on the PFMT technique, content clarity, illustration, design, and color choice of the book. After the pilot study, the guidebook significantly improved Incontinence Impact Questionnaire, Short Form, 1-hour pad test, and perineometer scores. However, the pilot study showed no significant improvement in Urogenital Distress Inventory, Short Form scores.
Conclusion
The PFMT guidebook developed using the ADDIE method improved outcomes in patients with SUI.
Figure
Reference
-
References
1. Liu B, Wang L, Huang SS, Wu Q, Wu DL. Prevalence and risk factors of urinary incontinence among Chinese women in Shanghai. Int J Clin Exp Med. 2014; 7:686–96.2. Sumardi R, Mochtar CA, Junizaf , Santoso BI, Setiati S, Nuhonni SA, et al. Prevalence of urinary incontinence, risk factors and its impact: multivariate analysis from Indonesian nationwide survey. Acta Med Indones. 2014; 46:175–82.3. Luber KM. The definition, prevalence, and risk factors for stress urinary incontinence. Rev Urol. 2004; 6(Suppl 3):S3–9.4. Rubilotta E, Balzarro M, D’Amico A, Cerruto MA, Bassi S, Bovo C, et al. Pure stress urinary incontinence: analysis of prevalence, estimation of costs, and financial impact. BMC Urol. 2019; 19:44.
Article5. Health Mo. Standar tarif pelayanan kesehatan dalam penyelenggaraan program Jaminan Kesehatan. 1st ed. Jakarta: Minister of Health;2016.6. Dumoulin C, Cacciari LP, Hay-Smith EJC. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2018; 10:CD005654.
Article7. Huang YC, Chang KV. Kegel exercises [Internet]. Treasure Island (FL): StatPearls Publishing;c2022. [cited 2022 Oct 1]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK555898/.8. Neumann PB, Grimmer KA, Deenadayalan Y. Pelvic floor muscle training and adjunctive therapies for the treatment of stress urinary incontinence in women: a systematic review. BMC Womens Health. 2006; 6:11.
Article9. García-Sánchez E, Ávila-Gandía V, López-Román J, Martínez-Rodríguez A, Rubio-Arias JÁ. What pelvic floor muscle training load is optimal in minimizing urine loss in women with stress urinary incontinence? A systematic review and meta-analysis. Int J Environ Res Public Health. 2019; 16:4358.
Article10. Okeke H, Ifediora L, Ogungbe C. Knowledge and practice of pelvic floor muscle exercises among pregnant women in Enugu Metropolis, Nigeria. Womens Health Rep (New Rochelle). 2020; 1:444–50.
Article11. Barton A, Serrao C, Thompson J, Briffa K. Transabdominal ultrasound to assess pelvic floor muscle performance during abdominal curl in exercising women. Int Urogynecol J. 2015; 26:1789–95.
Article12. Paiva LL, Ferla L, Darski C, Catarino BM, Ramos JG. Pelvic floor muscle training in groups versus individual or home treatment of women with urinary incontinence: systematic review and meta-analysis. Int Urogynecol J. 2017; 28:351–9.
Article13. Cross D, Waheed N, Krake M, Gahreman D. Effectiveness of supervised Kegel exercises using bio-feedback versus unsupervised Kegel exercises on stress urinary incontinence: a quasi-experimental study. Int Urogynecol J. 2023; 34:913–20.
Article14. Widdison R, Rashidi A, Whitehead L. Effectiveness of mobile apps to improve urinary incontinence: a systematic review of randomised controlled trials. BMC Nurs. 2022; 21:32.
Article15. Ackah M, Ameyaw L, Salifu MG, OseiYeboah C, Serwaa Ampomaa Agyemang A, Acquaah K, et al. Estimated burden, and associated factors of urinary incontinence among Sub-Saharan African women aged 15–100 years: a systematic review and meta-analysis. PLOS Glob Public Health. 2022; 2:e0000562.
Article16. Branch R. Instructional design: the ADDIE approach. 1st ed. New York: Springer New York;2009.17. de Assis LC, Bernardes JM, Barbosa AM, Santini AC, Vianna LS, Dias A. Effectiveness of an illustrated home exercise guide on promoting urinary continence during pregnancy: a pragmatic randomized clinical trial. Rev Bras Ginecol Obstet. 2015; 37:460–6.
Article18. Malan Z, Mash B, Everett-Murphy K. Development of a training programme for primary care providers to counsel patients with risky lifestyle behaviours in South Africa. Afr J Prim Health Care Fam Med. 2015; 7:819.
Article19. Battles JB. Improving patient safety by instructional systems design. Qual Saf Health Care. 2006; 15(Suppl 1):i25–9.
