Obstet Gynecol Sci.
2024 May;67(3):296-303. 10.5468/ogs.23291.
Determination of ovarian transposition through prediction of postoperative adjuvant therapy in young patients with early stage cervical cancer undergoing surgery: a Korean multicenter retrospective study (KGOG 1042)
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Kyung Hee University Medical Center, College of Medicine Kyung Hee University, Seoul, Korea
- 2Department of Obstetrics and Gynecology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Department of Obstetrics and Gynecology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 4Department of Obstetrics and Gynecology, Korea Cancer Center Hospital, Korea Institute of Radiological and Medical Sciences, Seoul, Korea
- 5National Cancer Center, Goyang, Korea
- 6Department of Obstetrics and Gynecology, Inha University Hospital, Inha University School of Medicine, Incheon, Korea
- 7Department of Obstetrics and Gynecology, Sanggye Paik Hospital, School of Medicine, Inje University, Seoul, Korea
- 8Department of Obstetrics and Gynecology, Ewha Womans University College of Medicine, Seoul, Korea
- 9Department of Obstetrics and Gynecology, CHA Gangnam Medical Center, CHA University College of Medicine, Seoul, Korea
- 10Department of Obstetrics and Gynecology, Kyung Hee University Hospital at Gangdong, Seoul, Korea
- KMID: 2555513
- DOI: http://doi.org/10.5468/ogs.23291
Abstract
Objective
We aimed to predict the risk of postoperative adjuvant therapy using preoperative variables in young patients with early stage cervical cancer. The predicted risk can guide whether ovarian transposition should be performed during surgery.
Methods
In total, 886 patients with stage IB1-IIA cervical cancer aged 20-45 years who underwent modified radical or radical hysterectomy between January 2000 and December 2008 were included. Preoperative variables, preoperative laboratory findings, International Federation of Gynaecology and Obstetrics stage, tumor size, and pathological variables were collected. Patients with high risk factors or those who met the Sedlis criteria were considered adjuvant therapy risk (+); others were considered adjuvant therapy risk (-). A decision-tree model using preoperative variables was constructed to predict the risk of adjuvant therapy.
Results
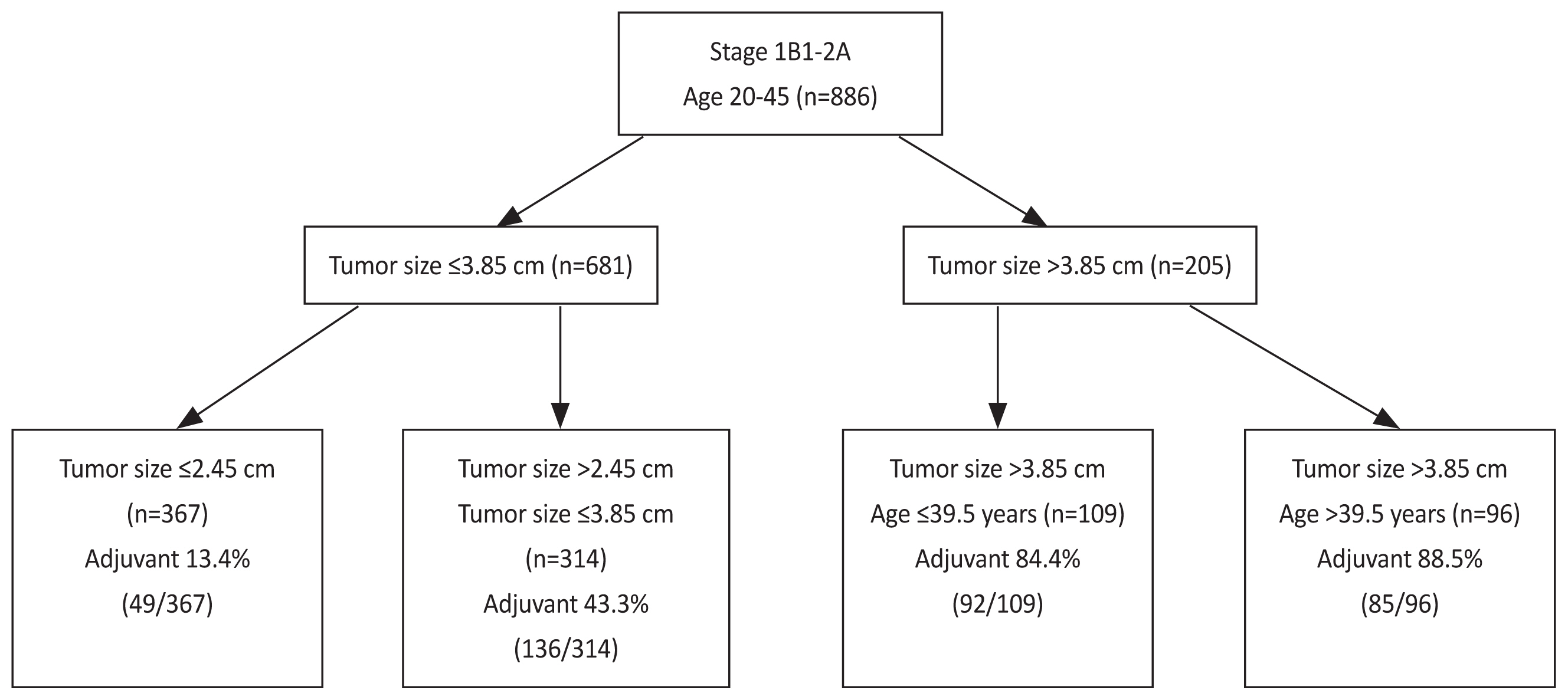
Of 886 patients, 362 were adjuvant therapy risk (+) (40.9%). The decision-tree model with four distinct adjuvant therapy risks using tumor size and age were generated. Specifically, patients with tumor size ≤2.45 cm had low risk (49/367; 13.4%), those with tumor size ≤3.85 cm and >2.45 cm had moderate risk (136/314; 43.3%), those with tumor size >3.85 cm and age ≤39.5 years had high risk (92/109; 84.4%), and those with tumor size >3.85 cm and age >39.5 years had the highest risk (85/96; 88.5%).
