J Korean Med Sci.
2024 May;39(18):e162. 10.3346/jkms.2024.39.e162.
Current Status of Molecular Diagnosis of Hereditary Hemolytic Anemia in Korea
- Affiliations
-
- 1Department of Pediatrics, Inje University Haeundae Paik Hospital, Busan, Korea
- 2Department of Pediatrics, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea
- 3Department of Pediatrics, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Department of Laboratory Medicine, Dong-A University College of Medicine, Busan, Korea
- 5Department of Laboratory Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 6Department of Laboratory Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 7Department of Pediatrics, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2555503
- DOI: http://doi.org/10.3346/jkms.2024.39.e162
Abstract
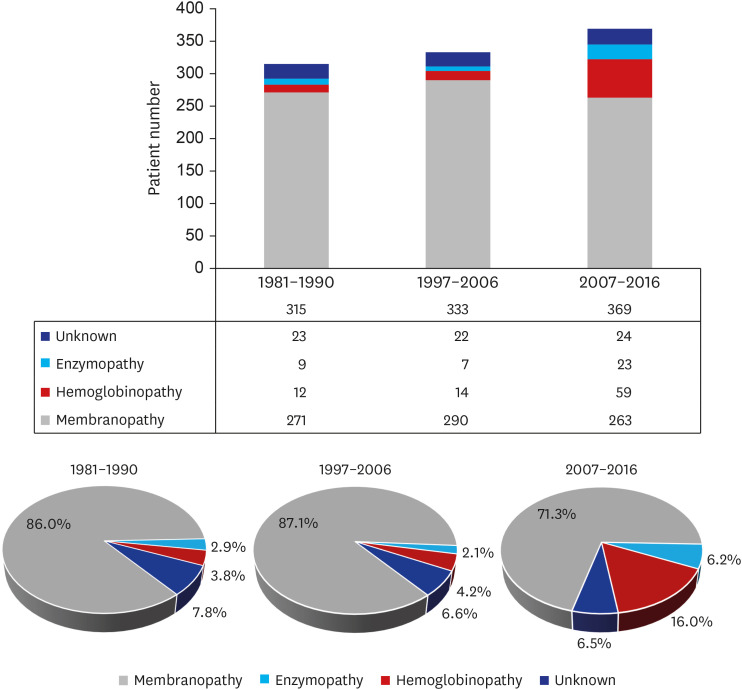
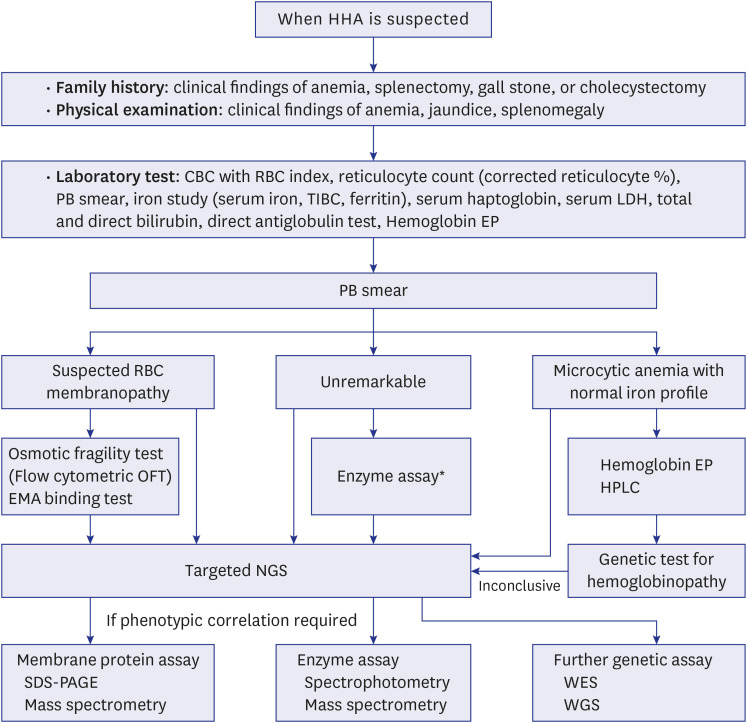
- Hereditary hemolytic anemia (HHA) is considered a group of rare hematological diseases in Korea, primarily because of its unique ethnic characteristics and diagnostic challenges. Recently, the prevalence of HHA has increased in Korea, reflecting the increasing number of international marriages and increased awareness of the disease. In particular, the diagnosis of red blood cell (RBC) enzymopathy experienced a resurgence, given the advances in diagnostic techniques. In 2007, the RBC Disorder Working Party of the Korean Society of Hematology developed the Korean Standard Operating Procedure for the Diagnosis of Hereditary Hemolytic Anemia, which has been continuously updated since then. The latest Korean clinical practice guidelines for diagnosing HHA recommends performing nextgeneration sequencing as a preliminary step before analyzing RBC membrane proteins and enzymes. Recent breakthroughs in molecular genetic testing methods, particularly nextgeneration sequencing, are proving critical in identifying and providing insight into cases of HHA with previously unknown diagnoses. These innovative molecular genetic testing methods have now become important tools for the management and care planning of patients with HHA. This review aims to provide a comprehensive overview of recent advances in molecular genetic testing for the diagnosis of HHA, with particular emphasis on the Korean context.
