J Korean Med Sci.
2024 Apr;39(15):e147. 10.3346/jkms.2024.39.e147.
Comprehensive Guidance for the Prevention of Periprosthetic Joint Infection After Total Joint Arthroplasty and Pitfalls in the Prevention
- Affiliations
-
- 1International Joint Center, Acibadem University Hospital, Istanbul, Turkey
- 2Rothman Orthopaedic Institute at Thomas Jefferson University, Philadelphia, PA, USA
- 3Department of Orthopedic Surgery, Daejeon Eulji Medical Center, Eulji University School of Medicine, Daejeon, Korea
- 4Kay Joint Center at Cheil Orthopaedic Hospital, Seoul, Korea
- 5Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2555475
- DOI: http://doi.org/10.3346/jkms.2024.39.e147
Abstract
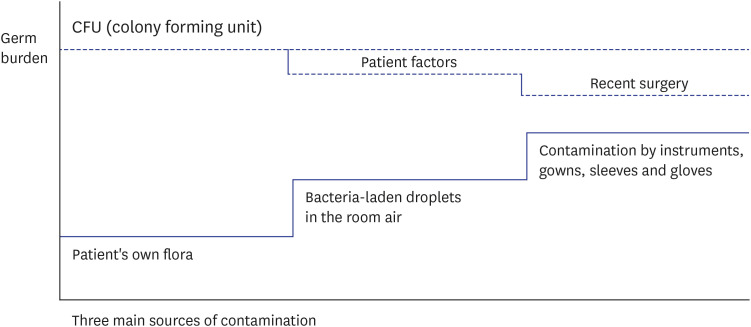
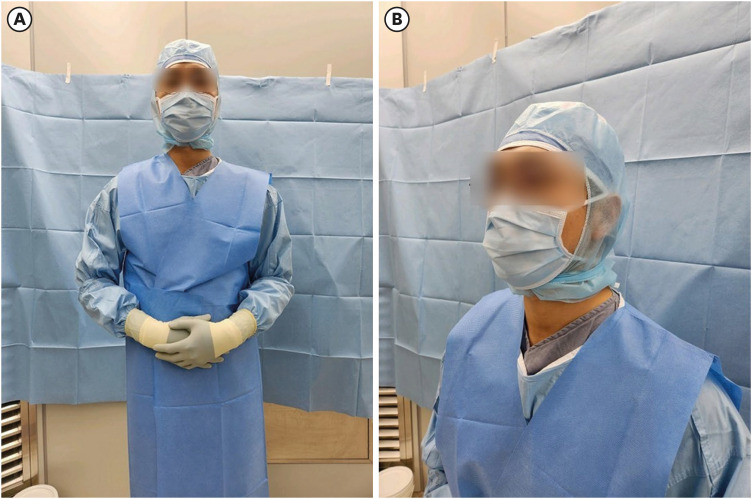
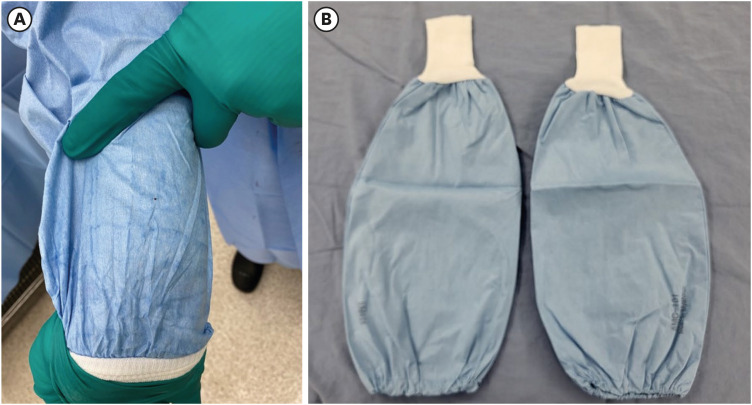
- Total joint arthroplasty (TJA) is a surgical procedure, in which parts of damaged joints are removed and replaced with a prosthesis. The main indication of TJA is osteoarthritis, and the volume of TJA is rising annually along with the increase of aged population. Hip and knee are the most common joints, in which TJAs are performed. The TJA prosthesis is composed of metal, plastic, or ceramic device. Even though TJA is the most successful treatment for end-stage osteoarthritis, it is associated with various complications, and periprosthetic joint infection (PJI) is the most serious complication after TJA. With the increasing volume of TJAs, there is a simultaneous rise in the incidence of PJI. Contamination of the surgical wound and the adherence of bacteria to the surface of prosthetic component represent the initial step in the pathogenesis of PJI. The main sources of the contamination are 1) patient's own flora, 2) droplets in the operation room air, and 3) surgical gloves and instruments. Even though modern techniques have markedly reduced the degree of contamination, TJAs cannot be done in completely germ-free conditions and some degree of contamination is inevitable in all surgical procedures. However, not all contamination leads to PJI. It develops when the burden of contamination exceeds the immune threshold or the colony forming units (CFUs) and various factors contribute to a decrease in the CFU level. Surgeons should be aware of the germ burden/CFU concept and should monitor sources of contamination to maintain the germ burden below the CFU to prevent PJI.
