Obstet Gynecol Sci.
2024 May;67(3):304-313. 10.5468/ogs.23268.
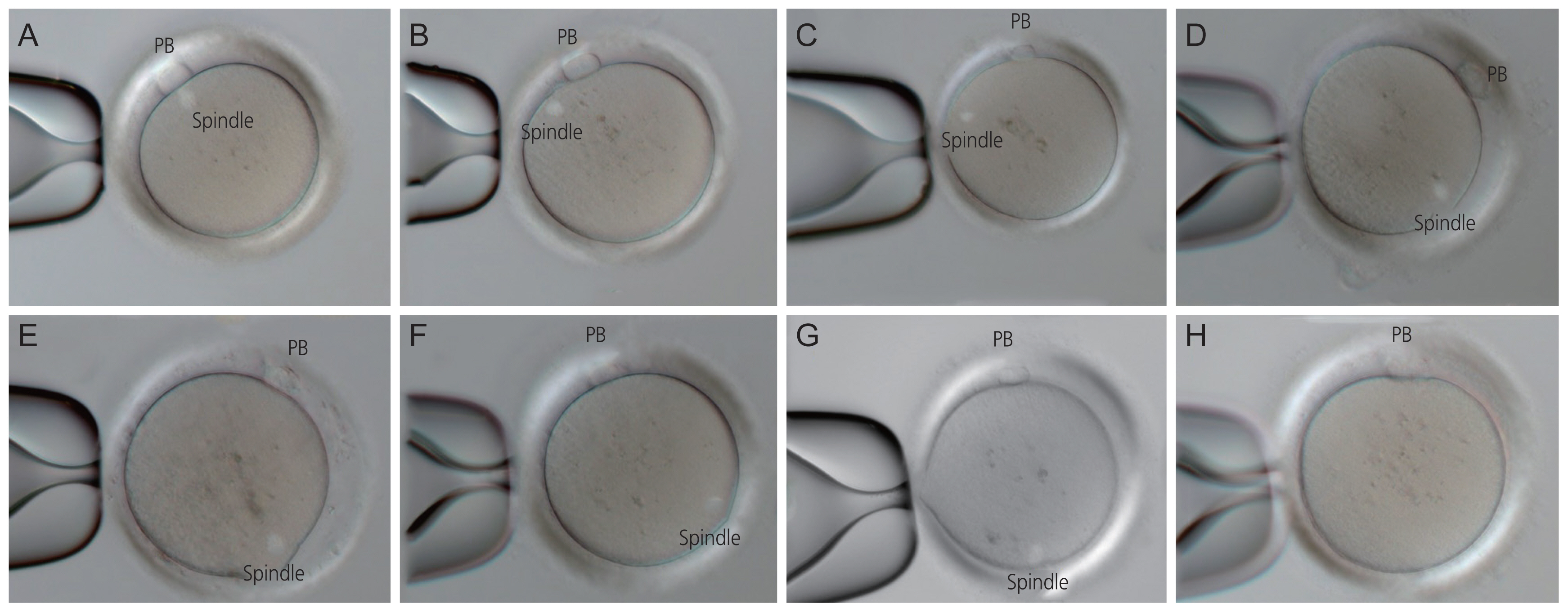
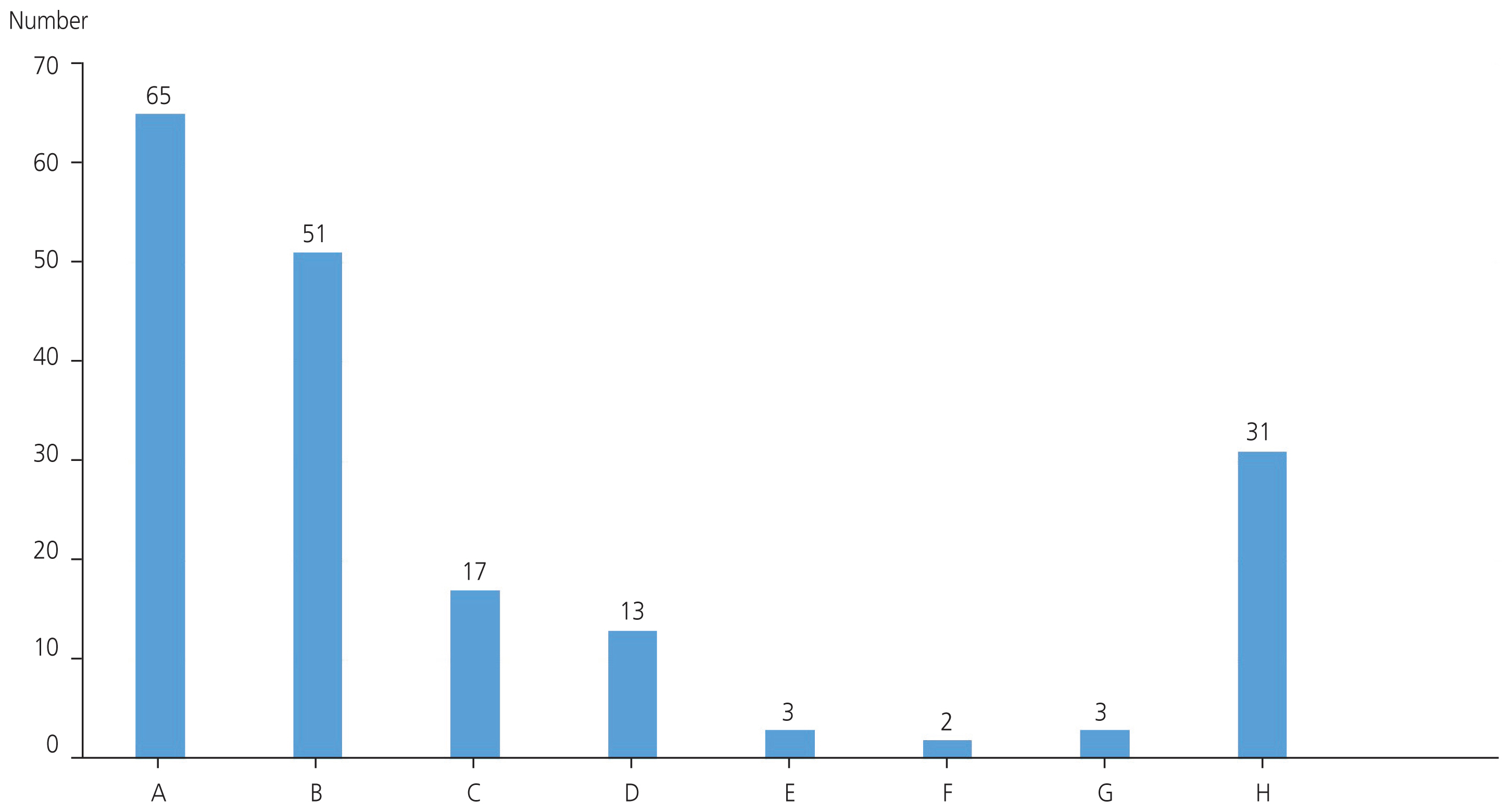
Clinical effectiveness of spindle-view intracytoplasmic sperm injection compared to conventional intracytoplasmic sperm injection in patients with poor ovarian response and previous implantation failure
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Inje University Haeundae Paik Hospital, Busan, Korea
- 2Busan Maria Fertility Clinic, Busan, Korea
- KMID: 2555514
- DOI: http://doi.org/10.5468/ogs.23268
Abstract
Objective
This study aimed to determine the clinical advantage of spindle-view intracytoplasmic sperm injection (SVICSI; a novel technology) over conventional intracytoplasmic sperm injection (cICSI) in patients with poor ovarian response (POR) and previous implantation failure.
Methods
The study included 37 patients who underwent SVICSI followed by fresh embryo transfer (FET) at a single fertility clinic from January to December 2022, 58 patients who underwent cICSI followed by FET at the same fertility clinic from January to December 2021 as a control group. All study participants met the Bologna criteria for POR and had at least three or more previous failed embryo transfers.