Keyword
Figure
Reference
-
1. Haley K. Congenital hemolytic anemia. Med Clin North Am. 2017; 101(2):361–374. PMID: 28189176.2. Chueh HW, Hwang SM, Shim YJ, Lee JM, Park HS, Lee JH, et al. Korean clinical practice guidelines for the diagnosis of hereditary hemolytic anemia. Blood Res. 2022; 57(2):86–94.3. Fermo E, Vercellati C, Marcello AP, Keskin EY, Perrotta S, Zaninoni A, et al. Targeted next generation sequencing and diagnosis of congenital hemolytic anemias: a three years experience monocentric study. Front Physiol. 2021; 12:684569. PMID: 34093240.4. Cho HS, Hah JO, Kang IJ, Kang HJ, Kwak JY, Koo HH, et al. Hereditary hemolytic anemia in Korea: a retrospective study from 1997 to 2006. Korean J Hematol. 2007; 42(3):197–205.5. Park ES, Jung HL, Kim HJ, Park SS, Bae SH, Shin HY, et al. Hereditary hemolytic anemia in Korea from 2007 to 2011: a study by the Korean Hereditary Hemolytic Anemia Working Party of the Korean Society of Hematology. Blood Res. 2013; 48(3):211–216. PMID: 24086942.6. Shim YJ, Jung HL, Shin HY, Kang HJ, Choi JY, Hah JO, et al. Epidemiological study of hereditary hemolytic anemia in the Korean pediatric population during 1997–2016: a nationwide retrospective cohort study. J Korean Med Sci. 2020; 35(33):e279. PMID: 32830468.7. Jung HL. A new paradigm in the diagnosis of hereditary hemolytic anemia. Blood Res. 2013; 48(4):237–239. PMID: 24466544.8. Park SH, Park CJ, Lee BR, Cho YU, Jang S, Kim N, et al. Comparison study of the eosin-5′-maleimide binding test, flow cytometric osmotic fragility test, and cryohemolysis test in the diagnosis of hereditary spherocytosis. Am J Clin Pathol. 2014; 142(4):474–484. PMID: 25239414.9. Won DI, Suh JS. Flow cytometric detection of erythrocyte osmotic fragility. Cytometry B Clin Cytom. 2009; 76(2):135–141. PMID: 18727072.10. Rees DC, Williams TN, Gladwin MT. Sickle-cell disease. Lancet. 2010; 376(9757):2018–2031. PMID: 21131035.11. Weatherall DJ. The inherited diseases of hemoglobin are an emerging global health burden. Blood. 2010; 115(22):4331–4336. PMID: 20233970.12. Bolton-Maggs PH, Langer JC, Iolascon A, Tittensor P, King MJ. General Haematology Task Force of the British Committee for Standards in Haematology. Guidelines for the diagnosis and management of hereditary spherocytosis--2011 update. Br J Haematol. 2012; 156(1):37–49. PMID: 22055020.13. Ghosh K, Colah R, Manglani M, Choudhry VP, Verma I, Madan N, et al. Guidelines for screening, diagnosis and management of hemoglobinopathies. Indian J Hum Genet. 2014; 20(2):101–119. PMID: 25400338.14. Perrotta S, Gallagher PG, Mohandas N. Hereditary spherocytosis. Lancet. 2008; 372(9647):1411–1426. PMID: 18940465.15. Da Costa L, Galimand J, Fenneteau O, Mohandas N. Hereditary spherocytosis, elliptocytosis, and other red cell membrane disorders. Blood Rev. 2013; 27(4):167–178. PMID: 23664421.16. Mansour-Hendili L, Aissat A, Badaoui B, Sakka M, Gameiro C, Ortonne V, et al. Exome sequencing for diagnosis of congenital hemolytic anemia. Orphanet J Rare Dis. 2020; 15(1):180. PMID: 32641076.17. King MJ, Garçon L, Hoyer JD, Iolascon A, Picard V, Stewart G, et al. ICSH guidelines for the laboratory diagnosis of nonimmune hereditary red cell membrane disorders. Int J Lab Hematol. 