J Korean Med Sci.
2024 May;39(17):e152. 10.3346/jkms.2024.39.e152.
Shifts in Clinical Characteristics, Treatment, and Outcome for Rheumatic Mitral Stenosis: Insights From a 20-Year Multicentre Registry Study in Korea
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea
- 2Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea
- 3Division of Cardiology, Department of Internal Medicine, Inha University College of Medicine, Incheon, Korea
- 4Division of Cardiology, Yeungnam University Medical Center, Daegu, Korea
- 5Division of Cardiology, Department of Internal Medicine, Inje University Ilsan Paik Hospital, Goyang, Korea
- 6Division of Cardiology, Gachon University Gil Medical Center, Incheon, Korea
- 7Department of Internal Medicine, Yonsei University Gangnam Severance Hospital, Seoul, Korea
- 8Division of Physiology, Department of Biomedical Laboratory, Daegu Health College, Daegu, Korea
- 9University of Texas Health, Houston, TX, USA
- KMID: 2555496
- DOI: http://doi.org/10.3346/jkms.2024.39.e152
Abstract
- Background
The rapid economic development of South Korea provides a unique model to study changes in the clinical characteristics, treatment approaches, and clinical outcomes of patients with rheumatic mitral stenosis (MS) relative to socioeconomic growth.
Methods
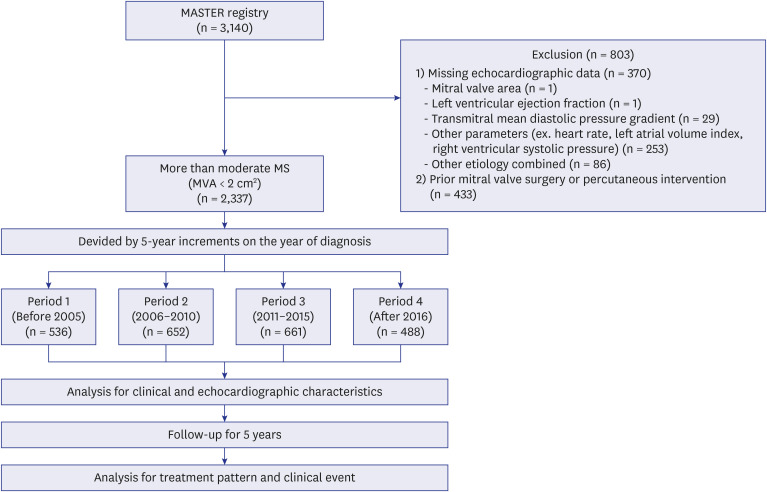
From the Multicenter mitrAl STEnosis with Rheumatic etiology (MASTER) registry, 2,337 patients diagnosed with moderate or severe rheumatic MS between January 2001 and December 2020 were analyzed. Patients were grouped into consecutive 5-year intervals based on their year of diagnosis. Clinical characteristics, echocardiographic data, and clinical outcomes were assessed.
Results
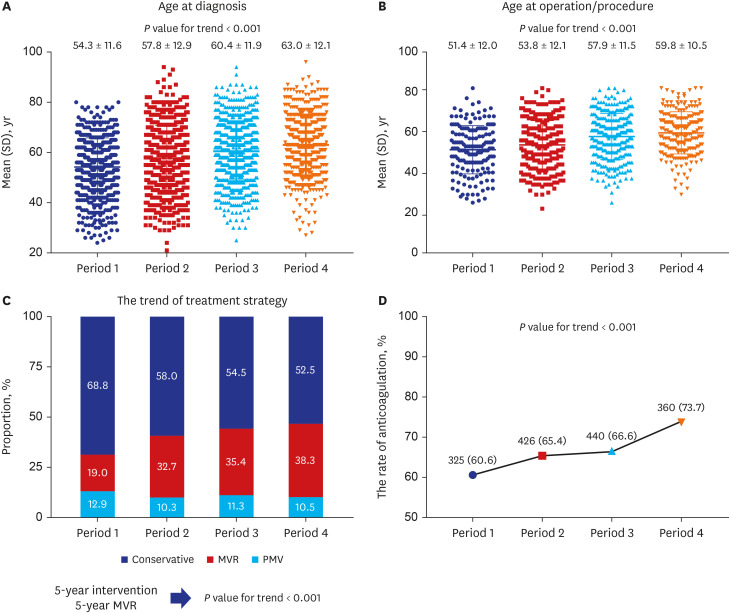
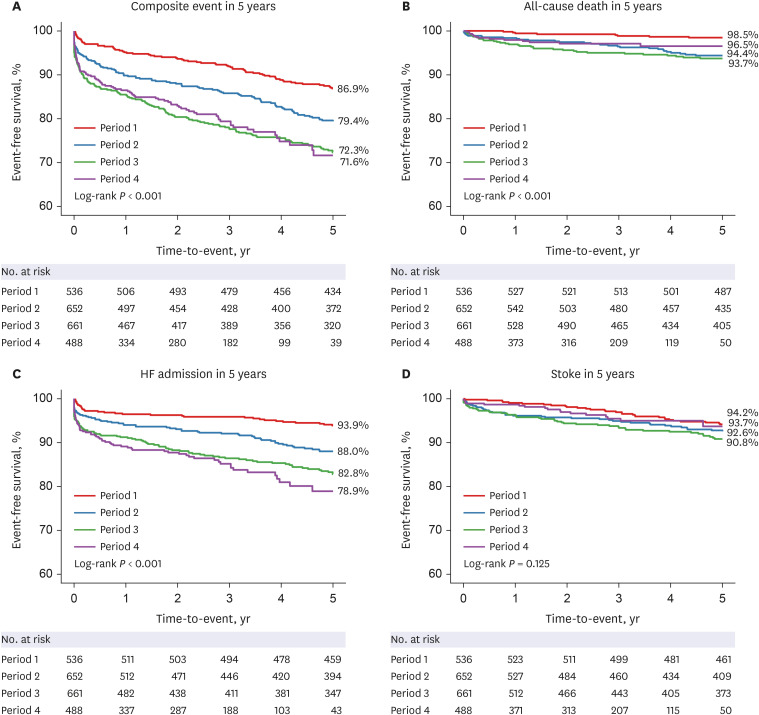
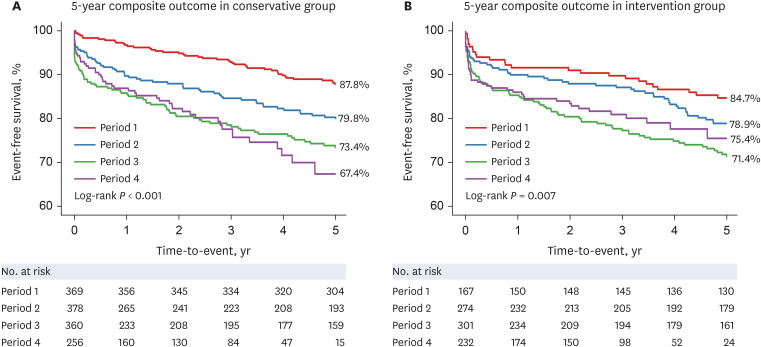
Over 20 years, the severity of mitral stenosis increased from 79.1% to 90.2%; similarly, the average age at diagnosis increased from 54.3 to 63.0 years (all P < 0.001). Comorbidities such as hypertension and atrial fibrillation increased (6.3% to 29.5% and 41.4% to 46.9%, respectively; all P for trend < 0.05). The rate of mitral intervention within five years after diagnosis increased from 31.2% to 47.4% (P for trend < 0.001). However, clinical outcomes of rheumatic mitral stenosis deteriorated over time in the composite outcomes (log-rank test, P < 0.001). Conversely, the incidence of stroke remained stable (60.6–73.7%; P < 0.001), which might be attributed to the increased use of anticoagulation therapy.
Conclusion
This study observed an increase in patient age, comorbidities, and valve disease severity as the country transitioned from a developing to developed status. Despite a rise in mitral valve interventions, clinical outcomes deteriorated over 20 years, highlighting the need for modified treatment approaches to improve patient outcomes.
Figure
Reference
-