Results
The number of blastocyst transfers was significantly higher in the SVICSI group than in the cICSI group. A good-quality cleavage embryo rate, blastocyst rate, and good-quality blastocyst rate were also significantly higher in the SVICSI group than in the cICSI group. There were no significant differences in the rates of fertilization, implantation, clinical pregnancy, or clinical abortion between the two groups.
Conclusion
In patients with POR, those who underwent SVICSI appeared to have better embryos than those who underwent cICSI. However, whether SVICSI improved clinical outcomes such as implantation and pregnancy rates cannot be proven.
Keyword
Figure
Reference
-
References
1. Matsunaga R, Horiuchi T. ICSI with the assistance of meiotic spindle imaging for the production of high quality embryos. J Mamm Ova Res. 2015; 32:3–10.
Article2. Boulet SL, Mehta A, Kissin DM, Warner L, Kawwass JF, Jamieson DJ. Trends in use of and reproductive outcomes associated with intracytoplasmic sperm injection. JAMA. 2015; 313:255–63.
Article3. Lanzendorf S, Maloney M, Ackerman S, Acosta A, Hodgen G. Fertilizing potential of acrosome-defective sperm following microsurgical injection into eggs. Gamete Res. 1988; 19:329–37.
Article4. Van Steirteghem AC, Nagy Z, Joris H, Liu J, Staessen C, Smitz J, et al. High fertilization and implantation rates after intracytoplasmic sperm injection. Hum Reprod. 1993; 8:1061–6.
Article5. Woodward BJ, Montgomery SJ, Hartshorne GM, Campbell KH, Kennedy R. Spindle position assessment prior to ICSI does not benefit fertilization or early embryo quality. Reprod Biomed Online. 2008; 16:232–8.
Article6. Asa E, Tabatabaee R, Farrokhi A, Nejatbakhsh R. Relationship between meiotic spindles visualization and intracytoplasmic sperm injection outcomes in human oocytes. Anat Cell Biol. 2017; 50:26–32.
Article7. Eichenlaub-Ritter U, Shen Y, Tinneberg HR. Manipulation of the oocyte: possible damage to the spindle apparatus. Reprod Biomed Online. 2002; 5:117–24.
Article8. Xia P. Intracytoplasmic sperm injection: correlation of oocyte grade based on polar body, perivitelline space and cytoplasmic inclusions with fertilization rate and embryo quality. Hum Reprod. 1997; 12:1750–5.
Article9. Wang WH, Meng L, Hackett RJ, Odenbourg R, Keefe DL. The spindle observation and its relationship with fertilization after intracytoplasmic sperm injection in living human oocytes. Fertil Steril. 2001; 75:348–53.
Article10. Wang WH, Meng L, Hackett RJ, Keefe DL. Developmental ability of human oocytes with or without birefringent spindles imaged by Polscope before insemination. Hum Reprod. 2001; 16:1464–8.
Article11. Petersen CG, Oliveira JB, Mauri AL, Massaro FC, Baruffi RL, Pontes A, et al. Relationship between visualization of meiotic spindle in human oocytes and ICSI outcomes: a meta-analysis. Reprod Biomed Online. 2009; 18:235–43.
Article12. Cooke S, Tyler JP, Driscoll GL. Meiotic spindle location and identification and its effect on embryonic cleavage plane and early development. Hum Reprod. 2003; 18:2397–405.
Article13. Moon JH, Hyun CS, Lee SW, Son WY, Yoon SH, Lim JH. Visualization of the metaphase II meiotic spindle in living human oocytes using the Polscope enables the prediction of embryonic developmental competence after ICSI. Hum Reprod. 2003; 18:817–20.
Article14. Rienzi L, Ubaldi F, Martinez F, Iacobelli M, Minasi MG, Ferrero S, et al. Relationship between meiotic spindle location with regard to the polar body position and oocyte developmental potential after ICSI. Hum Reprod. 2003; 18:1289–93.
Article15. Cohen Y, Malcov M, Schwartz T, Mey-Raz N, Carmon A, Cohen T, et al. Spindle imaging: a new marker for optimal timing of ICSI? Hum Reprod. 2004; 19:649–54.