Conclusion
The risk of postoperative adjuvant therapy in young patients with early stage cervical cancer can be predicted using preoperative variables. We can decide whether ovarian transposition should be performed using the predicted risk.
Figure
Reference
-
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68:394–424.2. Arbyn M, Weiderpass E, Bruni L, de Sanjosé S, Saraiya M, Ferlay J, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health. 2020; 8:e191–203.3. Meggiolaro A, Unim B, Semyonov L, Miccoli S, Maffongelli E, La Torre G. The role of pap test screening against cervical cancer: a systematic review and meta-analysis. Clin Ter. 2016; 167:124–39.4. Yin L, Lu S, Zhu J, Zhang W, Ke G. Ovarian transposition before radiotherapy in cervical cancer patients: functional outcome and the adequate dose constraint. Radiat Oncol. 2019; 14:100.5. Moon EK, Oh CM, Won YJ, Lee JK, Jung KW, Cho H, et al. Trends and age-period-cohort effects on the incidence and mortality rate of cervical cancer in Korea. Cancer Res Treat. 2017; 49:526–33.6. Jewell EL, Kulasingam S, Myers ER, Alvarez Secord A, Havrilesky LJ. Primary surgery versus chemoradiation in the treatment of IB2 cervical carcinoma: a cost effectiveness analysis. Gynecol Oncol. 2007; 107:532–40.7. Sedlis A, Bundy BN, Rotman MZ, Lentz SS, Muderspach LI, Zaino RJ. A randomized trial of pelvic radiation therapy versus no further therapy in selected patients with stage IB carcinoma of the cervix after radical hysterectomy and pelvic lymphadenectomy: a Gynecologic Oncology group study. Gynecol Oncol. 1999; 73:177–83.8. Rotman M, Sedlis A, Piedmonte MR, Bundy B, Lentz SS, Muderspach LI, et al. A phase III randomized trial of postoperative pelvic irradiation in stage IB cervical carcinoma with poor prognostic features: follow-up of a gynecologic oncology group study. Int J Radiat Oncol Biol Phys. 2006; 65:169–76.9. Wo JY, Viswanathan AN. Impact of radiotherapy on fertility, pregnancy, and neonatal outcomes in female cancer patients. Int J Radiat Oncol Biol Phys. 2009; 73:1304–12.10. National Comprehensive Cancer Network. Cervical cancer (Version 1, 2021) [Internet]. In : Plymouth Meeting: National Comprehensive Cancer Network; c2020. [cited 2011 Nov 3]. Available from: chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/ https://sukhin-oncology.com.ua/wp-content/uploads/2020/11/cervical2020.pdf .11. Moawad NS, Santamaria E, Rhoton-Vlasak A, Lightsey JL. Laparoscopic ovarian transposition before pelvic cancer treatment: ovarian function and fertility preservation. J Minim Invasive Gynecol. 2017; 24:28–35.12. Paik ES, Lim MC, Kim MH, Kim YH, Song ES, Seong SJ, et al. Prognostic model for survival and recurrence in patients with early-stage cervical cancer: a Korean Gynecologic Oncology group study (KGOG 1028). Cancer Res Treat. 2020; 52:320–33.13. Buonomo B, Multinu F, Casarin J, Betella I, Zanagnolo V, Aletti G, et al. Ovarian transposition in patients with cervical cancer prior to pelvic radiotherapy: a systematic review. Int J Gynecol Cancer. 2021; 31:360–70.14. Thiangphak E, Leetanaporn K, Buhachat R. Pretreatment total lymphocyte count as a prognostic factor of survival in patients with recurrent cervical cancer after definitive radiation-based therapy: a retrospective study. Obstet Gynecol Sci. 2023; 66:407–16.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of ovarian metastasis on transposed ovary in patient treated for uterine cervical cancer
- Maintenance of ovarian function in end-of-life cervical cancer patient following primary surgico-radiotherapy and ovarian transposition
- Adjuvant therapy in cervical cancer patients with high risk factors
- Ovarian Metastasis from Stage IB Cervical Adenocarcinoma: A Case Report
- A case of ovarian metastasis of the recurrent uterine cervical cancer after adjuvant radiation therapy