2015; 37(3):304–325. PMID: 25790109.18. Cohen AR, Galanello R, Pennell DJ, Cunningham MJ, Vichinsky E. Thalassemia. Hematology Am Soc Hematol Educ Program. 2004; 2004(1):14–34.19. Harteveld CL, Higgs DR. Alpha-thalassaemia. Orphanet J Rare Dis. 2010; 5(1):13. PMID: 20507641.20. Marengo-Rowe AJ. The thalassemias and related disorders. Proc Bayl Univ Med Cent. 2007; 20(1):27–31. PMID: 17256039.21. Kohne E. Hemoglobinopathies: clinical manifestations, diagnosis, and treatment. Dtsch Arztebl Int. 2011; 108(31-32):532–540. PMID: 21886666.22. Galanello R, Origa R. Beta-thalassemia. Orphanet J Rare Dis. 2010; 5(1):11. PMID: 20492708.23. Dhar A, Leung TM, Appiah-Kubi A, Gruber D, Aygun B, Serigano O, et al. Longitudinal analysis of cardiac abnormalities in pediatric patients with sickle cell anemia and effect of hydroxyurea therapy. Blood Adv. 2021; 5(21):4406–4412. PMID: 34529023.24. World Health Organization. Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity. Geneva, Switzerland: World Health Organization;2011.25. Nkhoma ET, Poole C, Vannappagari V, Hall SA, Beutler E. The global prevalence of glucose-6-phosphate dehydrogenase deficiency: a systematic review and meta-analysis. Blood Cells Mol Dis. 2009; 42(3):267–278. PMID: 19233695.26. Cappellini MD, Fiorelli G. Glucose-6-phosphate dehydrogenase deficiency. Lancet. 2008; 371(9606):64–74. PMID: 18177777.27. Beutler E, Gelbart T. Estimating the prevalence of pyruvate kinase deficiency from the gene frequency in the general white population. Blood. 2000; 95(11):3585–3588. PMID: 10828047.28. Carey PJ, Chandler J, Hendrick A, Reid MM, Saunders PW, Tinegate H, et al. Prevalence of pyruvate kinase deficiency in northern European population in the north of England. Blood. 2000; 96(12):4005–4006. PMID: 11186276.29. Mbayabo G, Lumbala Kabuyi P, Ngole M, Lumaka A, Race V, Maisin D, et al. Value of DNA testing in the diagnosis of sickle-cell anemia in childhood in an environment with a high prevalence of other causes of anemia. J Clin Lab Anal. 2022; 36(8):e24593. PMID: 35819088.30. van Straaten S, Biemond BJ, Kerkhoffs JL, Gitz-Francois J, van Wijk R, van Beers EJ. Iron overload in patients with rare hereditary hemolytic anemia: Evidence-based suggestion on whom and how to screen. Am J Hematol. 2018; 93(11):E374–E376. PMID: 30105801.31. Teawtrakul N, Jetsrisuparb A, Pongudom S, Sirijerachai C, Chansung K, Wanitpongpun C, et al. Epidemiologic study of major complications in adolescent and adult patients with thalassemia in Northeastern Thailand: the E-SAAN study phase I. Hematology. 2018; 23(1):55–60. PMID: 28759343.32. Kham SK, Quah TC, Loong AM, Tan PL, Fraser A, Chong SS, et al. A molecular epidemiologic study of thalassemia using newborns’ cord blood in a multiracial Asian population in Singapore: results and recommendations for a population screening program. J Pediatr Hematol Oncol. 2004; 26(12):817–819. PMID: 15591902.33. Phadke SR, Puri RD, Ranganath P. Prenatal screening for genetic disorders: Suggested guidelines for the Indian Scenario. Indian J Med Res. 2017; 146(6):689–699. PMID: 29664026.34. Huang H, Chen M, Chen L, Zhang M, Wang Y, Lin N, et al. Prenatal diagnosis of thalassemia in 695 pedigrees from southeastern China: a 10-year follow-up study. J Clin Lab Anal. 2021; 35(10):e23982. PMID: 34480509.35. Silva R, Amarasinghe D, Perera S, Premawardhena A. A systematic review on diagnostic methods of red cell membrane disorders in Asia. Int J Lab Hematol. 