Article20. Kittell-Limerick P. Perceived barriers to completion of the academic doctorate: a Delphi study. 1st ed. Texas: Texas A & M University-Commerce;2005.21. Giannarou L, Zervas E. Using Delphi technique to build consensus in practice. IJBSAM. 2014; 9:65–82.22. Rortveit G, Subak LL, Thom DH, Creasman JM, Vittinghoff E, Van Den Eeden SK, et al. Urinary incontinence, fecal incontinence and pelvic organ prolapse in a population-based, racially diverse cohort: prevalence and risk factors. Female Pelvic Med Reconstr Surg. 2010; 16:278–83.23. Indonesia PK. Panduan Tata Laksana. Inkontinensia Urine pada Dewasa. 1st ed. Jakarta: Ikatan Ahli Urologi Indonesia;2018.24. Kahyaoglu Sut H, Balkanli Kaplan P. Effect of pelvic floor muscle exercise on pelvic floor muscle activity and voiding functions during pregnancy and the postpartum period. Neurourol Urodyn. 2016; 35:417–22.
Article25. Chen L, Chen X, Luo D, Jin M, Hu Y, Cai W. Performance of self-reported and unsupervised antenatal pelvic floor muscle training and its effects on postpartum stress urinary incontinence among Chinese women: a cohort study. J Int Med Res. 2020; 48:300060520914226.
Article26. Al Belushi ZI, Al Kiyumi MH, Al-Mazrui AA, Jaju S, Alrawahi AH, Al Mahrezi AM. Effects of home-based pelvic floor muscle training on decreasing symptoms of stress urinary incontinence and improving the quality of life of urban adult Omani women: a randomized controlled single-blind study. Neurourol Urodyn. 2020; 39:1557–66.
Article27. Hoff Brækken I, Majida M, Engh ME, Bø K. Morphological changes after pelvic floor muscle training measured by 3-dimensional ultrasonography: a randomized controlled trial. Obstet Gynecol. 2010; 115:317–24.28. Leme Nagib AB, Riccetto C, Martinho NM, Camargos Pennisi PR, Blumenberg C, Paranhos LR, et al. Use of mobile apps for controlling of the urinary incontinence: a systematic review. Neurourol Urodyn. 2020; 39:1036–48.
Article29. Moroni RM, Magnani PS, Haddad JM, Castro Rde A, Brito LG. Conservative treatment of stress urinary incontinence: a systematic review with meta-analysis of randomized controlled trials. Rev Bras Ginecol Obstet. 2016; 38:97–111.
Article30. Sheng Y, Carpenter JS, Ashton-Miller JA, Miller JM. Mechanisms of pelvic floor muscle training for managing urinary incontinence in women: a scoping review. BMC Womens Health. 2022; 22:161.
Article31. Bø K, Haakstad LA. Is pelvic floor muscle training effective when taught in a general fitness class in pregnancy? A randomised controlled trial. Physiotherapy. 2011; 97:190–5.
Article32. Kaya S, Akbayrak T, Gursen C, Beksac S. Short-term effect of adding pelvic floor muscle training to bladder training for female urinary incontinence: a randomized controlled trial. Int Urogynecol J. 2015; 26:285–93.
Article33. Celiker Tosun O, Kaya Mutlu E, Ergenoglu AM, Yeniel AO, Tosun G, Malkoc M, et al. Does pelvic floor muscle training abolish symptoms of urinary incontinence? A randomized controlled trial. Clin Rehabil. 2015; 29:525–37.
Article34. Mørkved S, Bø K. Effect of pelvic floor muscle training during pregnancy and after childbirth on prevention and treatment of urinary incontinence: a systematic review. Br J Sports Med. 2014; 48:299–310.
Article35. Sun ZJ, Zhu L, Liang ML, Xu T, Lang JH. Comparison of outcomes between postpartum and non-postpartum women with stress urinary incontinence treated with conservative therapy: a prospective cohort study. Neurourol Urodyn. 2018; 37:1426–33.
Article36. Dinc A, Kizilkaya Beji N, Yalcin O. Effect of pelvic floor muscle exercises in the treatment of urinary incontinence during pregnancy and the postpartum period. Int Urogynecol J Pelvic Floor Dysfunct. 2009; 20:1223–3.
Article37. Hakim S. Buku panduan latihan Kegel pada perempuan untuk terapi inkontinensia urin tipe tekanan [Internet]. Jakarta: Universitas Indonesia;c2022. [cited 2022 Aug 2]. Available from: https://scholar.ui.ac.id/en/publications/buku-panduan-latihan-kegel-pada-perempuan-untuk-terapi-inkontinen.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pelvic floor muscle rehabilitation
- The Effects of Pelvic Floor Muscle Exercise on Urinary Symptoms and Quality of Life in Women with Stress Urinary Incontinence
- The Effect of Pelvic Floor Muscle Training with Biofeedback and Functional Electrical Stimulation for Genuine Stress Urinary Incontinence
- The Effect of Pelvic Muscle Exercise Program on Women with Stress Urinary Incontinence in the Degree and Amount of Urinary Incontinence and Maximum Vaginal Contraction Pressure
- Assessment of Pelvic Floor Muscle Exercise using Vaginal Cone in Stress Urinary Incontinence of Korea Women