1. Carapetis JR, Steer AC, Mulholland EK, Weber M. The global burden of group A streptococcal diseases. Lancet Infect Dis. 2005; 5(11):685–694. PMID: 16253886.2. Watkins DA, Johnson CO, Colquhoun SM, Karthikeyan G, Beaton A, Bukhman G, et al. Global, regional, and national burden of rheumatic heart disease, 1990-2015. N Engl J Med. 2017; 377(8):713–722. PMID: 28834488.3. Marijon E, Mirabel M, Celermajer DS, Jouven X. Rheumatic heart disease. Lancet. 2012; 379(9819):953–964. PMID: 22405798.4. Sims Sanyahumbi A, Colquhoun S, Wyber R, Carapetis JR. Global disease burden of group A streptococcus. Ferretti JJ, Stevens DL, Fischetti VA, editors. Streptococcus Pyogenes: Basic Biology to Clinical Manifestations. Oklahoma City, OK, USA: University of Oklahoma Health Sciences Center;2016.5. Seo HY, Yoon SJ, Kim EJ, Oh IH, Lee YH, Kim YA. The economic burden of rheumatic heart disease in South Korea. Rheumatol Int. 2013; 33(6):1505–1510. PMID: 23239034.6. Kim JY, Kim SH, Myong JP, Choi Y, Hwang YM, Kim TS, et al. Ten-year trends in the incidence, treatment and outcomes of patients with mitral stenosis in Korea. Heart. 2020; 106(10):746–750. PMID: 32029525.7. Olesen KH. The natural history of 271 patients with mitral stenosis under medical treatment. Br Heart J. 1962; 24(3):349–357. PMID: 14481743.8. Chung SH, Lee HJ, Kim HS, Oh JY. Health insurance benefit criteria and quality assurance policies of diagnostic ultrasound services in other countries. Health Policy Manag. 2014; 24(2):109–119.9. Kwon S. Thirty years of national health insurance in South Korea: lessons for achieving universal health care coverage. Health Policy Plan. 2009; 24(1):63–71. PMID: 19004861.10. Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2015; 16(3):233–270. PMID: 25712077.11. Reményi B, Wilson N, Steer A, Ferreira B, Kado J, Kumar K, et al. World Heart Federation criteria for echocardiographic diagnosis of rheumatic heart disease--an evidence-based guideline. Nat Rev Cardiol. 2012; 9(5):297–309. PMID: 22371105.12. Silbiger JJ. Advances in rheumatic mitral stenosis: echocardiographic, pathophysiologic, and hemodynamic considerations. J Am Soc Echocardiogr. 2021; 34(7):709–722.e1. PMID: 33652082.13. Baumgartner H, Hung J, Bermejo J, Chambers JB, Evangelista A, Griffin BP, et al. Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. J Am Soc Echocardiogr. 2009; 22(1):1–23. PMID: 19130998.14. Gordis L. The virtual disappearance of rheumatic fever in the United States: lessons in the rise and fall of disease. T. Duckett Jones memorial lecture. Circulation. 1985; 72(6):1155–1162. PMID: 4064266.15. Kawano H, Hisaoka T, Okada R. Chronological changes in the annual incidence of valvular heart disease based on autopsies performed in Japan. J Cardiol. 1993; 23(4):359–363. PMID: 8064585.16. Antunes MJ. The global burden of rheumatic heart disease: population-related differences (It is not all the same!). Rev Bras Cir Cardiovasc. 2020; 35(6):958–963.17. Xu H, Liu Q, Cao K, Ye Y, Zhang B, Li Z, et al. Distribution, characteristics, and management of older patients with valvular heart disease in China: China-DVD study. JACC Asia. 2022; 2(3):354–365. PMID: 36338396.18. GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease study 2019. Lancet. 