2022; 44(2):248–262. PMID: 35068068.36. Ahn DH, Sohn KC, Kang IJ, Kang JM, Ko YS, Ko YW, et al. Statistical analysis of hemolytic anemia in Korea. Korean J Hematol. 1991; 26(2):445–461.37. Lee HJ, Shin KH, Kim HH, Yang EJ, Park KH, Kim MJ, et al. Increased prevalence of thalassemia in young people in Korea: impact of increasing immigration. Ann Lab Med. 2019; 39(2):133–140. PMID: 30430775.38. Lee J, Park J, Choi H, Kim J, Kwon A, Jang W, et al. Genetic profiles of Korean patients with glucose-6-phosphate dehydrogenase deficiency. Ann Lab Med. 2017; 37(2):108–116. PMID: 28028996.39. Kim M, Park J, Lee J, Jang W, Chae H, Choi H, et al. Hemolytic anemia with null PKLR mutations identified using whole exome sequencing and cured by hematopoietic stem cell transplantation combined with splenectomy. Bone Marrow Transplant. 2016; 51(12):1605–1608. PMID: 27595284.40. Angastiniotis M, Vives Corrons JL, Soteriades ES, Eleftheriou A. The impact of migrations on the health services for rare diseases in Europe: the example of haemoglobin disorders. Sci World J. 2013; 2013:727905.41. Aguilar Martinez P, Angastiniotis M, Eleftheriou A, Gulbis B, Mañú Pereira MM, Petrova-Benedict R, et al. Haemoglobinopathies in Europe: health & migration policy perspectives. Orphanet J Rare Dis. 2014; 9(1):97. PMID: 24980780.42. Venturelli D, Lodi M, Palazzi G, Bergonzini G, Doretto G, Zini A, et al. Sickle cell disease in areas of immigration of high-risk populations: a low cost and reproducible method of screening in northern Italy. Blood Transfus. 2014; 12(3):346–351. PMID: 24887233.43. Kim YP, Joh JY, Shin IS. Family function of the families consisting of Asian immigrant women living in South Korea: a 3-year longitudinal study. Asia Pac J Public Health. 2015; 27(2):NP2702–NP2711. PMID: 22652245.44. Kim Y, Park J, Kim M. Diagnostic approaches for inherited hemolytic anemia in the genetic era. Blood Res. 2017; 52(2):84–94. PMID: 28698843.45. Bianchi P, Vercellati C, Fermo E. How will next generation sequencing (NGS) improve the diagnosis of congenital hemolytic anemia? Ann Transl Med. 2020; 8(6):268. PMID: 32355712.46. Noronha SA. Acquired and congenital hemolytic anemia. Pediatr Rev. 2016; 37(6):235–246. PMID: 27252179.47. Mohandas N. Inherited hemolytic anemia: a possessive beginner’s guide. Hematology Am Soc Hematol Educ Program. 2018; 2018(1):377–381. PMID: 30504335.48. Grace RF, Bianchi P, van Beers EJ, Eber SW, Glader B, Yaish HM, et al. Clinical spectrum of pyruvate kinase deficiency: data from the Pyruvate Kinase Deficiency Natural History Study. Blood. 2018; 131(20):2183–2192. PMID: 29549173.49. Zanella A, Bianchi P. Red cell pyruvate kinase deficiency: from genetics to clinical manifestations. Best Pract Res Clin Haematol. 2000; 13(1):57–81.50. Grace RF, Mark Layton D, Barcellini W. How we manage patients with pyruvate kinase deficiency. Br J Haematol. 2019; 184(5):721–734. PMID: 30681718.51. Lee YK, Cho HI, Park SS, Lee YJ, Ra E, Chang YH, et al. Abnormalities of erythrocyte membrane proteins in Korean patients with hereditary spherocytosis. J Korean Med Sci. 2000; 15(3):284–288. PMID: 10895969.52. Park J, Jeong DC, Yoo J, Jang W, Chae H, Kim J, et al. Mutational characteristics of ANK1 and SPTB genes in hereditary spherocytosis. Clin Genet. 