J Korean Med Sci.
2024 May;39(18):e158. 10.3346/jkms.2024.39.e158.
Impact of Comprehensive Primary Care in Patients With Complex Chronic Diseases: Nationwide Cohort Database Analysis in Korea
- Affiliations
-
- 1Department of Public Health, Graduate School of Korea University, Seoul, Korea
- 2Department of Health Administration, College of Nursing and Health, Kongju National University, Gongju, Korea
- 3Transdisciplinary Major in Learning Health Systems, Department of Healthcare Sciences, Graduate School, Korea University, Seoul, Korea
- 4Department of Preventive Medicine, Korea University College of Medicine, Seoul, Korea
- 5Institute for Future Public Health, Graduate School of Public Health, Korea University, Seoul, Korea
- KMID: 2555502
- DOI: http://doi.org/10.3346/jkms.2024.39.e158
Abstract
- Background
More comprehensive healthcare services should be provided to patients with complex chronic diseases to better manage their complex care needs. This study examined the effectiveness of comprehensive primary care in patients with complex chronic diseases.
Methods
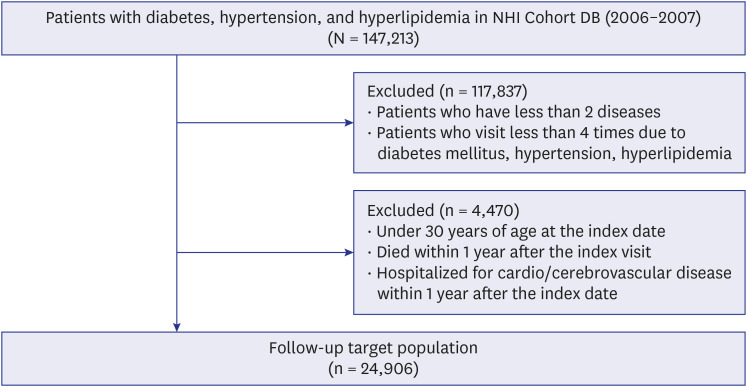
We obtained 2002–2019 data from the National Health Insurance Sample Cohort Database. Participants were individuals aged ≥ 30 years with at least two of the following diseases: hypertension, diabetes mellitus, and hyperlipidemia. Doctors’ offices were classified into specialized, functional, and gray-zone based on patient composition and major diagnostic categories. The Cox proportional hazard model was used to examine the association between office type and hospital admission due to all-causes, severe cardiovascular or cerebrovascular diseases (CVDs), hypertension, diabetes mellitus, or hyperlipidemia.
Results
The mean patient age was 60.3 years; 55.8% were females. Among the 24,906 patients, 12.8%, 38.3%, and 49.0% visited specialized, functional, and gray-zone offices, respectively. Patients visiting functional offices had a lower risk of all-cause admission (hazard ratio [HR], 0.935; 95% confidence interval [CI], 0.895–0.976) and CVD-related admission (HR, 0.908; 95% CI, 0.844–0.977) than those visiting specialized offices. However, the admission risks for hypertension, diabetes mellitus, and hyperlipidemia were not significantly different among office types.
Conclusion
This study provides evidence of the effectiveness of primary care in functional doctors’ offices for patients with complex chronic diseases beyond a single chronic disease and suggests the need for policies to strengthen functional offices providing comprehensive care.
Keyword
Figure
Reference
-
1. Sevick MA, Trauth JM, Ling BS, Anderson RT, Piatt GA, Kilbourne AM, et al. Patients with complex chronic diseases: perspectives on supporting self-management. J Gen Intern Med. 2007; 22 Suppl 3(Suppl 3):438–444. PMID: 18026814.2. Iglesias FH, Celada CA, Navarro CB, Morales LP, Visus NA, Valverde CC, et al. Complex care needs in multiple chronic conditions: population prevalence and characterization in primary care. A study protocol. Int J Integr Care. 2018; 18(2):16.3. Institute of Medicine. A Manpower Policy for Primary Health Care: Report of a Study. Washington, D.C., USA: National Academy Press;1978.4. O’Malley AS, Rich EC. Measuring comprehensiveness of primary care: challenges and opportunities. J Gen Intern Med. 2015; 30 Suppl 3(Suppl 3):S568–S575. PMID: 26105670.5. Starfield B. Is primary care essential? Lancet. 1994; 344(8930):1129–1133. PMID: 7934497.6. Yun JM, Choi S, Cho Y, Park SM, Kim Y. Definition and status of functional primary clinic in Korea. Korean J Fam Pract. 2021; 11(1):3–9.7. Lee JY, Eun SJ, Ock M, Kim HJ, Lee HJ, Son WS, et al. General internists’ perspectives regarding primary care and currently related issues in Korea. J Korean Med Sci. 2015; 30(5):523–532. PMID: 25931781.8. Ock M, Kim JE, Jo MW, Lee HJ, Kim HJ, Lee JY. Perceptions of primary care in Korea: a comparison of patient and physician focus group discussions. BMC Fam Pract. 