Keyword
Figure
Reference
-
1. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007; 89(4):780–785. PMID: 17403800.2. Tande AJ, Patel R. Prosthetic joint infection. Clin Microbiol Rev. 2014; 27(2):302–345. PMID: 24696437.3. Kim HS, Lee YK, Won SJ, Park SJ, Park JW, Koo KH. Effectiveness of online video instruction on time to start ambulation and duration of hospital stay, satisfaction and functional recovery in patients undergoing total hip arthroplasty. J Korean Med Sci. 2022; 37(2):e7. PMID: 35014223.4. Yoo JI, Cha Y, Lee YK, Ha YC, Koo KH. Do cementless short tapered stems reduce the incidence of thigh pain after hip arthroplasty? Systematic review and meta-analysis. J Korean Med Sci. 2022; 37(6):e41. PMID: 35166078.5. Kim HS, Park JW, Moon SY, Lee YK, Ha YC, Koo KH. Current and future burden of periprosthetic joint infection from national claim database. J Korean Med Sci. 2020; 35(49):e410. PMID: 33350183.6. AlBuhairan B, Hind D, Hutchinson A. Antibiotic prophylaxis for wound infections in total joint arthroplasty: a systematic review. J Bone Joint Surg Br. 2008; 90(7):915–919. PMID: 18591602.7. Kim SH, Jang SY, Cha Y, Kim BY, Lee HJ, Kim GO. How does medical policy on the use of prophylactic antibiotics affect medical costs, length of hospital stay, and antibiotic use in orthopedics? Yonsei Med J. 2023; 64(3):213–220. PMID: 36825348.8. Hambraeus A. Aerobiology in the operating room--a review. J Hosp Infect. 1988; 11(Suppl A):68–76.9. Parvizi J, Pawasarat IM, Azzam KA, Joshi A, Hansen EN, Bozic KJ. Periprosthetic joint infection: the economic impact of methicillin-resistant infections. J Arthroplasty. 2010; 25(6):Suppl. 103–107. PMID: 20570103.10. Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, et al. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res. 2010; 468(1):45–51. PMID: 19554385.11. Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infections. N Engl J Med. 2004; 351(16):1645–1654. PMID: 15483283.12. Aggarwal VK, Rasouli MR, Parvizi J. Periprosthetic joint infection: current concept. Indian J Orthop. 2013; 47(1):10–17. PMID: 23531512.13. Kapadia BH, Berg RA, Daley JA, Fritz J, Bhave A, Mont MA. Periprosthetic joint infection. Lancet. 2016; 387(10016):386–394. PMID: 26135702.14. Prokuski L, Clyburn TA, Evans RP, Moucha CS. Prophylactic antibiotics in orthopaedic surgery. Instr Course Lect. 2011; 60:545–555. PMID: 21553797.15. Charnley J. A sterile-air operating theatre enclosure. Br J Surg. 1964; 51(3):195–202. PMID: 14129433.16. Wendlandt R, Thomas M, Kienast B, Schulz AP. In-vitro evaluation of surgical helmet systems for protecting surgeons from droplets generated during orthopaedic procedures. J Hosp Infect. 2016; 94(1):75–79. PMID: 27238610.17. Young SW, Zhu M, Shirley OC, Wu Q, Spangehl MJ. Do ‘Surgical Helmet Systems’ or ‘Body Exhaust Suits’ affect contamination and deep infection rates in arthroplasty? A systematic review. J Arthroplasty. 2016; 31(1):225–233. PMID: 26321627.18. Vijaysegaran P, Knibbs LD, Morawska L, Crawford RW. Surgical space suits increase particle and microbiological emission rates in a simulated surgical environment. J Arthroplasty. 