2016; 90(1):69–78. PMID: 26830532.53. Choi HS, Choi Q, Kim JA, Im KO, Park SN, Park Y, et al. Molecular diagnosis of hereditary spherocytosis by multi-gene target sequencing in Korea: matching with osmotic fragility test and presence of spherocyte. Orphanet J Rare Dis. 2019; 14(1):114. PMID: 31122244.54. Russo R, Andolfo I, Manna F, Gambale A, Marra R, Rosato BE, et al. Multi-gene panel testing improves diagnosis and management of patients with hereditary anemias. Am J Hematol. 2018; 93(5):672–682. PMID: 29396846.55. Roy NBA, Da Costa L, Russo R, Bianchi P, Mañú-Pereira MDM, Fermo E, et al. The use of next-generation sequencing in the diagnosis of rare inherited anaemias: a Joint BSH/EHA Good Practice Paper. Br J Haematol. 2022; 198(3):459–477. PMID: 35661144.56. Cho H, Lee JW, Chung NG, Lee SE, Jang W, Kim M, et al. Two Korean cases of hereditary spherocytosis caused by mutations in SLC4A1 . Lab Med Online. 2018; 8(3):114–118.57. Shin S, Jang W, Kim M, Kim Y, Park SY, Park J, et al. Targeted next-generation sequencing identifies a novel nonsense mutation in SPTB for hereditary spherocytosis: a case report of a Korean family. Medicine (Baltimore). 2018; 97(3):e9677. PMID: 29505016.58. Shin S, Hwang KA, Paik K, Park J. A novel EPB41 p.Trp704* mutation in a Korean patient with hereditary elliptocytosis: a case report. Hematology. 2020; 25(1):321–326. PMID: 32807033.59. Jang W, Kim SK, Nahm CH, Choi JW, Kim JJ, Moon Y. A novel de novo mutation in ANK1 gene identified through targeted next-generation sequencing in a neonate with hereditary spherocytosis. Ann Clin Lab Sci. 2021; 51(1):136–139. PMID: 33653793.60. Yoon SJ, Cho EH, Woo HY, Park H, Jung HL, Kwon MJ. Identification of a de novo ANK1 variant in a patient with hereditary spherocytosis on multi-gene panel testing. Lab Med Online. 2022; 12(1):58–62.61. Arora RD, Dass J, Maydeo S, Arya V, Radhakrishnan N, Sachdeva A, et al. Flow cytometric osmotic fragility test and eosin-5′-maleimide dye-binding tests are better than conventional osmotic fragility tests for the diagnosis of hereditary spherocytosis. Int J Lab Hematol. 2018; 40(3):335–342. PMID: 29573337.62. Ciepiela O, Adamowicz-Salach A, Zgodzińska A, Łazowska M, Kotuła I. Flow cytometric osmotic fragility test: Increased assay sensitivity for clinical application in pediatric hematology. Cytometry B Clin Cytom. 2018; 94(1):189–195. PMID: 28103644.63. King MJ, Smythe JS, Mushens R. Eosin-5-maleimide binding to band 3 and Rh-related proteins forms the basis of a screening test for hereditary spherocytosis. Br J Haematol. 2004; 124(1):106–113. PMID: 14675415.64. Risinger M, Kalfa TA. Red cell membrane disorders: structure meets function. Blood. 2020; 136(11):1250–1261. PMID: 32702754.65. Da Costa L, Suner L, Galimand J, Bonnel A, Pascreau T, Couque N, et al. Diagnostic tool for red blood cell membrane disorders: assessment of a new generation ektacytometer. Blood Cells Mol Dis. 2016; 56(1):9–22. PMID: 26603718.66. Zaninoni A, Fermo E, Vercellati C, Consonni D, Marcello AP, Zanella A, et al. Use of laser assisted optical rotational cell analyzer (LoRRca MaxSis) in the diagnosis of RBC membrane disorders, enzyme defects, and congenital dyserythropoietic anemias: a monocentric study on 202 patients. Front Physiol. 