2020; 396(10258):1204–1222. PMID: 33069326.19. Ghamari SH, Abbasi-Kangevari M, Saeedi Moghaddam S, Aminorroaya A, Rezaei N, Shobeiri P, et al. Rheumatic heart disease is a neglected disease relative to its burden worldwide: findings from Global Burden of Disease 2019. J Am Heart Assoc. 2022; 11(13):e025284. PMID: 35730651.20. Kim K, Kim DY, Seo J, Cho I, Hong GR, Ha JW, et al. Temporal trends in diagnosis, treatments, and outcomes in patients with bicuspid aortic valve. Front Cardiovasc Med. 2021; 8:766430. PMID: 34805321.21. Sun BJ, Oh JK, Lee SH, Jang JY, Lee JH, Lee S, et al. Mid-term clinical outcomes in a cohort of asymptomatic or mildly symptomatic Korean patients with bicuspid aortic valve in a tertiary referral hospital. J Cardiovasc Imaging. 2019; 27(2):105–118. PMID: 30993945.22. Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2022; 43(7):561–632. PMID: 34453165.23. Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021; 143(5):e72–227. PMID: 33332150.24. Kim DY, Cho I, Kim K, Gwak SY, Ha KE, Lee HJ, et al. Outcomes of severe mitral stenosis with the revised severity criteria: mitral valve replacement vs percutaneous mitral valvuloplasty. Can J Cardiol. 2024; 40(1):100–109. PMID: 37716640.25. Choi JW, Kim JB, Jung YJ, Hwang HY, Kim KH, Yoo JS, et al. Trends in heart valve surgery in Korea: a report from the Heart Valve Surgery Registry Database. J Chest Surg. 2022; 55(5):388–396. PMID: 35999692.26. Badheka AO, Shah N, Ghatak A, Patel NJ, Chothani A, Mehta K, et al. Balloon mitral valvuloplasty in the United States: a 13-year perspective. Am J Med. 2014; 127(11):1126.e1–1126.12.27. El Sabbagh A, Reddy YN, Barros-Gomes S, Borlaug BA, Miranda WR, Pislaru SV, et al. Low-gradient severe mitral stenosis: hemodynamic profiles, clinical characteristics, and outcomes. J Am Heart Assoc. 2019; 8(5):e010736. PMID: 30793648.28. Cho IJ, Hong GR, Lee SH, Lee S, Chang BC, Shim CY, et al. Differences in characteristics, left atrial reverse remodeling, and functional outcomes after mitral valve replacement in patients with low-gradient very severe mitral stenosis. J Am Soc Echocardiogr. 2016; 29(8):759–767. PMID: 27106010.29. Hensey M, Brown RA, Lal S, Sathananthan J, Ye J, Cheung A, et al. Transcatheter mitral valve replacement: an update on current techniques, technologies, and future directions. JACC Cardiovasc Interv. 2021; 14(5):489–500. PMID: 33663778.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Giant Left Atrium in Rheumatic Mitral Stenosis
- Noninvasive Evaluation of Rheumatic Tricuspid Stenosis with Doppler and 2 Dimensional Echocardiography
- Rheumatic Carditis Associated with Mitral Stenosis
- Basal Interventricular Septal Aneurysm in Rheumatic Mitral Stenosis
- Partial Anomalous Pulmonary Venous Return via a Levoatriocardinal Vein in Association with Rheumatic Mitral Stenosis: MR Demonstration and Successful Surgical Repair