2018; 33(5):1524–1529. PMID: 29317156.19. Koster R, van Wezel RAC, van Doornmalen JPCM. Parametric release with measurements of steam sterilisation parameters: temperature, steam composition and time. Aseptica. Updated 2022. Accessed March 27, 2024. https://www.ebro.com/fileadmin/pics/Pressebericht/Ausgabe_1_2022_GB.pdf#page=15 .20. Blom AW, Barnett A, Ajitsaria P, Noel A, Estela CM. Resistance of disposable drapes to bacterial penetration. J Orthop Surg (Hong Kong). 2007; 15(3):267–269. PMID: 18162666.21. Kunutsor SK, Whitehouse MR, Blom AW, Beswick AD. INFORM Team. Patient-related risk factors for periprosthetic joint infection after total joint arthroplasty: a systematic review and meta-analysis. PLoS One. 2016; 11(3):e0150866. PMID: 26938768.22. Moon YW, Kim YS, Kwon SY, Kim SY, Lim SJ, Park YS. Perioperative risk of hip arthroplasty in patients with cirrhotic liver disease. J Korean Med Sci. 2007; 22(2):223–226. PMID: 17449928.23. Forlenza EM, Burnett RA, Korrapati A, Yang J, Forsythe B, Della Valle CJ. Preoperative corticosteroid injections demonstrate a temporal and dose-dependent relationship with the rate of postoperative infection following total hip arthroplasty. J Arthroplasty. 2021; 36(6):2033–2037.e1. PMID: 33618958.24. Chambers AW, Lacy KW, Liow MH, Manalo JP, Freiberg AA, Kwon YM. Multiple hip intra-articular steroid injections increase risk of periprosthetic joint infection compared with single injections. J Arthroplasty. 2017; 32(6):1980–1983. PMID: 28237216.25. Silva M, Tharani R, Schmalzried TP. Results of direct exchange or debridement of the infected total knee arthroplasty. Clin Orthop Relat Res. 2002; 404:125–131.26. Romanò CL, Manzi G, Logoluso N, Romanò D. Value of debridement and irrigation for the treatment of peri-prosthetic infections. A systematic review. Hip Int. 2012; 22(Suppl 8):S19–S24. PMID: 22956381.27. Bejon P, Berendt A, Atkins BL, Green N, Parry H, Masters S, et al. Two-stage revision for prosthetic joint infection: predictors of outcome and the role of reimplantation microbiology. J Antimicrob Chemother. 2010; 65(3):569–575. PMID: 20053693.28. Mahmud T, Lyons MC, Naudie DD, Macdonald SJ, McCalden RW. Assessing the gold standard: a review of 253 two-stage revisions for infected TKA. Clin Orthop Relat Res. 2012; 470(10):2730–2736. PMID: 22538959.29. Falahee MH, Matthews LS, Kaufer H. Resection arthroplasty as a salvage procedure for a knee with infection after a total arthroplasty. J Bone Joint Surg Am. 1987; 69(7):1013–1021. PMID: 3654692.30. Longo UG, De Salvatore S, Bandini B, Lalli A, Barillà B, Budhiparama NC, et al. Debridement, antibiotics, and implant retention (DAIR) for the early prosthetic joint infection of total knee and hip arthroplasties: a systematic review. J ISAKOS. 2024; 9(1):62–70. PMID: 37714518.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Three Concurrent Periprosthetic Joint Infections: A Case Report and Literature Review
- Economic Burden of Periprosthetic Joint Infection Following Primary Total Knee Replacement in a Developing Country
- Evidence-based Approach for Prevention of Surgical Site Infection
- Three Staged Revision Arthroplasty Using Structural Allograft in Chronic Periprosthetic Joint Infection Accompanied by Fracture: A Case Report
- Management of Periprosthetic Joint Infection