2018; 9:451. PMID: 29755372.67. Kim YK, Lim YT, Suh JS, Hah JO, Lee JM. Erythrocyte deformability reduction in various pediatric hematologic diseases. Clin Hemorheol Microcirc. 2020; 75(3):361–367. PMID: 32224530.68. Bryk AH, Wiśniewski JR. Quantitative analysis of human red blood cell proteome. J Proteome Res. 2017; 16(8):2752–2761. PMID: 28689405.69. Park CM, Lee K, Jun SH, Song SH, Song J. Ultra-performance liquid chromatography-tandem mass spectrometry-based multiplex enzyme assay for six enzymes associated with hereditary hemolytic anemia. J Chromatogr B Analyt Technol Biomed Life Sci. 2017; 1060:76–83.70. Risinger M, Emberesh M, Kalfa TA. Rare hereditary hemolytic anemias: diagnostic approach and considerations in management. Hematol Oncol Clin North Am. 2019; 33(3):373–392. PMID: 31030808.71. Roy NB, Wilson EA, Henderson S, Wray K, Babbs C, Okoli S, et al. A novel 33-gene targeted resequencing panel provides accurate, clinical-grade diagnosis and improves patient management for rare inherited anaemias. Br J Haematol. 2016; 175(2):318–330. PMID: 27432187.72. Aggarwal A, Jamwal M, Sharma P, Sachdeva MU, Bansal D, Malhotra P, et al. Deciphering molecular heterogeneity of Indian families with hereditary spherocytosis using targeted next-generation sequencing: first South Asian study. Br J Haematol. 2020; 188(5):784–795. PMID: 31602632.73. Nieto JM, Rochas-López S, González-Fernández FA, Villegas-Martínez A, Bolaños-Calderón E, Salido-Fiérrez E, et al. Next generation sequencing for diagnosis of hereditary anemia: experience in a Spanish reference center. Clin Chim Acta. 2022; 531:112–119. PMID: 35351432.74. Andolfo I, Russo R, Gambale A, Iolascon A. Hereditary stomatocytosis: an underdiagnosed condition. Am J Hematol. 2018; 93(1):107–121. PMID: 28971506.75. Park J, Jang W, Han E, Chae H, Yoo J, Kim Y, et al. Hereditary dehydrated stomatocytosis with splicing site mutation of PIEZO1 mimicking myelodysplastic syndrome diagnosed by targeted next-generation sequencing. Pediatr Blood Cancer. 2018; 65(7):e27053. PMID: 29603612.76. Bean LJH, Funke B, Carlston CM, Gannon JL, Kantarci S, Krock BL, et al. Diagnostic gene sequencing panels: from design to report-a technical standard of the American College of Medical Genetics and Genomics (ACMG). Genet Med. 2020; 22(3):453–461. PMID: 31732716.77. Zhao J, Li J, Lai Q, Yu Y. Combined use of gap-PCR and next-generation sequencing improves thalassaemia carrier screening among premarital adults in China. J Clin Pathol. 2020; 73(8):488–492. PMID: 31980563.78. Lee JS, Cho SI, Park SS, Seong MW. Molecular basis and diagnosis of thalassemia. Blood Res. 2021; 56(S1):S39–S43. PMID: 33935034.79. Tse WT, Gallagher PG, Jenkins PB, Wang Y, Benoit L, Speicher D, et al. Amino-acid substitution in α-spectrin commonly coinherited with nondominant hereditary spherocytosis. Am J Hematol. 1997; 54(3):233–241. PMID: 9067503.80. Iolascon A, Andolfo I, Russo R. Advances in understanding the pathogenesis of red cell membrane disorders. Br J Haematol. 