2014; 15(1):178. PMID: 25358391.9. Lee JH, Choi YJ, Volk RJ, Kim SY, Kim YS, Park HK, et al. Defining the concept of primary care in South Korea using a Delphi method. Fam Med. 2007; 39(6):425–431. PMID: 17549652.10. Bindman AB, Forrest CB, Britt H, Crampton P, Majeed A. Diagnostic scope of and exposure to primary care physicians in Australia, New Zealand, and the United States: cross sectional analysis of results from three national surveys. BMJ. 2007; 334(7606):1261. PMID: 17504790.11. Lee JY, Eun SJ, Kim HJ, Jo MW. Finding the primary care providers in the specialist-dominant primary care setting of Korea: a cluster analysis. PLoS One. 2016; 11(8):e0161937. PMID: 27560181.12. Kim HJ, Shin JY, Yang YJ, Cho B, Yun JM. Analysis of the comprehensiveness of primary care clinics in Korea. Korean J Fam Med. 2021; 42(1):47–52. PMID: 32418395.13. Alazri M, Heywood P, Neal RD, Leese B. Continuity of care: literature review and implications. Sultan Qaboos Univ Med J. 2007; 7(3):197–206. PMID: 21748104.14. Dickinson WP, Miller BF. Comprehensiveness and continuity of care and the inseparability of mental and behavioral health from the patient-centered medical home. Fam Syst Health. 2010; 28(4):348–355. PMID: 21299281.15. Tammes P, Purdy S, Salisbury C, MacKichan F, Lasserson D, Morris RW. Continuity of primary care and emergency hospital admissions among older patients in England. Ann Fam Med. 2017; 15(6):515–522. PMID: 29133489.16. Nyweide DJ, Bynum JP. Relationship between continuity of ambulatory care and risk of emergency department episodes among older adults. Ann Emerg Med. 2017; 69(4):407–415.e3. PMID: 27520592.17. van Loenen T, van den Berg MJ, Westert GP, Faber MJ. Organizational aspects of primary care related to avoidable hospitalization: a systematic review. Fam Pract. 2014; 31(5):502–516. PMID: 25216664.18. van Walraven C, Oake N, Jennings A, Forster AJ. The association between continuity of care and outcomes: a systematic and critical review. J Eval Clin Pract. 2010; 16(5):947–956. PMID: 20553366.19. Hussey PS, Schneider EC, Rudin RS, Fox DS, Lai J, Pollack CE. Continuity and the costs of care for chronic disease. JAMA Intern Med. 2014; 174(5):742–748. PMID: 24638880.20. Lee A, Kiyu A, Milman HM, Jimenez J. Improving health and building human capital through an effective primary care system. J Urban Health. 2007; 84(3):Suppl. i75–i85. PMID: 17356902.21. Kim JA, Yoon S, Kim LY, Kim DS. Towards actualizing the value potential of Korea Health Insurance Review and Assessment (HIRA) data as a resource for health research: strengths, limitations, applications, and strategies for optimal use of HIRA data. J Korean Med Sci. 2017; 32(5):718–728. PMID: 28378543.22. Sung NJ, Choi YJ, Lee JH. Primary care comprehensiveness can reduce emergency department visits and hospitalization in people with hypertension in South Korea. Int J Environ Res Public Health. 2018; 15(2):272. PMID: 29401740.23. O’Malley AS, Rich EC, Shang L, Rose T, Ghosh A, Poznyak D, et al. Practice-site-level measures of primary care comprehensiveness and their associations with patient outcomes. Health Serv Res. 2021; 56(3):371–377. PMID: 33197047.24. Henry TL, Petterson S, Phillips RS, Phillips RL Jr, Bazemore A. Comparing comprehensiveness in primary care specialties and their effects on healthcare costs and hospitalizations in Medicare beneficiaries. J Gen Intern Med. 2019; 34(12):2708–2710. PMID: 31520228.25. Bazemore A, Petterson S, Peterson LE, Phillips RL Jr. More comprehensive care among family physicians is associated with lower costs and fewer hospitalizations. Ann Fam Med. 2015; 13(3):206–213. PMID: 25964397.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Expansion of a food composition database for the food frequency questionnaire in the Korean Genome and Epidemiology Study (KoGES): a comprehensive database of dietary antioxidants and total antioxidant capacity
- Impact of a Primary Health Care Chronic Diseases Management Pilot Program
- Review the Change of Chronic Disease Care in Korea
- Time to establish multidisciplinary childhood cancer survivorship programs in Korea
- Risk of chronic periodontitis in patients with obstructive sleep apnea in Korea: a nationwide retrospective cohort study