Article16. Ferraretti AP, La Marca A, Fauser BC, Tarlatzis B, Nargund G, Gianaroli L, et al. ESHRE consensus on the definition of ‘poor response’ to ovarian stimulation for in vitro fertilization: the Bologna criteria. Hum Reprod. 2011; 26:1616–24.
Article17. Polyzos NP, Blockeel C, Verpoest W, De Vos M, Stoop D, Vloeberghs V, et al. Live birth rates following natural cycle IVF in women with poor ovarian response according to the Bologna criteria. Hum Reprod. 2012; 27:3481–6.
Article18. Polyzos NP, DeVos M, Humaidan P, Stoop D, Ortega-Hrepich C, Devroey P, et al. Corifollitropin alfa followed by rFSH in a GnRH antagonist protocol for poor ovarian responder patients: an observational pilot study. Fertil Steril. 2013; 99:422–6.19. Chun S, Seo JE, Rim YJ, Joo JH, Lee YC, Koo YH. Efficacy of hyaluronan-rich transfer medium on implantation and pregnancy rates in fresh and frozen-thawed blastocyst transfers in Korean women with previous implantation failure. Obstet Gynecol Sci. 2016; 59:201–7.
Article20. Gardner DK, Lane M, Stevens J, Schlenker T, Schoolcraft WB. Blastocyst score affects implantation and pregnancy outcome: towards a single blastocyst transfer. Fertil Steril. 2000; 73:1155–8.
Article21. Liu C, Li Y, Jiang H, Liu Y, Song X. The clinical outcomes of fresh versus frozen embryos transfer in women ≥40 years with poor ovarian response. Obstet Gynecol Sci. 2021; 64:284–92.
Article22. Younis JS, Laufer N. Oocyte donation is an independent risk factor for pregnancy complications: the implications for women of advanced age. J Womens Health (Larchmt). 2015; 24:127–30.
Article23. Ferraretti AP, Gianaroli L. The Bologna criteria for the definition of poor ovarian responders: is there a need for revision? Hum Reprod. 2014; 29:1842–5.
Article24. Khalili MA, Mojibian M, Sultan AM. Role of oocyte morphology on fertilization and embryo formation in assisted reproductive techniques. Middle East Fertil Soc J. 2005; 10:72–7.25. Omidi M, Khalili MA, Nahangi H, Ashourzadeh S, Rahimipour M. Does women’s age influence zona pellucida birefringence of metaphase II oocytes in in-vitro maturation program? Iran J Reprod Med. 2013; 11:823–8.26. Nguyen TT, Doan HT, Quan LH. The spindle of oocytes observed by polarized light microscope can predict embryo quality. Int J Reprod Contracept Obstet Gynecol. 2019; 8:131–5.
Article27. Oldenbourg R. A new view on polarization microscopy. Nature. 1996; 381:811–2.
Article28. Oh HS, Jang J, Yoon HJ. Influence of women’s age on meiotic spindle position and the effect of ICSI based on meiotic spindle visualization. Fertil Steril. 2022; 118:e139.
Article29. Mahfoudh AM, Moon JH, Henderson S, Garcia-Cerrudo E, Son WY, Dahan MH. Relationship between pre-ICSI meiotic spindle angle, ovarian reserve, gonadotropin stimulation, and pregnancy outcomes. J Assist Reprod Genet. 2017; 34:609–15.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison between intracytoplasmic sperm injection and intracytoplasmic morphologically selected sperm injection in oligo-astheno-teratozoospermia patients
- The Efficacy of Intracytoplasmic Sperm Injection for Previous Fertilization Failure with Conventional In Vitro Fertilization
- Clinical Study on Intracytoplasmic Sperm Injection Using Epididymal and Testicular Sperm
- The Outcome of Sperm Retrieval and Intracytoplasmic Sperm Injection in Patients with Obstructive Azoospermia: Impact of Previous Tuberculous Epididymitis
- Twin Pregnancy and Delivery After Intracytoplasmic Sperm Injection Followed by Calcium Ionophore with Spermatozoa from a Globozoospermic Man: A Case Report