2019; 187(1):13–24. PMID: 31364155.81. Sabath DE. Molecular diagnosis of thalassemias and hemoglobinopathies: an ACLPS critical review. Am J Clin Pathol. 2017; 148(1):6–15. PMID: 28605432.82. Lin PC, Chiou SS, Lin CY, Wang SC, Huang HY, Chang YS, et al. Whole-exome sequencing for the genetic diagnosis of congenital red blood cell membrane disorders in Taiwan. Clin Chim Acta. 2018; 487:311–317. PMID: 30317022.83. Rieneck K, Lausen B, Clausen FB, Jønson L, Hansen AT, Dziegiel MH. Exome-based trio analysis for diagnosis of the cause of congenital severe hemolytic anemia in a child. Transfus Med Hemother. 2022; 49(5):320–325. PMID: 37969868.84. Wang R, Yang S, Xu M, Huang J, Liu H, Gu W, et al. Exome sequencing confirms molecular diagnoses in 38 Chinese families with hereditary spherocytosis. Sci China Life Sci. 2018; 61(8):947–953. PMID: 29572776.85. Hamada M, Doisaki S, Okuno Y, Muramatsu H, Hama A, Kawashima N, et al. Whole-exome analysis to detect congenital hemolytic anemia mimicking congenital dyserythropoietic anemia. Int J Hematol. 2018; 108(3):306–311. PMID: 29936674.86. Agarwal AM, Nussenzveig RH, Reading NS, Patel JL, Sangle N, Salama ME, et al. Clinical utility of next-generation sequencing in the diagnosis of hereditary haemolytic anaemias. Br J Haematol. 2016; 174(5):806–814. PMID: 27292444.87. Cortesi V, Manzoni F, Raffaeli G, Cavallaro G, Fattizzo B, Amelio GS, et al. Severe presentation of congenital hemolytic anemias in the neonatal age: diagnostic and therapeutic issues. Diagnostics (Basel). 2021; 11(9):1549. PMID: 34573891.88. Wu Y, Liao L, Lin F. The diagnostic protocol for hereditary spherocytosis-2021 update. J Clin Lab Anal. 2021; 35(12):e24034. PMID: 34689357.89. Bianchi P, Fermo E, Glader B, Kanno H, Agarwal A, Barcellini W, et al. Addressing the diagnostic gaps in pyruvate kinase deficiency: consensus recommendations on the diagnosis of pyruvate kinase deficiency. Am J Hematol. 2019; 94(1):149–161. PMID: 30358897.90. Davis BH. CLSI Document H52-A2. Red Blood Cell Diagnostic Testing Using Flow Cytometry. 2nd ed. Berwyn, PA, USA: Clinical and Laboratory Standards Institute;2014.91. King MJ, Zanella A. Hereditary red cell membrane disorders and laboratory diagnostic testing. Int J Lab Hematol. 2013; 35(3):237–243. PMID: 23480868.92. Gambale A, Iolascon A, Andolfo I, Russo R. Diagnosis and management of congenital dyserythropoietic anemias. Expert Rev Hematol. 2016; 9(3):283–296. PMID: 26653117.93. Bender MA, Yusuf C, Davis T, Dorley MC, Del Pilar Aguinaga M, Ingram A, et al. Newborn screening practices and alpha-thalassemia detection—United States, 2016. MMWR Morb Mortal Wkly Rep. 2020; 69(36):1269–1272. PMID: 32915167.94. Jamwal M, Aggarwal A, Palodhi A, Sharma P, Bansal D, Trehan A, et al. Next-generation sequencing-based diagnosis of unexplained inherited hemolytic anemias reveals wide genetic and phenotypic heterogeneity. J Mol Diagn. 2020; 22(4):579–590. PMID: 32036089.95. Zarza R, Moscardó M, Alvarez R, García J, Morey M, Pujades A, et al. Co-existence of hereditary spherocytosis and a new red cell pyruvate kinase variant: PK mallorca. Haematologica. 2000; 85(3):227–232. PMID: 10702808.96. Favale F, Gardembas M, Pajot O, Saada V, Fénéant-Thibault M, Delaunay J, et al. Southeast Asian ovalocytosis and a sickle cell trait in a young patient with sudden retinal stroke: a fortuitous association? Hemoglobin. 2009; 33(6):475–479. PMID: 19958192.97. Fermo E, Vercellati C, Marcello AP, Zaninoni A, van Wijk R, Mirra N, et al. Hereditary Xerocytosis due to mutations in PIEZO1 gene associated with heterozygous pyruvate kinase deficiency and beta-thalassemia trait in two unrelated families. Case Rep Hematol. 2017; 2017:2769570. PMID: 28367341.98. Khurana M, Edwards D, Rescorla F, Miller C, He Y, Sierra Potchanant E, et al. Whole-exome sequencing enables correct diagnosis and surgical management of rare inherited childhood anemia. Cold Spring Harb Mol Case Stud. 2018; 4(5):a003152. PMID: 30275003.99. Cappellini MD, Porter JB, Viprakasit V, Taher AT. A paradigm shift on beta-thalassaemia treatment: how will we manage this old disease with new therapies? Blood Rev. 2018; 32(4):300–311. PMID: 29455932.100. Belfield KD, Tichy EM. Review and drug therapy implications of glucose-6-phosphate dehydrogenase deficiency. Am J Health Syst Pharm. 2018; 75(3):97–104. PMID: 29305344.101. Al-Samkari H, Van Beers EJ, Kuo KH, Barcellini W, Bianchi P, Glenthøj A, et al. The variable manifestations of disease in pyruvate kinase deficiency and their management. Haematologica. 2020; 105(9):2229–2239. PMID: 33054048.102. Kung C, Hixon J, Kosinski PA, Cianchetta G, Histen G, Chen Y, et al. AG-348 enhances pyruvate kinase activity in red blood cells from patients with pyruvate kinase deficiency. Blood. 2017; 130(11):1347–1356. PMID: 28760888.103. Johnson S, Grace RF, Despotovic JM. Diagnosis, monitoring, and management of pyruvate kinase deficiency in children. Pediatr Blood Cancer. 2022; 69(8):e29696. PMID: 35452178.104. Gallagher PG, Maksimova Y, Lezon-Geyda K, Newburger PE, Medeiros D, Hanson RD, et al. Aberrant splicing contributes to severe α-spectrin-linked congenital hemolytic anemia. J Clin Invest. 2019; 129(7):2878–2887. PMID: 31038472.105. Richmond CM, Campbell S, Foo HW, Lunke S, Stark Z, Moody A, et al. Rapid identification of biallelic SPTB mutation in a neonate with severe congenital hemolytic anemia and liver failure. Mol Syndromol. 2020; 11(1):50–55. PMID: 32256302.106. Hall BJ, Reiter AJ, Englum BR, Rothman JA, Rice HE. Long-term hematologic and clinical outcomes of splenectomy in children with hereditary spherocytosis and sickle cell disease. Pediatr Blood Cancer. 2020; 67(8):e28290. PMID: 37132000.107. Chonat S, Risinger M, Sakthivel H, Niss O, Rothman JA, Hsieh L, et al. The spectrum of SPTA1-associated hereditary spherocytosis. Front Physiol. 2019; 10:815. PMID: 31333484.108. Rothman JA, Stevens JL, Gray FL, Kalfa TA. How I approach hereditary hemolytic anemia and splenectomy. Pediatr Blood Cancer. 2020; 67(11):e28337. PMID: 32391969.109. Iolascon A, Andolfo I, Barcellini W, Corcione F, Garçon L, De Franceschi L, et al. Recommendations regarding splenectomy in hereditary hemolytic anemias. Haematologica. 2017; 102(8):1304–1313. PMID: 28550188.110. Münch AL, Jacobsen EM, Schulz A, Loichinger W, Wowra T, Schiefele L, et al. Long-term haematological response and maintained immunological function after laparoscopic subtotal splenectomy in patients with hereditary spherocytosis. Eur J Haematol. 2023; 111(5):777–786. PMID: 37700575.